Published online May 27, 2010. doi: 10.4254/wjh.v2.i5.201
Revised: March 30, 2010
Accepted: April 6, 2010
Published online: May 27, 2010
A 60-year-old male underwent orthotopic liver transplantation because of hepatitis C virus related cirrhosis. After 12 d, the patient underwent re-transplantation due to primary graft non function. One year later the patient developed a thrombosis of the main portal vein needing a surgical revision. After 11 years the patient was operated on because of a clinical picture of intestinal occlusion. As an incidental finding, a large aneurysm of the main portal vein was diagnosed. The incidence of intra- and extrahepatic Portal vein aneurysms (PVAs) is not clear. To the best of our knowledge, only one case of intrahepatic PVA in a liver transplant has been reported in the literature. In addition, we have found no documented cases of extrahepatic PVAs in liver transplanted patients.
- Citation: Francesco FD, Gruttadauria S, Caruso S, Gridelli B. Huge extrahepatic portal vein aneurysm as a late complication of liver transplantation. World J Hepatol 2010; 2(5): 201-202
- URL: https://www.wjgnet.com/1948-5182/full/v2/i5/201.htm
- DOI: https://dx.doi.org/10.4254/wjh.v2.i5.201
A 60-year-old male underwent orthotopic liver transplantation in Cambridge, England in 1993, because of hepatitis C virus related cirrhosis. After 12 d, the patient underwent re-transplantation due to primary graft non function. In 1994, a thrombosis of the main portal vein (MPV) was detected. As a result, the patient underwent surgical reconstruction (there were no medical records or details of the previous surgery in the patient’s possession). From 1994 to 2003, the patient showed no liver function alterations. However, liver ultrasound (US) performed during follow-up showed a slow dimensional increase of the MPV (16 mm in December 1994, 18 mm in 1996, 25 mm in 2002, and 30 mm in 2003).
The patient did not undergo any other radiological examinations at any time. In June 2003, the patient was admitted to another hospital for acute intestinal occlusion, with abdominal pain and vomiting. The patient underwent explorative laparotomy with adhesiolisis. At that time no aneurysm of the portal vein was diagnosed or detected.
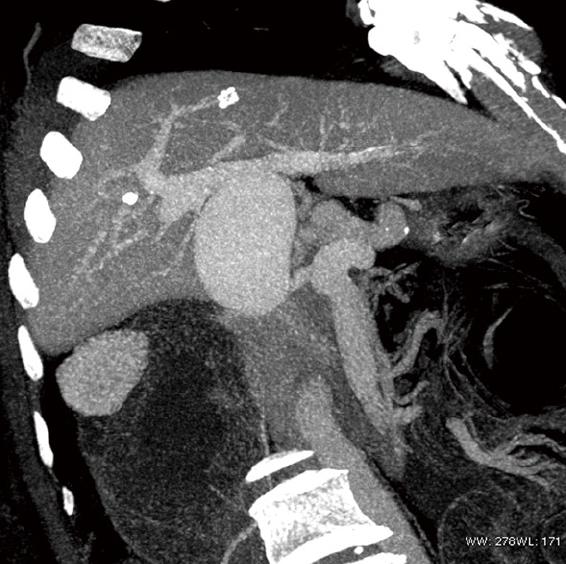
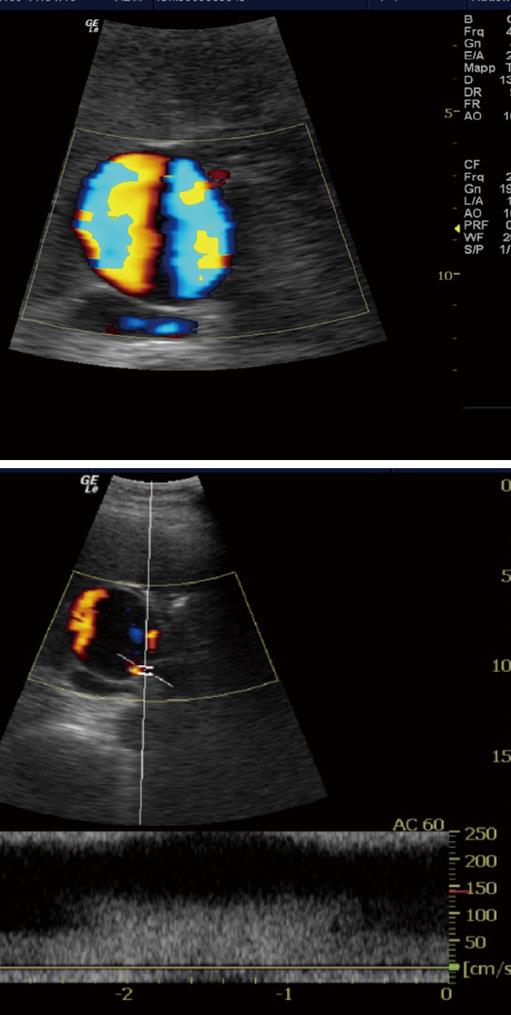
In July 2003, the patient was admitted to our center with a clinical picture of intestinal occlusion. 64 Multi Detector CT scan (Lightspeed VCT, GE) performed with and without contrast media showed an overdistension of the small bowel and right colon in the presence of a severe neoplastic lesion occluding the transverse colon. A colonscopy confirmed the lesion, which was also biopsy proven. As an incidental finding, a large aneurysm of the MPV, 6.5 cm in diameter and arising 1 cm after the spleno-mesenteric confluence, was found (Figure 1). The patient underwent surgery for colon resection; the presence of tenacious adherences made it impossible to check the portal vein situation. A mild amount of ascites and splenomegaly was detected (longitudinal diameter of 16.3 cm) with no other radiological signs of portal hypertension. At that time liver function tests were normal. Doppler US showed increased velocity near the origin of the aneurysm, and turbulent flow inside. Monophasic flow with normal velocity was detected in the intrahepatic portal branches (Figure 2).
Extrahepatic portal vein aneurysms, defined as MPV greater than 1.9 cm, are rare in non-transplanted patients and in cirrhotic patients, and only 67 cases have been documented, in the English literature. Portal vein aneurysms (PVAs) can be congenital or acquired, and even if the etiology remains unclear, there are some related conditions, such as portal hypertension, pancreatitis or trauma.
PVAs are usually asymptomatic[1-3] if small, while large PVAs can cause biliary tract obstruction, chronic portal hypertension, portal vein thrombosis, acute portal hypertension, abdominal discomfort and, though rarely, adjacent structure compression and rupture.
Our patient showed no symptoms or complications related to the aneurysm that justified surgical treatment. The patient was followed with Doppler US every three months.
The incidence of intra- and extrahepatic PVAs is not clear. To the best of our knowledge, only one case of intrahepatic PVA in a liver transplant has been reported in the literature[4]. In addition, we have found no documented cases of extrahepatic PVAs in liver transplanted patients. We believe that in our case, one or more of the three surgical interventions on the portal vein, created a weak point in the portal vein which was responsible, over a period of years, for the development of the aneurysm. In addition, at the time of the colon resection surgery, the intestinal occlusion could have increased the intra-abdominal pressure and consequently the portal pressure, leading to the enlargement of the portal aneurysm.
Peer reviewers: Lars Müller, MD, Consultant, Department of General and Thoracic Surgery, University Hospital of Schleswig-Holstein, Campus Kiel, Arnold-Heller-Str. 3, Kiel 24105, Germany; Boon Hun Yong, Associate Professor, Department of Anaesthesiology, University of Hong Kong, Hong Kong, China
| 1. | Gallego C, Velasco M, Marcuello P, Tejedor D, De Campo L, Friera A. Congenital and acquired anomalies of the portal venous system. Radiographics. 2002;22:141-159. |
| 2. | Koc Z, Oguzkurt L, Ulusan S. Portal venous system aneurysms: imaging, clinical findings, and a possible new etiologic factor. AJR. 2007;189:1023-1030. |
| 3. | Miyazaki K, Takatsuki M, Eguchi S, Hidaka M, Tokai H, Hamasaki K, Tajima Y, Kanematsu T. Living donor liver transplantation for hepatitis C virus cirrhosis with a huge portal vein aneurysm. Liver Transpl. 2008;14:1221-1222. |
| 4. | Ferraz-Neto BH, Sakabe D, Buttros DA, Resende MB, Afonso RC. Portal vein aneurysm as late complication of liver transplantation: a case report. Transplant Proc. 2004;36:970-971. |