Revised: January 14, 2010
Accepted: January 21, 2010
Published online: February 27, 2010
Post-traumatic hepatic artery pseudoaneurysm is uncommon, appearing in approximately 1% of hepatic trauma cases. Most are extrahepatic (80%) and have a late onset. Although they are usually asymptomatic, they should always be treated becasue of the high risk of complications, especially breakage. Currently the treatment of choice is endovascular embolization with coils or the exclusion of the pseudoaneurysm using other intravascular devices. Recently there have been accounts of a treatment that combines embolization with coils and image-guided percutaneous human thrombin injection. We present a case of post-traumatic hepatic artery pseudoaneurysm that was successfully treated using this combined technique.
- Citation: Francisco LE, Asunción LC, Antonio CA, Ricardo RC, Manuel RP, Caridad MH. Post-traumatic hepatic artery pseudoaneurysm treated with endovascular embolization and thrombin injection. World J Hepatol 2010; 2(2): 87-90
- URL: https://www.wjgnet.com/1948-5182/full/v2/i2/87.htm
- DOI: https://dx.doi.org/10.4254/wjh.v2.i2.87
Post-traumatic hepatic artery pseudoaneurysms are rare complications of blunt abdominal trauma. Patients are generally asymptomatic and diagnosis is an incidental finding. Occasionally they can be symptomatic and the most common clinical manifestations are abdominal pain, hematemesis, anemia, hypovolemia and jaundice[1,2].
The classical surgical management of these patients is changing because of the introduction of new endovascular and percutaneous approaches.
We report a case of post-traumatic hepatic artery pseudoaneurysm which was embolized with coils as a first therapeutic choice. However, due to its partial closure, the occlusion was completed using ultrasound-guided percutaneous human thrombin injection.
In an 18 year-old male patient who suffered a motorcycle accident,chest and abdominal computed tomography (CT) showed multiple pulmonary contusions, vertebral fractures, hemoperitoneum and splenic fracture. During an operation for splenectomy, a tiny hepatic laceration which was observed near the falciform ligament was electrocoagulated. The patient was admitted into the intensive care unit (ICU) and was discharged 2 mo later without relevant complications.
A CT during the ICU stay showed hepatic left lobe contusions, not seen in initial CT, which evolved favorably. The hepatic artery was normal in this control study and there was not any evident pseudoaneurysm.
Six months after the liver trauma the patient went to the emergency department complaining of colic-type abdominal pain, nausea, vomiting, pruritus and choluria. On physical examination jaundice was observed and blood tests indicated that there was an increase in total and direct bilirubin levels.
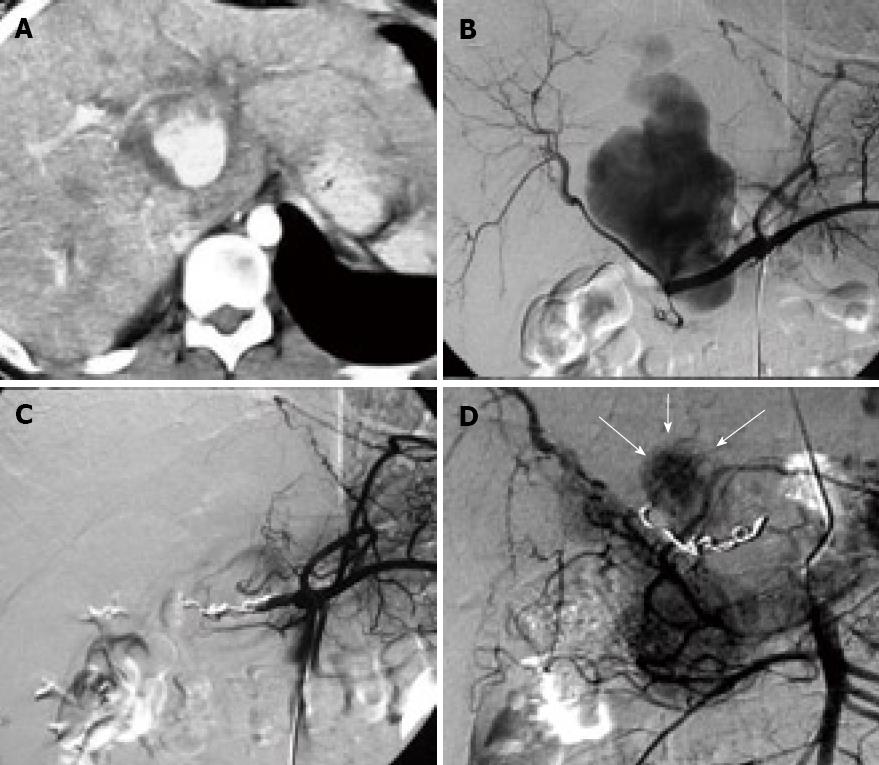
Emergency ultrasound showed moderate intrahepatic biliary dilation and a well defined hypoechogenic mass of 10 cm × 5 cm located in the hepatic hilum with features of pseudoaneurysm. Abdominal CT with intravenous contrast (120 mL; 4 mL/s; 80 s delay; pitch 1.5) confirmed the findings described in the ultrasound examination (Figure 1A).
Angiography of the celiac axis revealed the presence of a pseudoaneurysm which was joined to the hepatic artery through a short, narrow neck. A significant difference in caliper between the afferent and efferent arterial segment was evident (Figure 1B). Superior mesenteric artery angiography showed collateral branches that connected with the right hepatic artery. In indirect portography the permeability of the portal vein was confirmed.
Using selective catheterization of the common hepatic artery with a 4F cobra catheter (Cordis, L Roden, Holland) the afferent and efferent artery segment was embolized with 3 coils of 5 cm × 5 mm (Cook-coil for MREYE embolization, IMWCE 35-5-5; William Cook Europe). Closure of the pseudoaneurysm was confirmed in the immediate post-embolization test from the celiac axis (Figure 1C) and from the superior mesenteric artery.
Three days later, the patient presented with hematemesis, hematochezia, hypotension, decreased hematocrit and increased bilirubin. An endoscopy of the upper gastro-intestinal tract was normal. Given that there was suspicion of pseudoaneurysm breakage to the biliary tract, a new contrast enhanced abdominal CT was carried out. This revealed partial thrombosis of the pseudoaneurysm and persistent dilated intrahepatic bile ducts without free peritoneal fluid or collections. We carried out a second angiography, finding this time that the residual light of the pseudoaneurysm was fed by narrow vessels from the upper mesenteric artery (Figure 1D). We tried to carry out another embolization, but this time the thin branches could not be catheterized supraselectively.
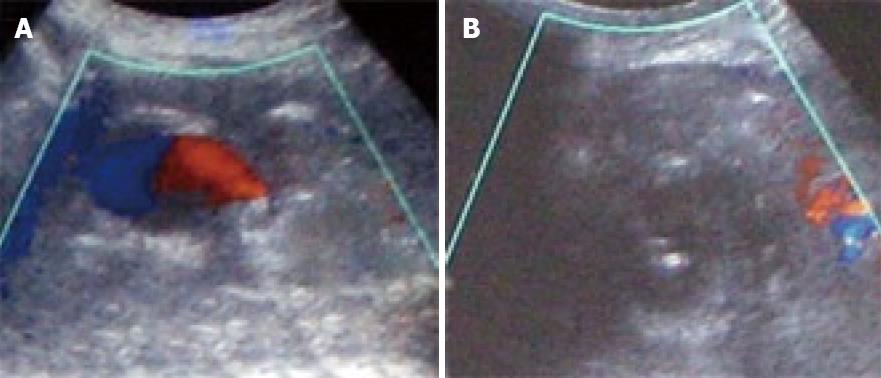
The next step we considered to achieve the total occlusion of the pseudoaneurysm was the direct injection of human thrombin with ultrasound guidance. We used a 22 G spinal needle (Boston Scientific Medi-tech) and 2 mL (500 UI/mL) of human thrombin was injected (Tissucol Duo; Baxter Health Care Corporation) controlling the entire procedure with Doppler ultrasound until the absence of flow in the lesion was confirmed (Figure 2).
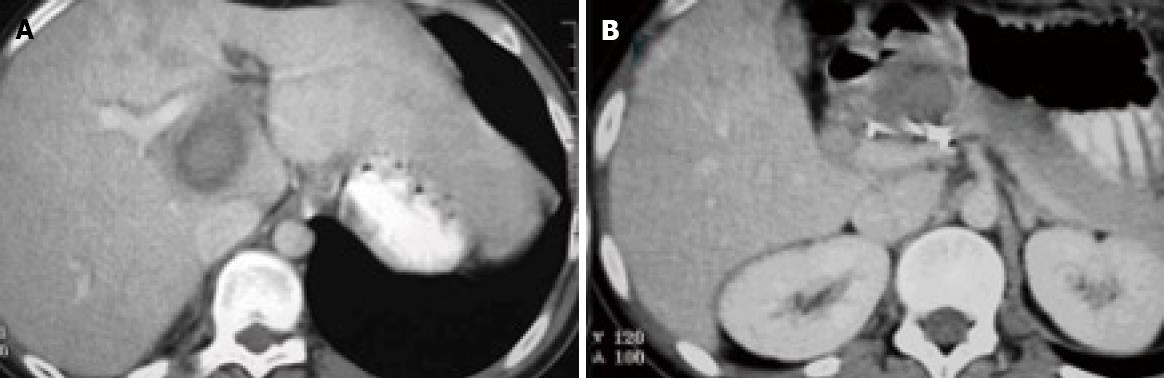
In follow-up at two years, the patient was asymptomatic and had totally normal bilirubin levels. Abdominal CT showed thrombosis of the pseudoaneurysm, decreased size and normal-sized bile ducts (Figure 3).
Conservative treatment has become the standard of care in hemodynamically stable patients with blunt liver trauma. Approximately 71%-89% of these patients are treated conservatively with a success rate of between 85%-94%[3-5]. Contrast enhanced abdominal CT is the imaging modality of choice for diagnosis and follow-up of these patients. It facilitates the evaluation of hepatic parenchyma and other abdominal and retroperitoneal organs; the presence and estimation of the quantity of hemoperitoneum. It also monitors the healing process and the evaluation of possible complications[2].
Delayed complications can occur from weeks to months after the trauma and they include delayed hemorrhage, post-traumatic pseudoaneurysm, abscesses, hemobilia and biliary complications such as biloma and biliary peritonitis[2].
Post-traumatic hepatic artery pseudoaneurysm is an uncommon delayed complication. Although they are usually asymptomatic and found at follow-up by CT or ultrasound, they should be treated as early as possible because they have a high risk of rupture and are associated with high morbidity[1,6,7].
Conventional treatments include either endovascular embolization or surgery. Whereas surgery is associated with significant morbidity and mortality, endovascular embolization is safe and effective and has emerged as the primary line of treatment and the most commonly used option[2,8,9]. Coils are the most commonly used materials and the afferent and efferent artery segments should be embolized to avoid retrograde filling, achieving a success rate of 70%-100%. On occasions, the pseudoaneurysm cannot be totally thrombosed by this way because the occlusion of the vessel has not been complete or because it is fed by collaterals. On these occasions, embolization should be attempted again through the endovascular route. Distal coil migration, hepatic abscess and hepatic ischemia are some of the reported complications of endovascular hepatic artery embolization[9].
Another percutaneous treatment options available are described below.
Image guided human thrombin injection: Image guided human thrombin injection has been widely used in peripheral false aneurysms that occur mainly as a consequence of angiographies. The recurrence rate is 2.08% after thrombin treatment for femoral pseudoaneurysms[10,11], almost always when the neck is wide. Unwanted effects of thrombin injection in arterial false aneurysms are infrequent and can be classified into thrombotic and immunologic. Distal arterial thrombosis after thrombin injection occurs in approximately 0.95% of cases for femoral pseudoaneurysms, generally when the neck is wide, the flow is very fast or the thrombin is injected near the neck and without enough imaging control[12]. The consequences are rarely serious. Thrombin has also been used in another locations such as the common iliac artery[13], radial[14] and visceral arteries without complications[9,15]. The immunologic complications where described when using bovine thrombin and include the development of antibodies with the potential risk of bleeding and coagulopathy. A number of recent studies have demonstrated that human thrombin does not seem to incur any risk of immunologic sensitization[16].
Endovascular treatment: There is also the possibility of endovascular treatment by placing a stent and using liquid agents like glue. With uncovered stents, the false aneurysm is not excluded from blood flow and it is possible that it might not thrombose, especially when the neck is wide. Through the mesh of these stents it is possible to access into the pseudoaneurysm and embolize it with microcoils, achieving better results than when only the prosthesis alone is used[17,18]. With covered stents the pseudoaneurysm is excluded although these could have potential disadvantages because of technical difficulties in negotiating tortuous vessels and the low flexibility of the endoprosthesis[16].
In our patient, after carrying out an angiography and seeing the features of the pseudoaneurysm as well as hepatic arterial and portal vascularization, it was decided to embolize the afferent and efferent arterial segments with coils. The possibility of positioning a covered stent was considered but, due to the difference in caliber between the afferent and efferent arterial segments, the existence of collaterals for the right hepatic lobe from the upper mesenteric artery and the normal flow in the portal vein we believed it was safer to carry out the embolization of the hepatic artery. After the embolization we checked correct closure of the false aneurysm from the celiac axis and from the superior mesenteric artery. Two days later, a small residual cavity still remained. On this occasion it was not possible repeat the endovascular embolization with coils because the afferent vessel were thin and tortuous and we therefore decided to inject human thrombin percutaneously and with color doppler ultrasound control[9]. The effects were immediate after the injection of human thrombin, leaving the residual light closed. Although we could have used a direct injection with thrombin from the start, we believe that the slow-down in flow provoked by the coils improved the success of the thrombin treatment.
To summarize, for the treatment of visceral pseudoaneurysms it is necessary to know all therapeutic options and to evaluate the convenience of each one. In the absence of studies with a large number of patients to validate one or other treatment as the preferred option, we contribute by adding our experience to the cases reported in the bibliography.
Peer reviewer: Dr. Patrick Veit-Haibach, MD, University Hospital Zürich, Department of Nuclear Medicine, Raemistrasse 100, Zürich 80941, Switzerland
| 1. | Croce MA, Fabian TC, Spiers JP, Kudsk KA. Traumatic hepatic artery pseudoaneurysm with hemobilia. Am J Surg. 1994;168:235-238. |
| 2. | Yoon W, Jeong YY, Kim JK, Seo JJ, Lim HS, Shin SS, Kim JC, Jeong SW, Park JG, Kang HK. CT in blunt liver trauma. Radiographics. 2005;25:87-104. |
| 3. | Malhotra AK, Fabian TC, Croce MA, Gavin TJ, Kudsk KA, Minard G, Pritchard FE. Blunt hepatic injury: a paradigm shift from operative to nonoperative management in the 1990s. Ann Surg. 2000;231:804-813. |
| 4. | Velmahos GC, Toutouzas K, Radin R, Chan L, Rhee P, Tillou A, Demetriades D. High success with nonoperative management of blunt hepatic trauma: the liver is a sturdy organ. Arch Surg. 2003;138:475-480; discussion 480-481. |
| 5. | David Richardson J, Franklin GA, Lukan JK, Carrillo EH, Spain DA, Miller FB, Wilson MA, Polk HC Jr, Flint LM. Evolution in the management of hepatic trauma: a 25-year perspective. Ann Surg. 2000;232:324-330. |
| 6. | Pachter HL, Knudson MM, Esrig B, Ross S, Hoyt D, Cogbill T, Sherman H, Scalea T, Harrison P, Shackford S. Status of nonoperative management of blunt hepatic injuries in 1995: a multicenter experience with 404 patients. J Trauma. 1996;40:31-38. |
| 7. | Basile KE, Sivit CJ, Sachs PB, Stallion A. Hepatic arterial pseudoaneurysm: a rare complication of blunt abdominal trauma in children. Pediatr Radiol. 1999;29:306-308. |
| 8. | Sun L, Guan YS, Wu H, Pan WM, Li X, He Q, Liu Y. Post-traumatic hepatic artery pseudo-aneurysm combined with subphrenic liver abscess treated with embolization. World J Gastroenterol. 2006;12:2798-2799. |
| 9. | Dambrin C, Marcheix B, Birsan T, Cron C, Muscari F, Suc B, Cérène A, Rousseau H. Posttraumatic pseudoaneurysm of the hepatic artery: treatment with ultrasound-guided percutaneous transhepatic thrombin injection. J Trauma. 2005;59:239-242. |
| 10. | Vázquez V, Reus M, Morales MD, Abellán J, Piñero A, Soria F, Parrilla P. [Usefulness of sonographically guided thrombin injection of iatrogenic femoral pseudoaneurysms]. Med Clin (Barc). 2003;121:53-57. |
| 11. | Vázquez V, Reus M, Piñero A, Abellán D, Canteras M, Espinosa de Rueda M, Morales D, Parrilla P. Human thrombin for treatment of pseudoaneurysms: comparison of bovine and human thrombin sonogram-guided injection. AJR Am J Roentgenol. 2005;184:1665-1671. |
| 12. | Kang SS, Labropoulos N, Mansour MA, Michelini M, Filliung D, Baubly MP, Baker WH. Expanded indications for ultrasound-guided thrombin injection of pseudoaneurysms. J Vasc Surg. 2000;31:289-298. |
| 13. | Reus M, Morales D, Vázquez V, Llorente S, Alonso J. Ultrasound-guided percutaneous thrombin injection for treatment of extrarenal pseudoaneurysm after renal transplantation. Transplantation. 2002;74:882-884. |
| 14. | Reus M, Vázquez V, Alonso J, Morales D, Rodríguez JM. Treatment of a radial artery pseudoaneurysm with ultrasound-guided percutaneous thrombin injection in a patient with Behçet’s syndrome. J Clin Ultrasound. 2003;31:440-444. |
| 15. | Krueger K, Zaehringer M, Lackner K. Percutaneous treatment of a splenic artery pseudoaneurysm by thrombin injection. J Vasc Interv Radiol. 2005;16:1023-1025. |
| 16. | Paci E, Antico E, Candelari R, Alborino S, Marmorale C, Landi E. Pseudoaneurysm of the common hepatic artery: treatment with a stent-graft. Cardiovasc Intervent Radiol. 2000;23:472-474. |
| 17. | Ichihara T, Sato T, Miyazawa H, Shibata S, Hashimoto M, Ishiyama K, Yamamoto Y. Stent placement is effective on both postoperative hepatic arterial pseudoaneurysm and subsequent portal vein stricture: a case report. World J Gastroenterol. 2007;13:970-972. |
| 18. | Hartnell GG, Gates J. Treatment of gastroduodenal artery hemorrhage with a conventional stent. J Vasc Interv Radiol. 1999;10:172-174. |