Published online May 27, 2010. doi: 10.4254/wjh.v2.i5.198
Revised: April 15, 2010
Accepted: April 22, 2010
Published online: May 27, 2010
A 66-year-old female with cryptogenic cirrhosis complicated by ascites, hepatic encephalopathy, variceal bleeding and malnutrition with MELD of 34 underwent orthotopic deceased donor liver transplantation performed with piggyback technique. Extensive eversion thromboendovenectomy was performed for a portal vein thrombus which resulted in an excellent portal vein flow. The liver graft was recirculated without any hemodynamic instability. Subsequently, the patient became hypotensive progressing to asystole. She was resuscitated and a transesophageal probe was inserted which revealed a mobile right atrial thrombus and an underfilled poorly contractile right ventricle. The patient was noted to be coagulopathic at the time. She became progressively more stable with a TEE showing complete resolution of the intracardiac thrombus.
- Citation: Sibulesky L, Peiris P, Taner CB, Kramer DJ, Canabal JM, Nguyen JH. Intraoperative intracardiac thrombosis in a liver transplant patient. World J Hepatol 2010; 2(5): 198-200
- URL: https://www.wjgnet.com/1948-5182/full/v2/i5/198.htm
- DOI: https://dx.doi.org/10.4254/wjh.v2.i5.198
Intracardiac thrombosis (ICT) during orthtopic liver transplantation is a catastrophic complication that carries a very high mortality. The exact cause of this condition is not known but it appears that it has multiple etiologies including administration of antifibrinolytic drugs intraoperatively and venovenous bypass.
In this case report we describe a patient who developed ICT during orthotopic liver transplantation. No risk factors could be identified.
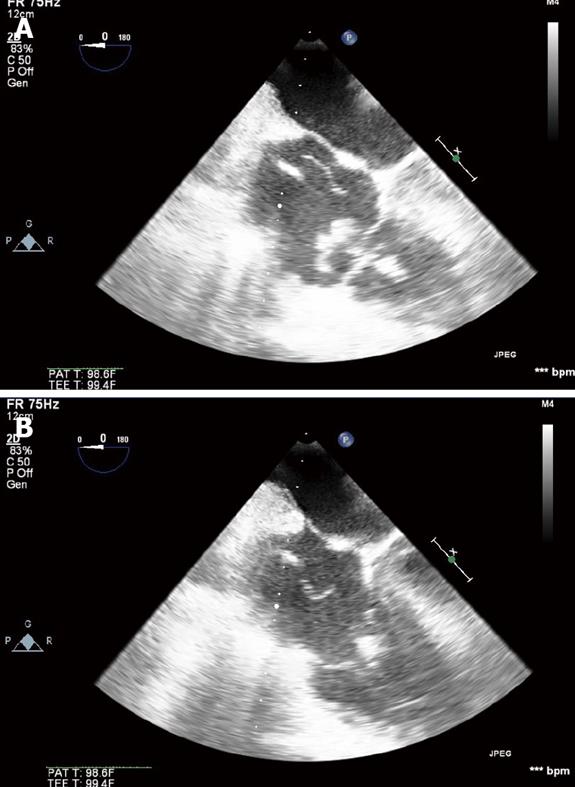
A 66-year-old female with cryptogenic cirrhosis was admitted to our Intensive Care Unit (ICU) with acutely worsening liver function. She had had multiple operations in the past including open cholecystectomy, total abdominal hysterectomy with salpingo-oophorectomy and appendectomy. She was noted to have a nodular liver while undergoing laparotomy for lysis of adhesions in 2007. Her liver disease was complicated by ascites, hepatic encephalopathy, variceal bleeding and malnutrition. She was on continuous venovenous hemofiltration for renal dysfunction. Her MELD was 34. A contrast-enhanced CT revealed a cirrhotic liver with thrombus in the portal vein extending into the superior mesenteric and splenic veins. The patient did not have any known hypercoagulable disorder and the thrombus in the portal vein was attributed to her liver disease. She was treated in the ICU for 15 d when an organ became available. The orthotopic deceased donor liver transplantation was performed with piggyback technique. Extensive eversion thromboendovenectomy resulted in an excellent portal vein flow. The liver graft was recirculated after the hepatic and portal vein anastomoses were completed. The patient tolerated recirculation well without any hemodynamic instability. While the hepatic artery was dissected and mobilized for the arterial anastomosis, the patient became acutely hypotensive progressing to asystole. She was resuscitated with external cardiac massage and inotropic support. A transesophageal echocardiography (TEE) probe was emergently inserted and showed mobile right atrial thrombus and an underfilled, poorly contractile right ventricle (Figure 1A). At the time of resuscitation, INR was 6.4, fibrinogen < 25 mg/dL and platelets 13 000/μL (Table 1). No antifibrinolytic therapy was administered. Continued monitoring by TEE showed the clot adherent to the tricuspid valve (Figure 1B) and later was not seen on four chamber view indicating either spontaneous thrombolysis or propagation into the pulmonary vasculature. The right ventricular function and filling improved and the patient became hemodynamically more stable, allowing successful completion of the liver transplantation. The patient was transferred to the ICU for postoperative care on dopamine drip (10 mcg/kg per minute). The patient was weaned off pressors on POD zero and was successfully extubated on POD two. An echocardiogram performed on POD two demonstrated normal right and left ventricular size and function with ejection fraction of 57%. There was no evidence of intracardiac thrombus. The postoperative ultrasound of the liver graft revealed widely patent hepatic veins, hepatic artery and portal vein with normal flows. Ultrasound of the extremities was negative for deep vein thrombosis. The patient currently has normal liver function and continues to make good progress.
| Platelets /μL | INR | Fibrinogen (mg/dL) | |
| Beginning of case | 44 000 | 1.8 | 210 |
| Detection of clot | 13 000 | 6.4 | < 25 |
| End of case | 55 000 | 1.7 | 196 |
Intracardiac thrombosis (ICT) during liver transplantation is a devastating complication with poor outcomes. Warnaar et al[1] reported a mortality rate of 68% with a majority of patients dying in the operating room. This complication is extremely rare (1%-1.5%) and unfortunately the exact etiology is not known. It has been associated with intraoperative administration of antifibrinolytics including epsilon-aminocaproic acid, aprotinin and clotting factors used to decrease intraoperative bleeding and transfusion requirement[2]. Other potential risk factors described are the presence of venovenous bypass, pulmonary artery catheter, continuous venovenous hemofiltration, migration of preexisting thrombi, sepsis and disseminated intravascular coagulation. Empiric administration of antifibrinolytics and clotting factors should be strongly discouraged since the risk of ICT formation and pulmonary embolus at times outweighs the risk of intraoperative bleeding.
Systemic hypotension, increase in central venous pressure, pulmonary artery pressure, decrease in cardiac output and cardiac arrest are frequently encountered signs[2]. The definitive diagnosis is made on transesophageal echocardiography.
There is no consensus for treatment since the condition is so rare. Administration of tissue plasminogen activator into the right atrium[2,3] and heparin boluses[4] have been described although they are associated with potentially massive hemorrhage. Suction embolectomy is another treatment option.
The source of the ICT in our patient is uncertain. It is unclear whether this clot was preformed or newly developed. After recirculation, our patient became profoundly coagulopathic. We believe that the fibrinolysis that occurred after reperfusion of the liver graft led to the lysis of the thrombus and subsequently to a successful outcome.
Peer reviewers: Valentina Medici, MD, PhD, Department of Internal Medicine, University of California Davis, 4150 V Street, Suite 3500, Sacramento, CA 95817, United States; Joseph Ahn, MD, Assistant Professor of Medicine, Medical Director, Liver Transplantation, Loyola University Medical Center, 2160 S. First Ave., Building 54, Room 007, Maywood, IL 60153, United States
| 1. | Warnaar N, Molenaar IQ, Colquhoun SD, Slooff MJ, Sherwani S, de Wolf AM, Porte RJ. Intraoperative pulmonary embolism and intracardiac thrombosis complicating liver transplantation: a systematic review. J Thromb Haemost. 2008;6:297-302. |
| 2. | Jackson D, Botea A, Gubenko Y, Delphin E, Bennett H. Successful intraoperative use of recombinant tissue plasminogen activator during liver transplantation complicated by massive intracardiac/pulmonary thrombosis. Anesth Analg. 2006;102:724-728. |
| 3. | Planinsic RM, Hilmi IA, Sakai T. Prevention of intracardiac/pulmonary thrombosis during liver transplantation. Anesth Analg. 2006;103:1329. |
| 4. | Planinsic RM, Nicolau-Raducu R, Eghtesad B, Marcos A. Diagnosis and treatment of intracardiac thrombosis during orthotopic liver transplantation. Anesth Analg. 2004;99:353-356, table of contents. |