Published online Sep 27, 2024. doi: 10.4254/wjh.v16.i9.1289
Revised: July 26, 2024
Accepted: August 28, 2024
Published online: September 27, 2024
Processing time: 215 Days and 2.2 Hours
Primary abdominal pregnancy is an extremely rare form of ectopic pregnancy. Ectopic pregnancies that occur in the liver and diaphragm are even rarer, limited case reports are available in the literature.
A woman of childbearing age was transferred to the emergency department due to lumbar and abdominal pain radiating to the back toward the lower right. After a series of physical and auxiliary examinations, she was clinically diagnosed with hepatic ectopic pregnancy. Laparoscopic surgery was performed to remove the pregnancy tissue and achieve hemostasis. After a period of follow-up, the patient was successfully cured.
Paying attention to the patient's signs and utilizing imaging examination methods can help avoid missed diagnoses of liver pregnancy.
Core Tip: Liver pregnancy is an extremely rare type of ectopic pregnancy. Timely and accurate diagnosis can prevent the threat of death due to pregnancy-related complications. This case mainly discusses the diagnosis of liver pregnancy from various aspects, including the patient's symptoms, physical examination, and imaging studies. In particular, Multidisciplinary joint discussion and the use of magnetic resonance imaging to determine the exact location of the pregnancy can provide diagnosis and treatment recommendations for the disease.
- Citation: Yang XC, Fang M, Peng YG, Wang L, Ju R. Hepatic ectopic pregnancy with hemorrhage secondary diaphragmatic adhesion: A case report. World J Hepatol 2024; 16(9): 1289-1296
- URL: https://www.wjgnet.com/1948-5182/full/v16/i9/1289.htm
- DOI: https://dx.doi.org/10.4254/wjh.v16.i9.1289
When a gestational sac is implanted in the peritoneal cavity outside the uterine cavity or fallopian tube, we define this phenomenon as abdominal pregnancy. It is a rare ectopic pregnancy that occurs in about 1% of patients. The implant sites include the omentum, peritoneum of the pelvic and abdominal cavity, uterine surface, and abdominal organs[1].
It can be divided into primary abdominal pregnancy and secondary abdominal pregnancy. Primary abdominal preg
A woman in her 30s was transferred to the emergency department due to lumbar and abdominal pain radiating to the back toward the lower right.
The patient experienced abdominal pain for half a day, with no previous discomfort. The emergency abdominal computed tomography (CT) scan revealed a slightly higher density mixed lesion beneath the capsule of the right lobe of the liver, as well as pelvic fluid.
The patient has a good overall health condition with no significant medical history.
Menstrual status: Menarche at the age of 14. The patient has regular menstrual cycles with a duration of 30 days and a menstrual period lasting 5 days. The last menstrual period was on September 13, 2023. Marital and reproductive history: The patient is married and has given birth to a full-term baby girl through a normal delivery (natural conception). The patient has also had one previous induced abortion (The pregnancy was achieved through assisted reproductive technology).
The patient denies any family history of hereditary mental illness or malignant tumors.
On physical examination, the vital signs were as follows: Body temperature, 36.5 °C; Heart rate, 85 bpm; Non-invasive, blood pressure, 121/74 mmHg; Respiratory rate, 22 breathes per minute; Oxygen saturation, 98% under breathing ambient air.
The abdomen is soft, with significant tenderness in the right upper quadrant and no muscle guarding. No abnormalities were found during the gynecological examination.
The patient was admitted to emergency intensive care unit and more tests were performed. Her hemoglobin on admission was 133 g/L (reference range 115-150 g/L) (Table 1), β-human chorionic gonadotropin (β-HCG) was 2244 mIU/mL (reference range 0-20 mIU/mL). After 48 hours, her repeat β-HCG had increased to 3166 mIU/mL (Table 2), progesterone was 10.20 ng/mL and hemoglobin falled to 97 g/L (Table 1).
| Time | Hemoglobin (g/L) |
| Admission | 133 |
| 24 hours later | 109 |
| 48 hours later | 97 |
| Date | β-HCG (mIU/mL) |
| September 29, 2023 | 2244 |
| October 2, 2023 | 3166 |
| October 4, 2023 | 521 |
| October 18, 2023 | 9.3 |
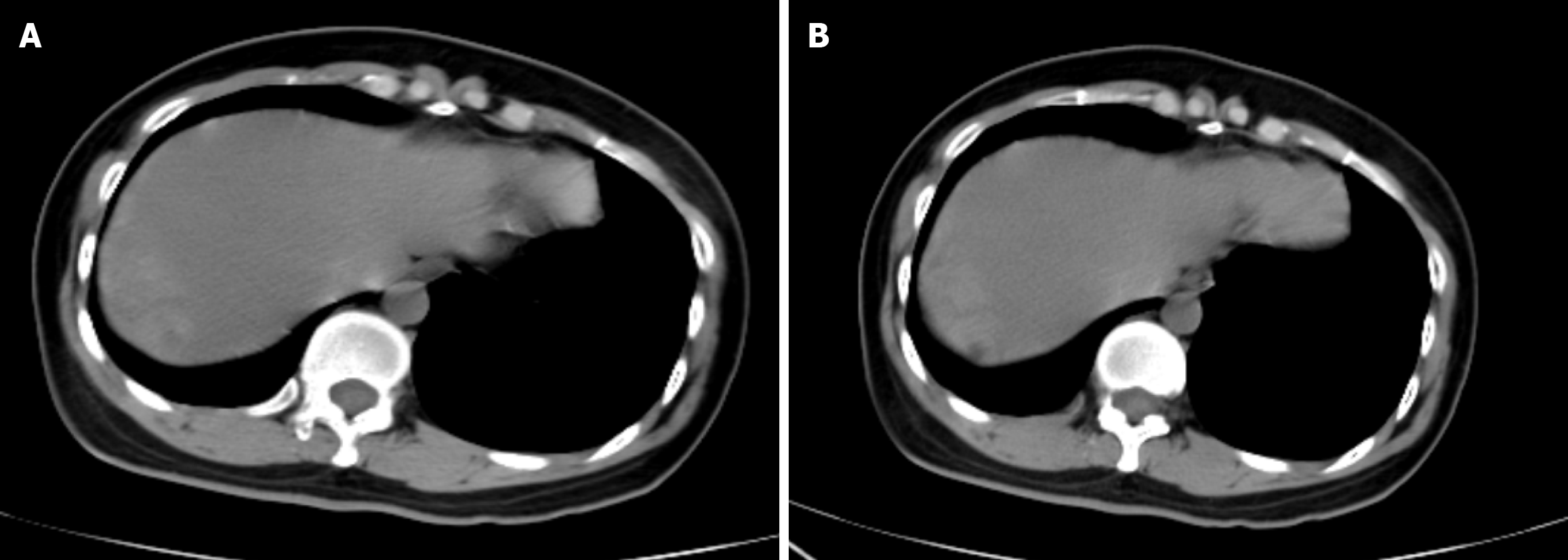
In the emergency room, the CT of the abdomen and pelvic scan showed pelvic effusion and mixed hyperintensity density (Figure 1A), which was initially considered a hepatic subcapsular hematoma. On the next slice, a decreased density was observed on the edge of the liver (Figure 1B).
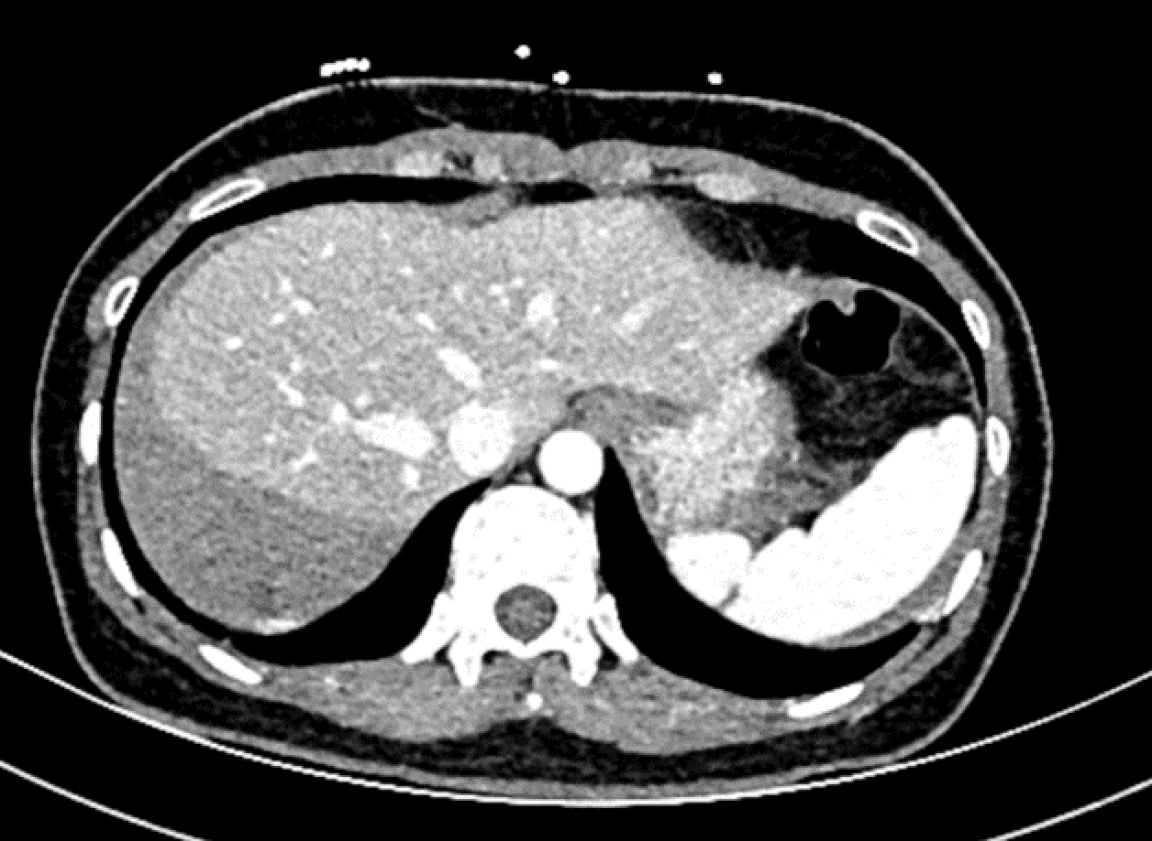
The next day, an enhanced CT scan was performed and showed no obvious enhancement around the lesion, but the hematoma had increased (Figure 2).
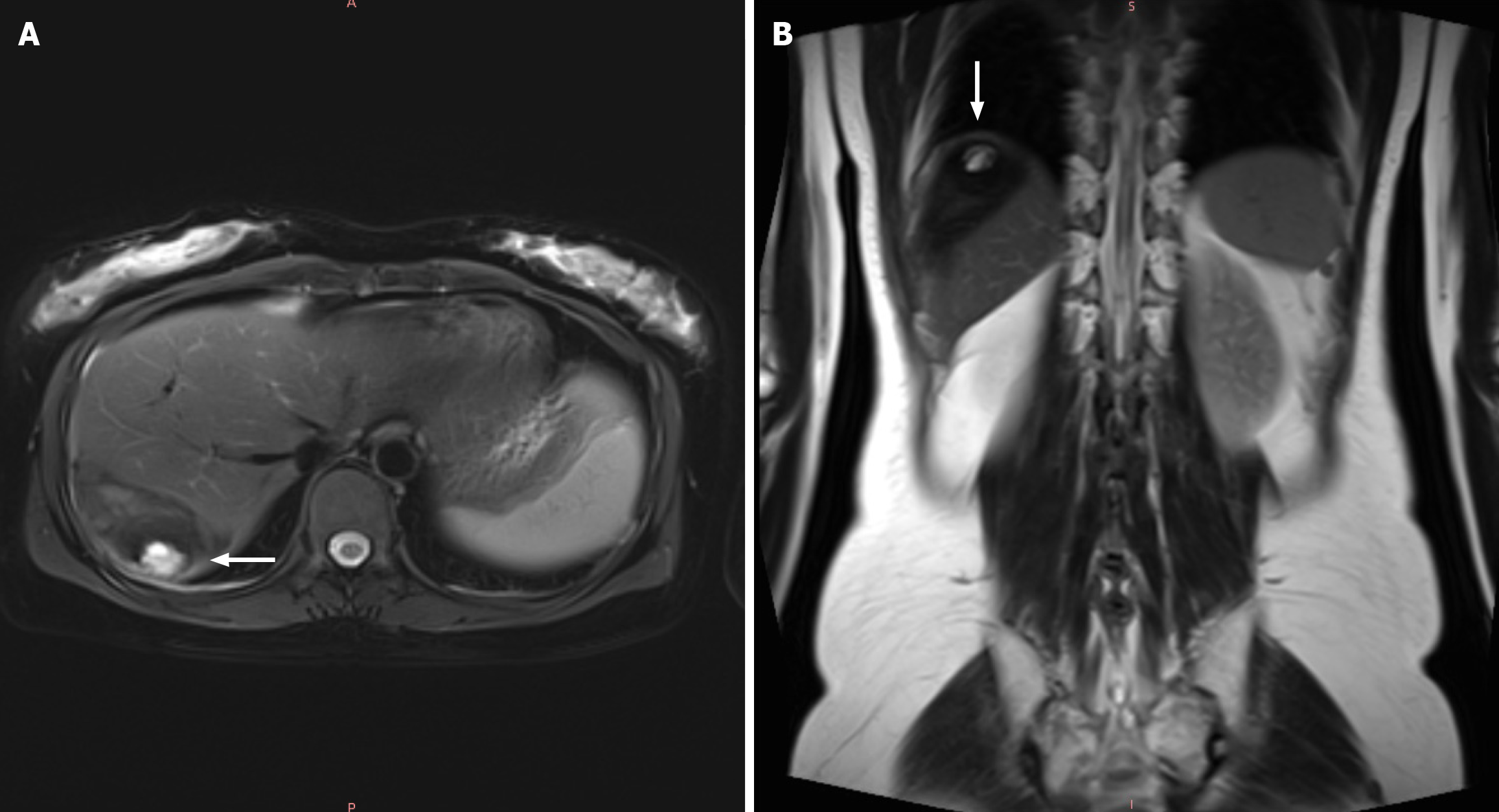
A transvaginal ultrasound was performed again, revealing no intrauterine pregnancy. The hemodynamics of the patient were stable. A magnetic resonance imaging (MRI) scan was performed, and T2-weighted imaging showed a low signal under the capsule of right lobe of the liver with a quasi-circular high signal inside, with a diameter of 20 mm (Figure 3A). However, in the coronal view, the lesion seemed closer to the diaphragm (Figure 3B).
Hepatic ectopic pregnancy.
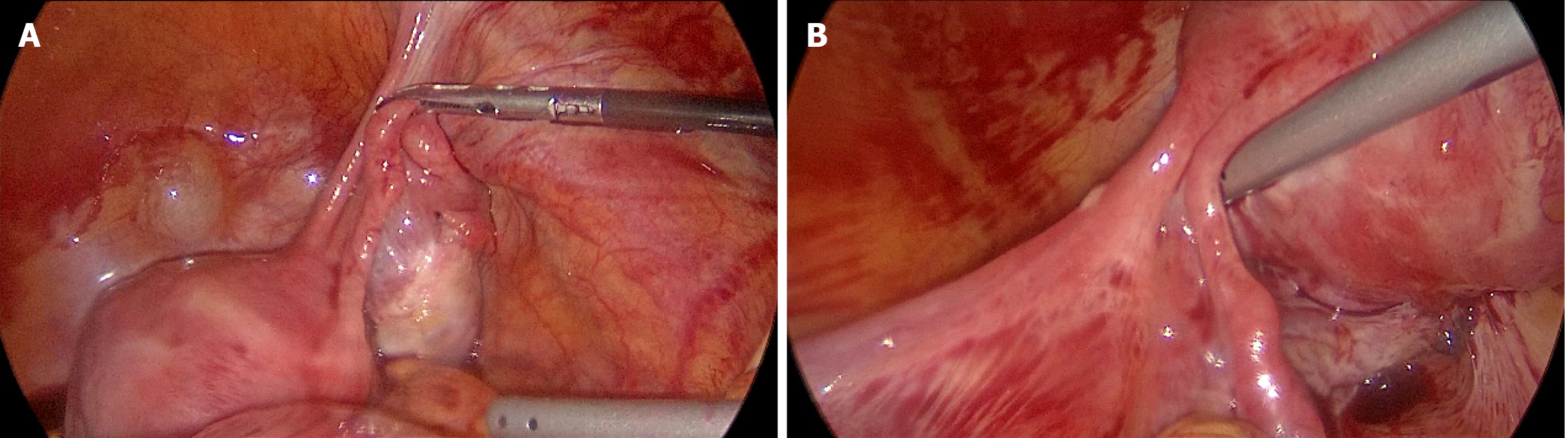
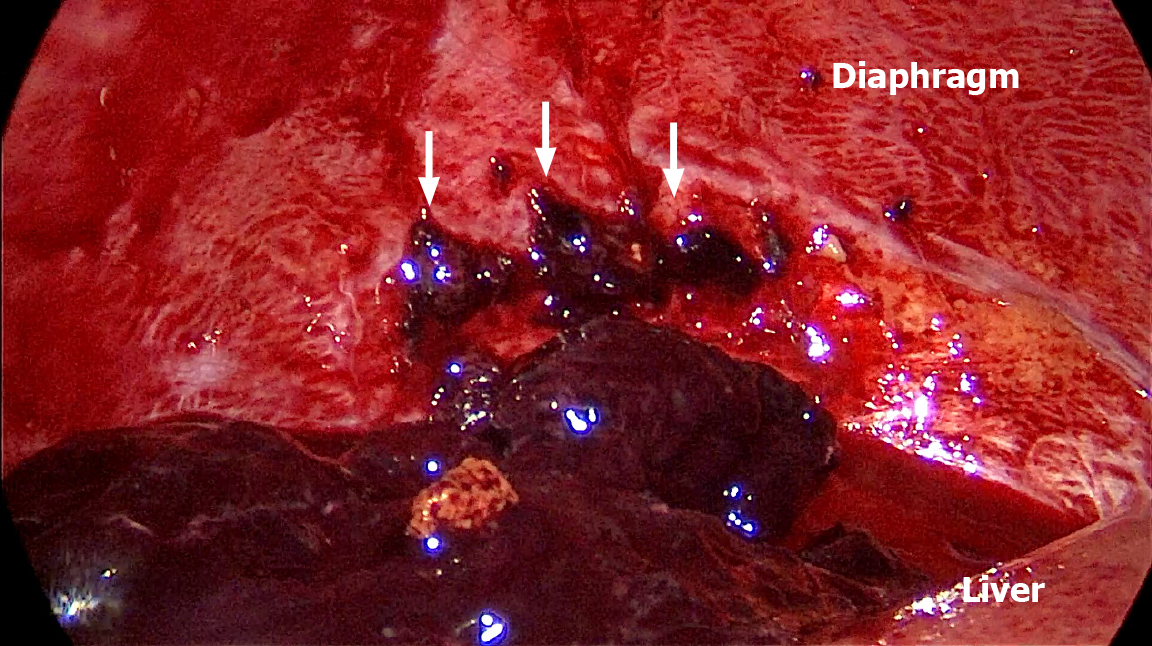
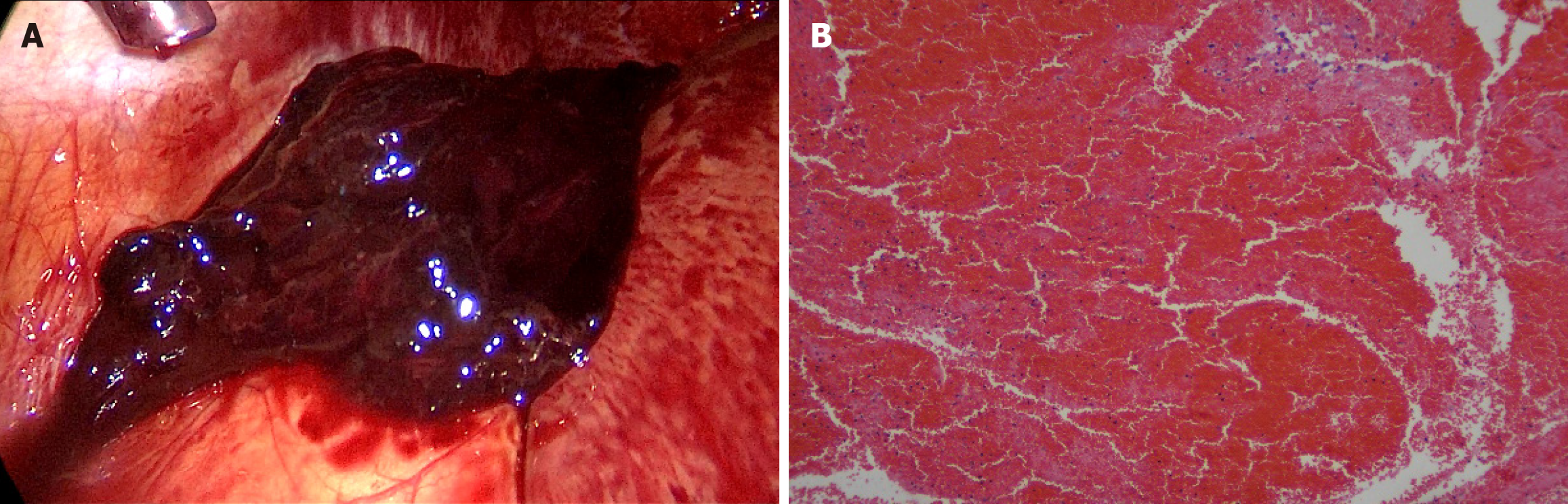
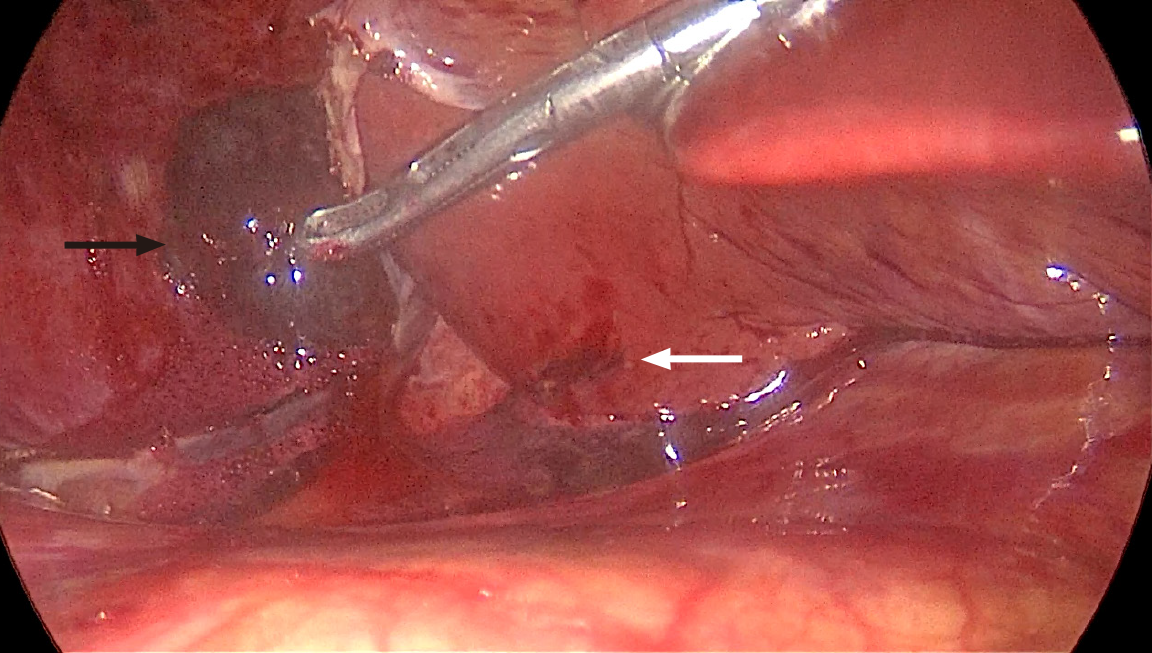
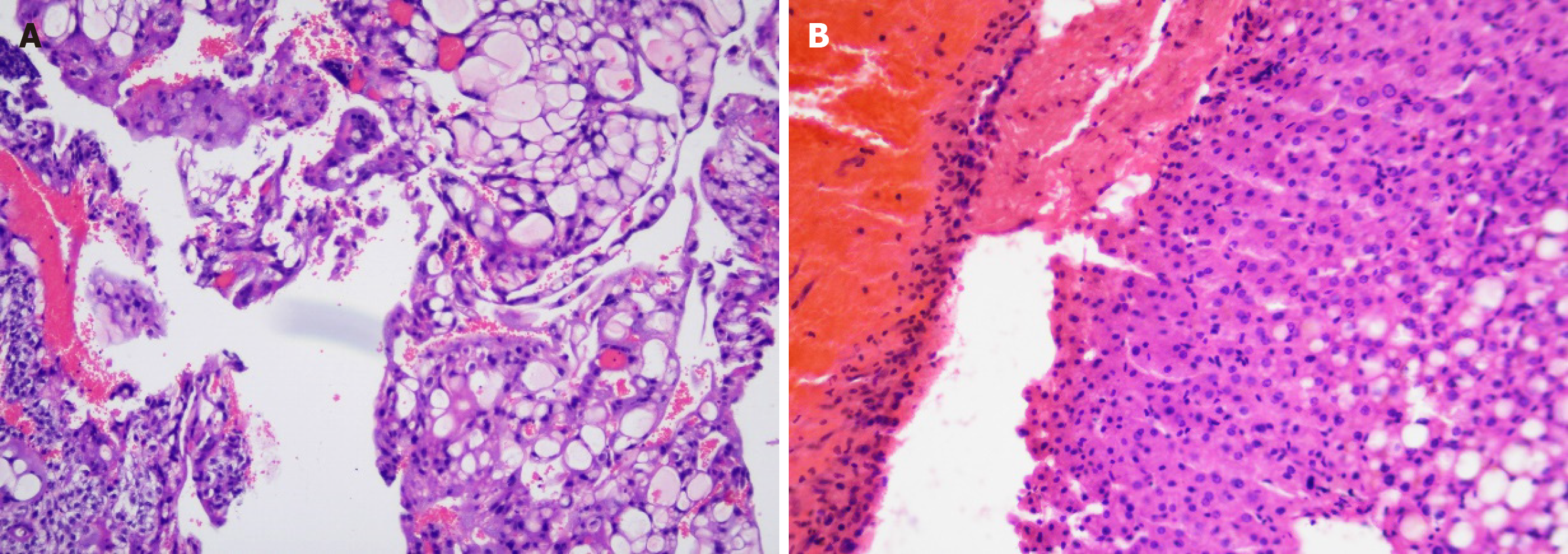
After a multidisciplinary discussion, laparoscopic exploration was performed. Exploration of the uterine adnexa revealed no abnormalities (Figure 4). Laparoscopy revealed blood accumulation in the abdomen of about 600 mL. After cleaning out the hematocele, no subcapsular hematoma was found in the liver. There was a small amount of adherent tissue and a minor bleeding on the diaphragm surface; the tissue was removed and sent for rapid pathological examination (Figure 5). The surrounding clot was removed and sent for rapid pathological examination (Figure 6). A tear of about 1 cm was found in the 6th segment of the visceral surface of the liver with local bleeding, which was the embryo implantation site. A gray tissue mass about 2 cm below was removed and sent for rapid pathology (Figure 7). Rapid pathologic examination confirmed that trophoblast cells and a small amount of liver tissue were found in the first tissue (Figure 8). Villus tissue was found in the third tissue (Figure 9).
The surgeon performed local electrocoagulation on the liver and the surface of the diaphragm. The surgeon explored the pelvis and found no abnormalities in the uterus, fallopian tubes, or ovaries. The final postoperative diagnosis of the patient was diaphragmatic adhesion secondary to liver ectopic pregnancy loss, indicating that means the case was a primary abdominal pregnancy.
Her β-HCG after 24 hours fell to 521.0 mIU/mL. A week after discharge, her repeated β-HCG fell to 9.3 mIU/L. She has been back to her work for three months and her menstruation became regular again.
The subcapsular hematoma of the liver is usually secondary to trauma, especially blunt injury. Spontaneous subcapsular bleeding of the liver is often associated with tumors, coagulation disorders, and other diseases, and rarely occurs. In obstetrics and gynecology, HELLP syndrome can cause spontaneous liver subcapsular hematoma. The incidence of HELLP syndrome is about 0.5%-0.9%, with clinical manifestations of hemolysis, elevated liver enzymes, and thrombocytopenia. Hepatic subcapsular hemorrhage is one of the complications of HELLP syndrome, with an incidence of 0.9%-2%[3]. Tidjane et al[4] have reported that liver subcapsular hemorrhage is related to coronavirus disease 2019 (COVID-19) infection, mainly because COVID-19 can cause coagulation dysfunction.
In this case, the CT scan, enhanced CT scan, and MRI all revealed bleeding under the liver capsule. The surgical procedure confirmed that the hemorrhage had accumulated under the diaphragm and outside the liver envelope. This deviation is related to local tissue anatomy. The space between the liver and diaphragm was narrow. After pregnancy, the fertilized eggs migrate from the abdominal cavity to the surface of the liver for implantation. The embryo tissue is not deeply implanted, eventually falling off on the surface of the liver, resulting in liver rupture and bleeding. The decidua and the shed embryonic tissue adhered to the diaphragm and formed adhesions. With the increase of local accumulation of blood, blood clots were formed, which play a local compression role. At the same time, the liver and diaphragm pressed against each other, slowing the bleeding rate, the local wrapping was formed, forming the illusion of bleeding under the liver capsule.
If a primary abdominal pregnancy is diagnosed, three conditions are required: (1) Both the fallopian tubes and ovaries are normal, with no recent evidence of pregnancy; (2) There is no formation of utero peritoneal fistula; and (3) The pregnancy is only present in the abdominal cavity, without the possibility of tubal pregnancy. The risk factors of ectopic pregnancy include tubal infection, surgery, smoking, assisted reproduction, pelvic inflammation, endometriosis, multiparity and unknown causes[1,5]. For this patient, the history of in-vitro fertilization treatment and curettage Increased the risk of ectopic pregnancy.
Most abdominal ectopic pregnancy occur in highly vascularized organs, and the liver qualifies. Based on the CT scan, we inferred liver ectopic pregnancy secondary to subcapsular hemorrhage. However, during laparoscopic exploration, no subcapsular hematoma was found in the liver. We only found a small amount of adherent tissue on the surface of diaphragm, which was smooth with no significant active bleeding. The tear was about 1 cm in the 6th segment of the visceral surface of the liver, secluded and with local bleeding. The surgeon was an experienced hepatobiliary surgeon, and the visual field was clearly exposed to rule out the possibility of intraoperative injury. We judged that the location was where the embryo implanted. The postoperative pathological examination revealed liver components in the tissue, confirming our theory: The embryo first implanted in the liver, then fell off and finally adhered to the diaphragm, failing to implant. Due to the lack of vascularization in diaphragm, the pregnancy ended in miscarriage. Because the blood clots formed played a local compression role, the bleeding rate slowed. The patient arrived at the hospital in good time, and under active treatment, her vital signs and hemodynamics were stable throughout. The patient’s lack of an obvious history of menopause was probably related to early ovulation.
Several cases have been reported in which the ectopic pregnancy could be diagnosed by CT, ultrasound, MRI and Positron emission tomography (PET)/computed tomography[6,7]. In this case, the CT scan was not sensitive enough to make a diagnosis. Although ultrasound is a purposeful option, certain locations of pregnancy may sometimes be missed. MRI is more specific and sensitive. Based on the mechanism of fluorodeoxyglucose PET/CT, the gestational sac implantation site may be accurately recognized by the metabolism scan. However, PET/CT and MRI are only useful for patients with stable hemodynamics. In terms of the accessibility and convenience, the CT scan is still the first choice for ruptured ectopic pregnancy in particular locations.
The therapies of ectopic pregnancy include surgery (laparoscopy or/and laparotomy), drugs (Methotrexate, Mifepristone etc.), or a combination of surgery and drugs[1]. Adequate disease analysis and discussion are important measures to ensure patients receive effective treatment. Preoperative evaluation is required. If abdominal pregnancy causes bleeding, doctors usually treat it surgically.
Primary abdominal pregnancy has a very low incidence rate, especially when it occurs in solid organs such as the liver. Preoperative abdominal ultrasound, CT, MRI, and other imaging examinations are crucial in determining the location of the ectopic pregnancy, assessing the severity of the condition, and deciding on the treatment plan.
| 1. | Dunphy L, Boyle S, Cassim N, Swaminathan A. Abdominal ectopic pregnancy. BMJ Case Rep. 2023;16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 2. | Sokalska A, Rambhatla A, Dudley C, Bhagavath B. Nontubal ectopic pregnancies: overview of diagnosis and treatment. Fertil Steril. 2023;120:553-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Haram K, Svendsen E, Abildgaard U. The HELLP syndrome: clinical issues and management. A Review. BMC Pregnancy Childbirth. 2009;9:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 300] [Cited by in RCA: 323] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 4. | Tidjane A, Laredj A, Boudjenan-Serradj N, Bensafir S, Tabeti B. A giant spontaneous subcapsular hematoma of the liver revealing a COVID-19 infection, a coincidence? (A case report). Pan Afr Med J. 2021;38:142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 5. | Farquhar CM. Ectopic pregnancy. Lancet. 2005;366:583-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 328] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 6. | Cai YY, Xiao EH, Shang QL, Xiao LZ. Ectopic pregnancy in the liver incidentally diagnosed by imaging: A case report. Exp Ther Med. 2017;14:373-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Hao J, Cheng Z, Hu N, Xiao L, Wang Y. Imaging of Hepatic Ectopic Pregnancy by 18F-FDG PET/CT. Clin Nucl Med. 2016;41:697-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |