Published online Jan 27, 2025. doi: 10.4254/wjh.v17.i1.101664
Revised: November 5, 2024
Accepted: November 19, 2024
Published online: January 27, 2025
Processing time: 105 Days and 18.7 Hours
Hepatic eosinophilic pseudotumor (HEPT) is a rare condition that mimics ma
A 40-year-old female presented with a 1-month history of epigastric pain and significant weight loss. Imaging revealed a hepatic mass, initially misdiagnosed as intrahepatic cholangiocarcinoma. Laboratory results showed marked eosinophilia, and histopathological examination confirmed significant eosinophilic infiltration without malignancy. Serological testing identified F. hepatica infection. The patient was treated with a single dose of triclabendazole, leading to complete symptom resolution and normalization of hepatic imaging findings within days.
HEPT due to F. hepatica can closely mimic malignancy; timely antiparasitic treat
Core Tip: This manuscript presents a case of hepatic eosinophilic pseudotumor (HEPT) misdiagnosed as intrahepatic cholangiocarcinoma, later confirmed to be caused by Fasciola hepatica infection. HEPT, a rare benign condition characterized by dense eosinophilic infiltration, mimics malignant hepatic tumors, posing significant diagnostic challenges. The report emphasizes the importance of histopathological and serological analyses in differentiating HEPT from malignancies, especially in endemic regions. The case demonstrated the efficacy of triclabendazole in resolving HEPT secondary to parasitic infection, highlighting the need for awareness of parasitic causes in atypical hepatic lesions.
- Citation: Le KL, Tran MQ, Pham TN, Duong NNQ, Dinh TT, Le NK. Hepatic eosinophilic pseudotumor due to Fasciola hepatica infection mimicking intrahepatic cholangiocarcinoma: A case report. World J Hepatol 2025; 17(1): 101664
- URL: https://www.wjgnet.com/1948-5182/full/v17/i1/101664.htm
- DOI: https://dx.doi.org/10.4254/wjh.v17.i1.101664
Hepatic eosinophilic pseudotumor (HEPT) is a rare and often overlooked condition, marked by dense eosinophilic infiltration within the liver parenchyma that can mimic malignant hepatic tumors both clinically and radiologically[1-3]. Despite its benign nature, HEPT poses a substantial diagnostic challenge due to its close resemblance to primary hepatic malignancies or metastatic lesions on imaging. The differential diagnosis for hepatic masses presenting with eosinophilic infiltration is extensive, encompassing a range of infectious, inflammatory, and neoplastic processes. This broad spectrum necessitates a meticulous and comprehensive diagnostic approach to prevent unwarranted surgical or medical inter
Among the various etiologies of HEPT, parasitic infections-particularly those caused by liver flukes such as Fasciola hepatica (F. hepatica)-are noteworthy. Recently, cases of HEPT directly linked to liver fluke infections have been do
Although serologic testing for liver flukes is widely recommended for diagnosing HEPT, reports exist where such testing was bypassed[1,10]. In those cases, the absence of parasitic evaluation may lead clinicians toward alternative treatments, including corticosteroids or even hepatic resection. This approach can complicate management by potentially overlooking an infectious etiology, thereby exposing patients to treatments more suited to autoimmune or idiopathic conditions rather than parasitic infection, underscoring the importance of thorough initial testing in suspected HEPT cases.
Given the rarity of HEPT and the significant diagnostic conundrum it presents, the documentation of such cases is vital. This will not only raise awareness among clinicians but also inform on management strategies for similar clinical scenarios. In this report, we present a case of HEPT that was initially misdiagnosed as intrahepatic cholangiocarcinoma and later identified to be secondary to F. hepatica infection based on histopathological and serological findings. Re
A 40-year-old female presented with a chief complaint of abdominal pain that had persisted for 1 month.
The patient described the pain as a dull ache localized to the epigastric region, unrelated to food intake and occasionally accompanied by chills which were alleviated by antipyretic medications. During this period, she also experienced a significant reduction in appetite and an unintentional weight loss of 5 kg. There were no changes in bowel habits nor in stool characteristics.
The patient’s past medical history was notable for hypertension managed with medication. She denied any prior surgical history. Occupationally, she worked as a seamstress.
Her dietary habits included a strict regimen of consuming well-cooked foods and boiled water, with infrequent con
On examination, there was mild tenderness to palpation in the epigastric region, with no evidence of guarding or rebound tenderness. The remainder of the physical examination was unremarkable.
Laboratory investigations revealed mild anemia and marked eosinophilia, while liver function tests and bilirubin levels were within normal limits (Table 1). Tumor markers, including carcinoembryonic antigen and carbohydrate antigen 19-9, were not elevated.
| Parameter | Result |
| Blood test | |
| White blood cells | 9.71 K/µL |
| Eosinophils | 35.3% |
| Neutrophils | 39.1% |
| Hemoglobin | 120 g/L |
| Hematocrit | 37.4% |
| Aspartate aminotransferase | 27.2 U/L |
| Alanine aminotransferase | 30.4 U/L |
| Total bilirubin | 6.0 μmol/L |
| Direct bilirubin | 2.28 μmol/L |
| Carcinoembryonic antigen | < 0.5 ng/mL |
| Carbohydrate antigen 19-9 | < 2.0 ng/mL |
| Diagnostic serum test | |
| Hepatitis B surface antigen | Negative (0.27) |
| Quantitative hepatitis B surface antibody | 91.48 mIU/mL |
| Hepatitis C virus antibody | Negative (0.11) |
| Fasciola sp. IgG | Positive (0.976) |
| Entamoeba histolytica IgG | Negative (0.08) |
| Toxocara IgG | Negative (0.17) |
| Strongyloides stercoralis IgG | Grayzone (0.26) |
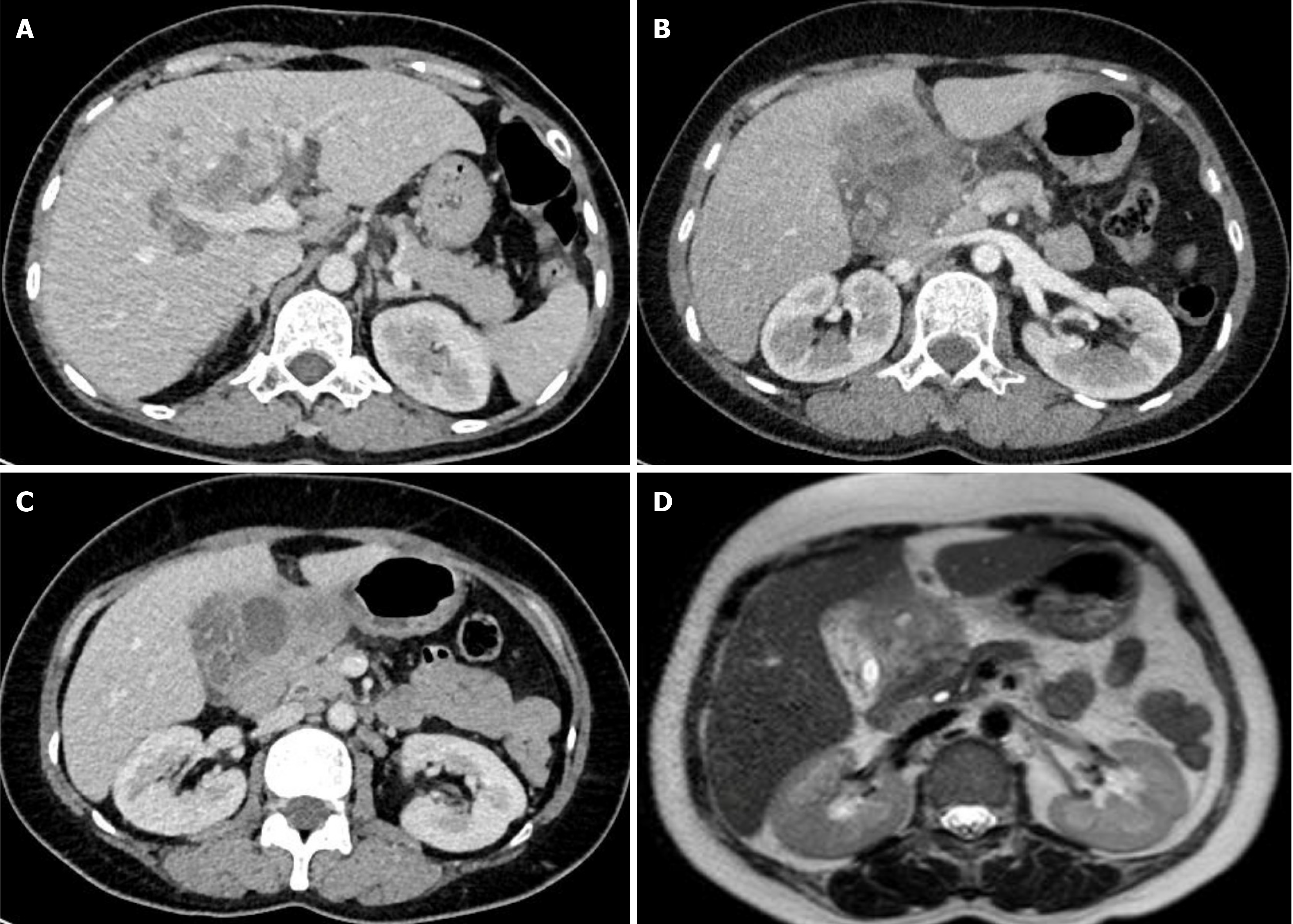
Initial abdominal ultrasound revealed a mass in the left hepatic lobe, protruding into the abdominal cavity and exerting pressure on the lesser curvature of the stomach. The imaging raised concerns for a potential gastric mass invading the liver. However, esophagogastroduodenoscopy showed no abnormalities in the gastric mucosa, effectively ruling out a gastric origin. Further imaging with contrast-enhanced computed tomography (CT) and magnetic resonance imaging of the liver (Figure 1) demonstrated a mass in the hepatic hilum, particularly involving segment IV, raising suspicion for intrahepatic cholangiocarcinoma with possible invasion into the gallbladder.
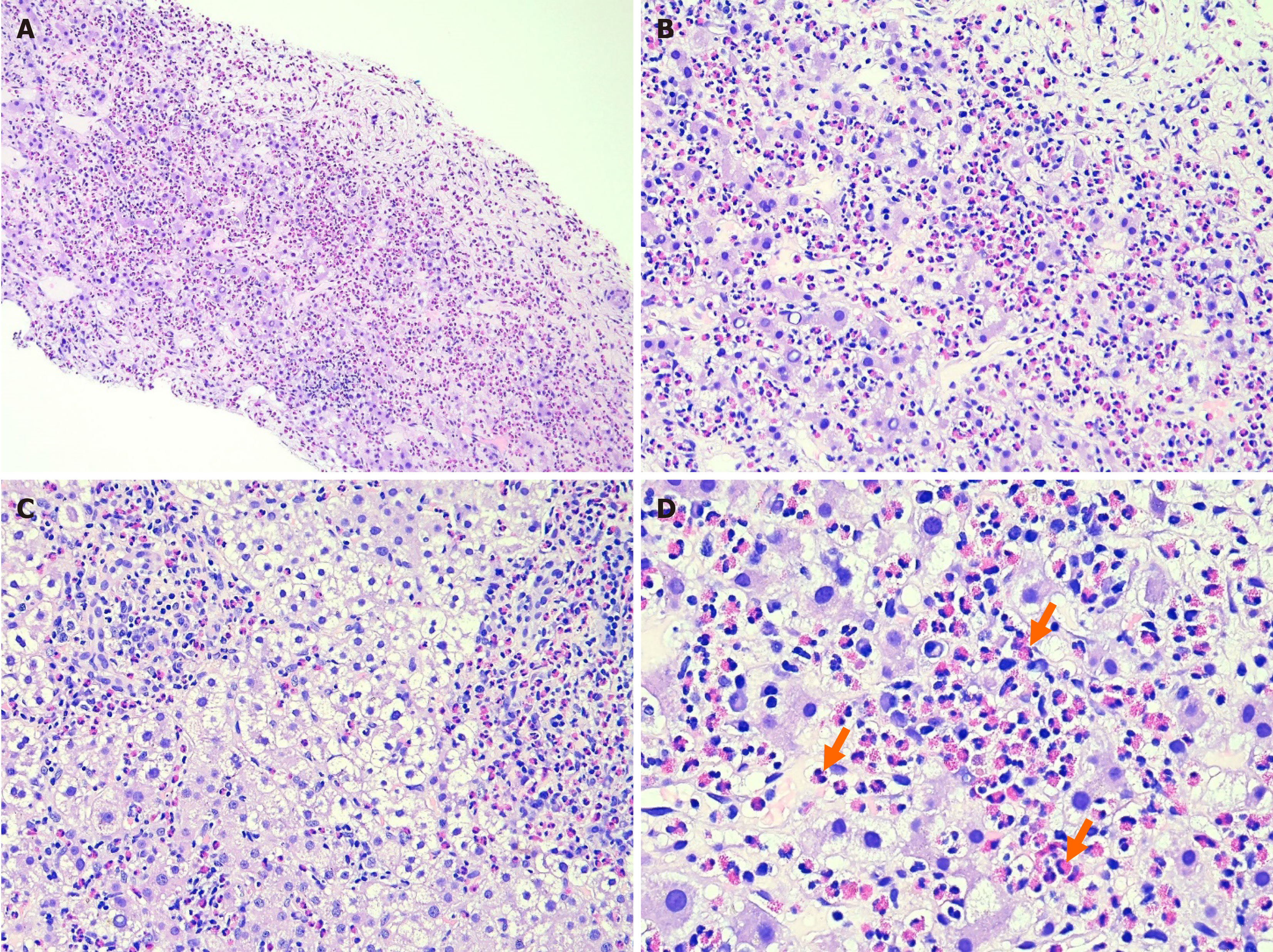
After a comprehensive review by the multidisciplinary tumor board, a percutaneous core needle biopsy of the liver was performed, which showed acute inflammation in the portal tracts extending into the lobules, with marked eosinophilic infiltration and no evidence of malignancy (Figure 2). A second biopsy reaffirmed these findings. In light of the absence of malignant cells across both samples, the noted eosinophilia, and the endemic nature of parasitic infections in Vietnam, the tumor board recommended targeted serological tests for parasites common in the region. The results of such pointed towards a HEPT. Subsequent serological testing showed positivity for IgG antibodies for Fasciola species and ruled out other prevalent parasitic infections. A definitive diagnosis of HEPT secondary to hepatic fascioliasis was thus established.
HEPT secondary to hepatic fascioliasis.
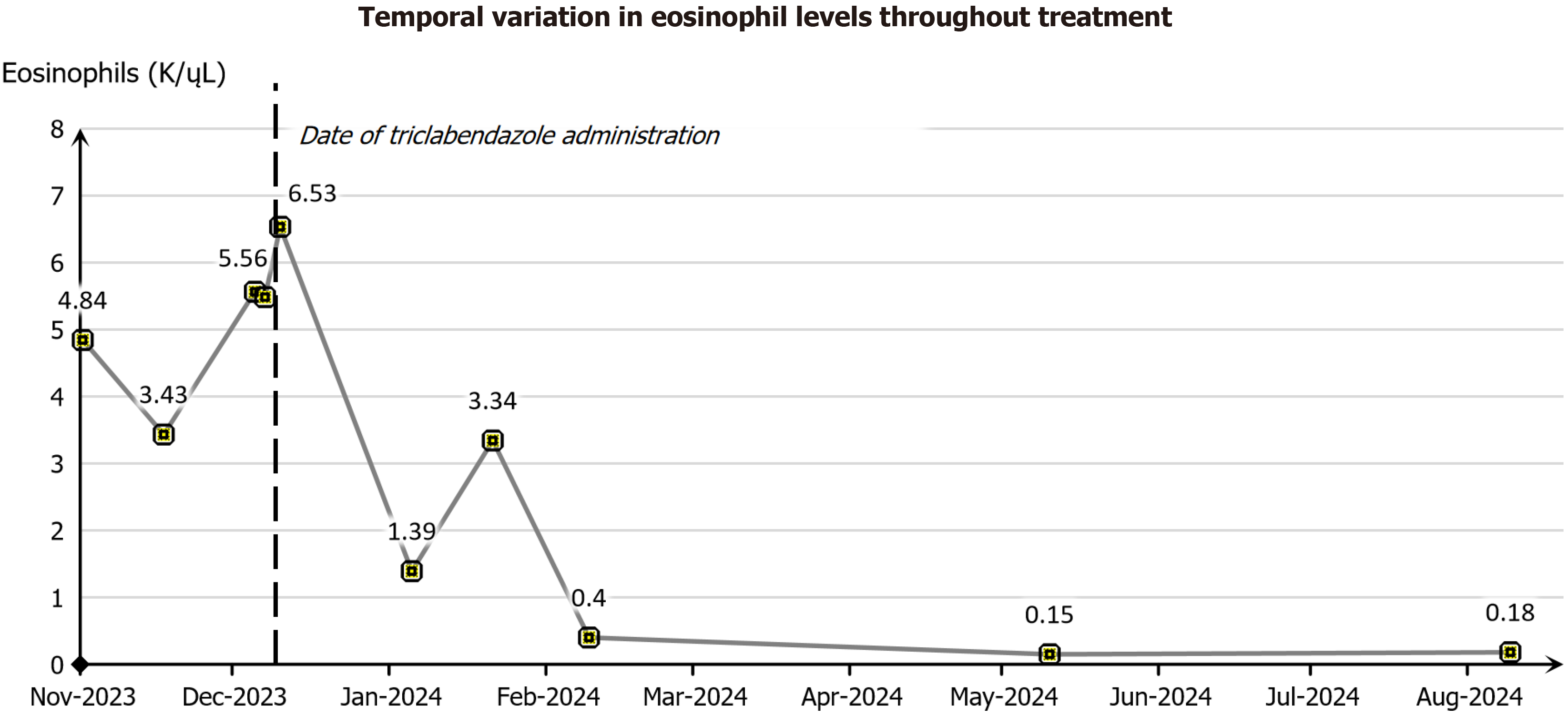
The patient was treated with a single oral dose of triclabendazole (10 mg/kg). Following treatment, her symptoms, including jaundice and epigastric pain, showed marked improvement, with complete resolution within 3 days. No adverse reactions to the medication were observed. The dramatic clinical response, along with progressive decline in peripheral eosinophil count after the triclabendazole administration, further reinforced the determination of hepatic fascioliasis as the underlying cause of HEPT.
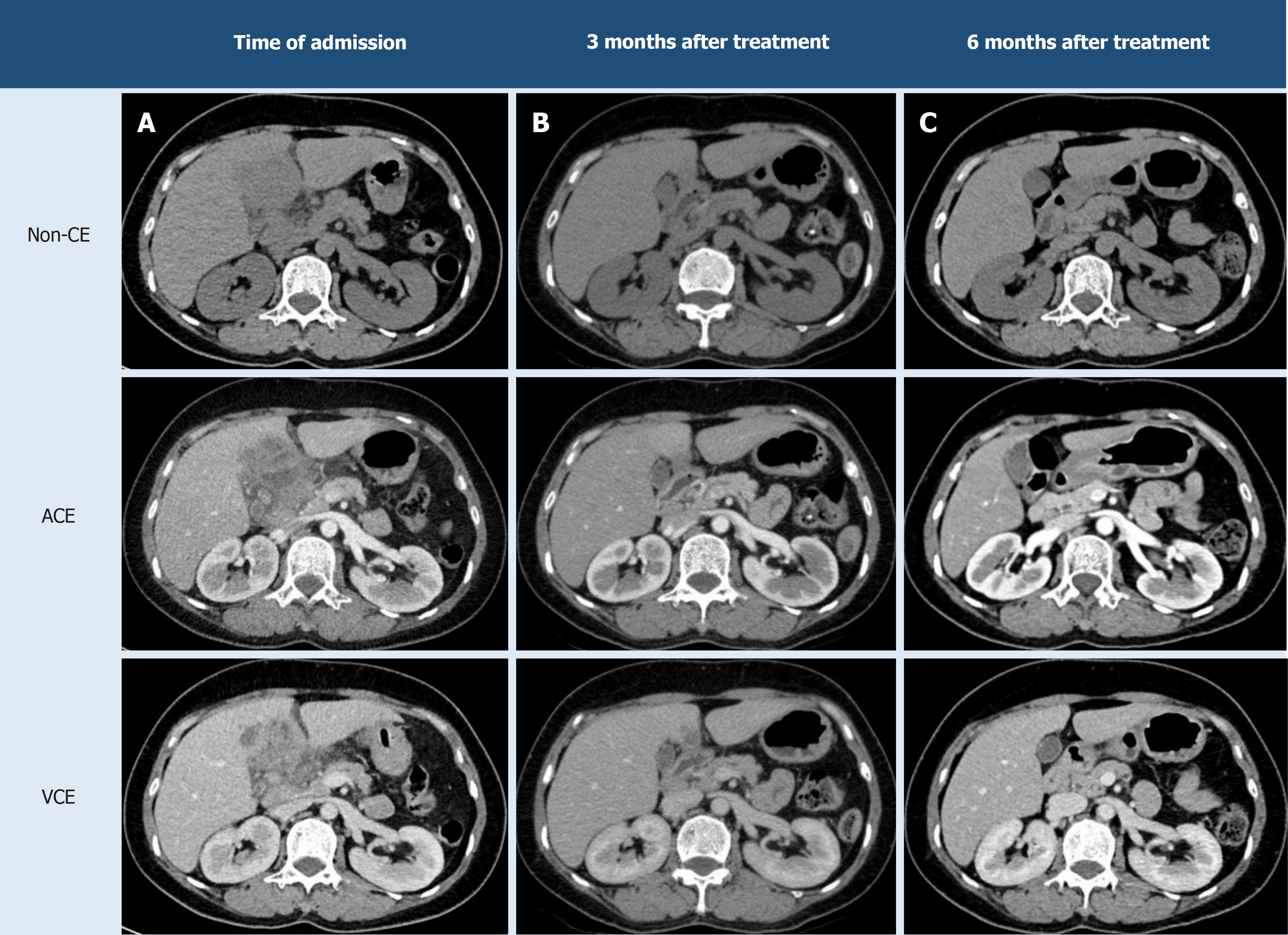
The patient was discharged with instructions for close follow-up, as malignancy could not be ruled out entirely by imaging and hepatic fascioliasis itself poses a risk for cholangiocarcinoma. Follow-up visits were scheduled every 2 weeks for the 1st month and then monthly for the subsequent 3 months. At her 6-month follow-up, the patient remained asymptomatic, with a 2 kg weight gain and a normalized eosinophil count (Figure 3). Repeat CT imaging demonstrated complete resolution of the hepatic lesion (Figure 4).
The key events of this clinical case, including the progression from initial symptoms to diagnosis and treatment, are summarized in Table 2. This table provides a clear and concise timeline of the significant clinical milestones, illustrating the diagnostic challenges encountered and the subsequent resolution of HEPT following the triclabendazole treatment.
| Timeframe | Event |
| 1 month prior admission | Patient presented with recurring upper abdominal pain, fever with chills, and significant weight loss |
| Week 1 | Patient underwent a clinical evaluation and basic laboratory tests, including complete blood count and tumor markers |
| Week 2 | Abdominal CT and magnetic resonance imaging scans revealed a mass in the hepatic hilum, raising suspicion of intrahepatic cholangiocarcinoma |
| Week 3 | Liver biopsies, performed twice, showed no malignant cells but revealed significant eosinophilic infiltration |
| Week 4 | Serologic testing was positive for Fasciola hepatica; treatment with triclabendazole was initiated |
| 6 months later | The patient exhibited marked symptom improvement, weight gain, and complete resolution of the hepatic mass on imaging studies. Furthermore, serologic testing for Fasciola sp. IgG yielded negative results, and stool examinations for parasitic identification were also negative |
The patient had reported significant anxiety and distress upon initially learning of the potential diagnosis of cholangiocarcinoma, which contributed to her marked weight loss. At follow-up, she expressed great relief and satisfaction with the diagnostic process and treatment outcome, particularly with the resolution of her symptoms and the disappearance of the hepatic mass on imaging.
HEPT is a rare clinical entity that poses a considerable diagnostic challenge due to its nonspecific clinical presentation and ambiguous radiological features[4,11]. HEPT often mimics malignancy, as exemplified by our case, where initial imaging suggested intrahepatic cholangiocarcinoma. This diagnostic complexity is compounded by the rarity of HEPT, particularly when it is associated with parasitic infections such as F. hepatica.
The eosinophilic infiltration characteristic of HEPT can be triggered by various factors, including parasitic infections, drug reactions, and autoimmune disorders[12]. This underscores the need for a comprehensive diagnostic approach to differentiate HEPT from other hepatic pathologies. The pathogenesis of HEPT remains unclear; however, it is thought to involve an eosinophilic response to a local or systemic trigger, as demonstrated in cases involving parasitic infections like F. hepatica.
The challenges in diagnosing HEPT are well-documented in the literature. Reviews, such as those by Krsak et al[6] and Patel et al[13], highlight cases where HEPT was initially misdiagnosed as malignant lesions, leading to unnecessary surgical interventions. The study from Patel et al[13] further elaborated on the imaging characteristics of HEPT, noting that hypoenhancing lesions on contrast-enhanced CT and magnetic resonance imaging can closely resemble intrahepatic cholangiocarcinoma, which aligns with the findings in our case.
Histopathological examination remains crucial in distinguishing HEPT from malignant hepatic lesions. The absence of cellular anaplasia and the presence of dense eosinophilic infiltrates, as seen in our patient’s biopsies, are key in steering the diagnosis away from malignancy and towards HEPT associated with parasitic infection. Our case adds to the growing body of evidence advocating for a thorough, multidisciplinary approach when evaluating hepatic lesions with atypical presentations to avoid misdiagnosis and ensure appropriate management.
For our case the diagnosis was ultimately established through histopathological examination, which demonstrated significant eosinophilic infiltration in the absence of malignant cells, along with a positive serological test for F. hepatica. The patient’s prompt response to antiparasitic treatment with triclabendazole further substantiated the diagnosis of a parasitic-induced pseudotumor. This case emphasizes the importance of considering parasitic infections, particularly F. hepatica, in the differential diagnosis of hepatic masses, especially in regions where such infections are endemic.
In Vietnam, F. hepatica infection, or fascioliasis, remains a public health concern, particularly in rural and endemic areas[14]. Recent studies indicate that the prevalence of fascioliasis among humans in certain regions of Vietnam is significant, with rates varying from 4.4% to as high as 66.2% in snail intermediate hosts, which serve as a critical reservoir for the parasite[15,16]. Given the high prevalence in these endemic areas, clinicians should maintain a high index of suspicion for fascioliasis in patients presenting with atypical hepatic lesions and eosinophilia. This awareness is critical to prevent misdiagnosis and to avoid unnecessary invasive procedures, such as those that might be considered if a malignancy is incorrectly assumed.
HEPT can be managed using various treatment options depending on the severity and underlying cause. Conservative therapy is often the first line of treatment. Antibiotics may be effective[4,17], particularly when the pseudotumor results from an infection, helping to avoid surgical interventions. In some cases, corticosteroids like prednisolone have shown positive outcomes by reducing eosinophil counts and alleviating symptoms[1,18]. Nonsteroidal anti-inflammatory drugs have also been successfully utilized to manage hepatic inflammatory pseudotumors[4,17]. When conservative treatments fail or the diagnosis remains unclear, surgical resection becomes necessary[2,19]; it can, however, offer a definitive cure in cases with severe symptoms. In very rare and extreme cases, liver transplantation has been performed as a last resort. Notably, spontaneous regression of the pseudotumor may occur, though this is not a dependable outcome[4,17].
Triclabendazole, endorsed by both the World Health Organization (WHO) and the United States Food and Drug Administration, is the preferred treatment for fascioliasis due to its demonstrated efficacy and favorable safety profile. Recognized by the WHO as the only effective medication for infections caused by F. hepatica and Fasciola gigantica, triclabendazole uniquely targets both immature and adult stages of these liver flukes, making it essential for managing this zoonotic disease[20,21]. Clinical studies have shown that triclabendazole is generally well-tolerated, with most side effects being mild and transient, including abdominal pain, nausea, and dizziness[21]. However, in rare instances, more severe reactions like elevated liver enzymes and allergic responses have been documented. In our case, a single oral dose of triclabendazole at 10 mg/kg resulted in complete resolution of symptoms and normalization of hepatic imaging findings within a few days, with no side effects reported by the patient. This outcome reinforces the effectiveness of triclabendazole as a first-line therapy for F. hepatica infection and highlights the importance of timely antiparasitic treatment in avoiding further complications associated with untreated fascioliasis. The high efficacy of the drug combined with its ability to treat both acute and chronic stages of infection underscores its vital role in the management of fascioliasis.
The WHO provides specific recommendations to prevent fascioliasis, emphasizing the importance of reducing exposure to contaminated water and aquatic vegetation. Key preventive strategies include avoiding the consumption of raw or undercooked aquatic plants, such as watercress, which can serve as a transmission route for Fasciola parasites. Moreover, in endemic regions, people are encouraged to use only clean, treated water for drinking and food preparation to minimize the risk of ingesting infective metacercariae. Public health education undoubtedly plays a significant role in endemic areas, where community awareness of hygiene and safe practices is essential to prevent transmission.
This case underscores the diagnostic complexities of HEPT secondary to F. hepatica infection, which can closely mimic intrahepatic cholangiocarcinoma on imaging studies. Given the imaging similarities, Fasciola infection should be considered in patients presenting with HEPT, especially for those in endemic areas or with recent travel history to such regions. Accurate diagnosis relies on a combination of histopathological examination and serological testing, highlighting the critical role of these methods in differentiating parasitic infections from malignant liver lesions.
Importantly, antiparasitic therapy provides rapid and effective symptom relief without the side effects of prolonged corticosteroid use or the risks associated with unnecessary surgery-both common proposals in similar cases. Moreover, this therapy may serve as a diagnostic trial, helping to confirm Fasciola infection as the underlying cause of HEPT. Successful treatment with antiparasitic agents can lead to complete clinical and radiological resolution, reinforcing the importance of considering parasitic infections in the differential diagnosis of hepatic masses. Further case reports and studies are warranted to enhance our understanding and management strategies for this rare but clinically significant condition, especially given the recent Fasciola outbreaks in Vietnam and globally.
We extend our heartfelt thanks to Master Dinh-Khanh Do, Head of the Department of Pathology at Nhan Dan Gia Dinh Hospital, for his invaluable assistance in analyzing the pathological images. His expertise and support have been instrumental to our research.
| 1. | Matsumoto Y, Ogawa K, Shimizu A, Nakamura M, Hoki S, Kuroki S, Yano Y, Ikuta K, Senda E, Shio S. Inflammatory Pseudo-tumor of the Liver Accompanied by Eosinophilia. Intern Med. 2021;60:2075-2079. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Zhang Y, Lu H, Ji H, Li Y. Inflammatory pseudotumor of the liver: A case report and literature review. Intractable Rare Dis Res. 2015;4:155-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Faraj W, Ajouz H, Mukherji D, Kealy G, Shamseddine A, Khalife M. Inflammatory pseudo-tumor of the liver: a rare pathological entity. World J Surg Oncol. 2011;9:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Samanta A, Sen Sarma M. Hepatic pseudotumor: A diagnostic challenge. World J Hepatol. 2024;16:667-670. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 5. | Birlutiu V, Birlutiu RM. The First Case of Human Hepatic Fasciolosis Presented as Hepatic Pseudotumor Histopathologically Diagnosed in Romania-A Case Report. Healthcare (Basel). 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Krsak M, Patel NU, Poeschla EM. Case Report: Hepatic Fascioliasis in a Young Afghani Woman with Severe Wheezing, High-Grade Peripheral Eosinophilia, and Liver Lesions: A Brief Literature Review. Am J Trop Med Hyg. 2019;100:588-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Girma A, Belete Y, Afework S, Bisrat T. The Liver's hidden foe: A case study on Human Fasciolasis. IDCases. 2024;37:e02045. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Charatcharoenwitthaya P, Apisarnthanarak P, Pongpaibul A, Boonyaarunnate T. Eosinophilic pseudotumour of the liver. Liver Int. 2012;32:311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Sivagnanam S, van der Poorten D, Douglas MW. Hepatic lesions and eosinophilia in an urban dweller. Liver Int. 2014;34:643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Park JY, Choi MS, Lim YS, Park JW, Kim SU, Min YW, Gwak GY, Paik YH, Lee JH, Koh KC, Paik SW, Yoo BC. Clinical features, image findings, and prognosis of inflammatory pseudotumor of the liver: a multicenter experience of 45 cases. Gut Liver. 2014;8:58-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Balabaud C, Bioulac-Sage P, Goodman ZD, Makhlouf HR. Inflammatory pseudotumor of the liver: a rare but distinct tumor-like lesion. Gastroenterol Hepatol (N Y). 2012;8:633-634. [PubMed] |
| 12. | Sim DW, Son DJ, Cho E, Choi SK, Shin SS, Jun CH. What Are the Clinical Features and Etiology of Eosinophilic Liver Infiltration? Gut Liver. 2019;13:183-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Patel NU, Bang TJ, Dodd GD 3rd. CT findings of human Fasciola hepatica infection: case reports and review of the literature. Clin Imaging. 2016;40:251-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | De NV, Minh PN, Le TH, Dung DT, Duong TT, Tuan BV, Dong LT, Chau NVV, Cuervo PF, Bargues MD, Valero MA, Gabrielli AF, Montresor A, Mas-Coma S. A multidisciplinary analysis of over 53,000 fascioliasis patients along the 1995-2019 countrywide spread in Vietnam defines a new epidemiological baseline for One Health approaches. One Health. 2024;19:100869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 15. | Hoang Quang V, Levecke B, Do Trung D, Devleesschauwer B, Vu Thi Lam B, Goossens K, Polman K, Callens S, Dorny P, Dermauw V. Fasciola spp. in Southeast Asia: A systematic review. PLoS Negl Trop Dis. 2024;18:e0011904. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Bui TD, Doanh PN, Saegerman C, Losson B. Current status of fasciolosis in Vietnam: an update and perspectives. J Helminthol. 2016;90:511-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Ballester-Pla N, García-Domínguez R, Pérez-Girbes A, Orbis-Castellanos JF, Pareja E. Conservative treatment of hepatic inflammatory pseudotumor. Cir Esp. 2016;94:422-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Sasahira N, Kawabe T, Nakamura A, Shimura K, Shimura H, Itobayashi E, Asada M, Shiratori Y, Omata M. Inflammatory pseudotumor of the liver and peripheral eosinophilia in autoimmune pancreatitis. World J Gastroenterol. 2005;11:922-925. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Zhang DY, Weng SQ, Dong L, Shen XZ. Eosinophilic pseudotumor of the liver: report of six cases and review of literature. J Dig Dis. 2015;16:159-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Ashrafi K, Bargues MD, O'Neill S, Mas-Coma S. Fascioliasis: a worldwide parasitic disease of importance in travel medicine. Travel Med Infect Dis. 2014;12:636-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 21. | Gandhi P, Schmitt EK, Chen CW, Samantray S, Venishetty VK, Hughes D. Triclabendazole in the treatment of human fascioliasis: a review. Trans R Soc Trop Med Hyg. 2019;113:797-804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 72] [Article Influence: 14.4] [Reference Citation Analysis (0)] |