Published online Jun 27, 2024. doi: 10.4254/wjh.v16.i6.951
Revised: April 29, 2024
Accepted: June 4, 2024
Published online: June 27, 2024
Processing time: 149 Days and 1 Hours
Nonalcoholic fatty liver disease (NAFLD) is a liver condition that is prevalent worldwide and associated with significant health risks and economic burdens. As it has been linked to insulin resistance (IR), this study aimed to perform a bibliometric analysis and visually represent the scientific literature on IR and NAFLD.
To map the research landscape to underscore critical areas of focus, influential studies, and future directions of NAFLD and IR.
This study conducted a bibliometric analysis of the literature on IR and NAFLD indexed in the SciVerse Scopus database from 1999 to 2022. The search strategy used terms from the literature and medical subject headings, focusing on terms related to IR and NAFLD. VOSviewer software was used to visualize research trends, collaborations, and key thematic areas. The analysis examined publication type, annual research output, contributing countries and institutions, funding agencies, journal impact factors, citation patterns, and highly cited references.
This analysis identified 23124 documents on NAFLD, revealing a significant increase in the number of publications between 1999 and 2022. The search retrieved 715 papers on IR and NAFLD, including 573 (80.14%) articles and 88 (12.31%) reviews. The most productive countries were China (n = 134; 18.74%), the United States (n = 122; 17.06%), Italy (n = 97; 13.57%), and Japan (n = 41; 5.73%). The leading institutions included the Università degli Studi di Torino, Italy (n = 29; 4.06%), and the Consiglio Nazionale delle Ricerche, Italy (n = 19; 2.66%). The top funding agencies were the National Institute of Diabetes and Digestive and Kidney Diseases in the United States (n = 48; 6.71%), and the National Natural Science Foundation of China (n = 37; 5.17%). The most active journals in this field were Hepatology (27 publications), the Journal of Hepatology (17 publications), and the Journal of Clinical Endocrinology and Metabolism (13 publications). The main research hotspots were “therapeutic approaches for IR and NAFLD” and “inflammatory and high-fat diet impacts on NAFLD”.
This is the first bibliometric analysis to examine the relationship between IR and NAFLD. In response to the escalating global health challenge of NAFLD, this research highlights an urgent need for a better understanding of this condition and for the development of intervention strategies. Policymakers need to prioritize and address the increasing prevalence of NAFLD.
Core Tip: Although numerous bibliometric studies have investigated insulin resistance (IR) and nonalcoholic fatty liver disease (NAFLD), few studies have explored the correlation of these two conditions. As explained here, understanding the interplay between IR and NAFLD is crucial for enhancing patient health outcomes. Consequently, this study aimed to perform a bibliometric analysis and visually represent the scientific literature pertaining to IR and NAFLD. Through mapping the research landscape, the study also aimed to emphasize key areas of focus, influential works, and potential future directions.
- Citation: Zyoud SH, Hegazi OE, Alalalmeh SO, Shakhshir M, Abushamma F, Khilfeh S, Al-Jabi SW. Mapping the global research landscape on nonalcoholic fatty liver disease and insulin resistance: A visualization and bibliometric study. World J Hepatol 2024; 16(6): 951-965
- URL: https://www.wjgnet.com/1948-5182/full/v16/i6/951.htm
- DOI: https://dx.doi.org/10.4254/wjh.v16.i6.951
Nonalcoholic fatty liver disease (NAFLD) is the most common cause of chronic liver disease worldwide[1]. NAFLD is defined as a spectrum of disorders that, in the absence of a secondary cause (e.g., excessive alcohol consumption), share the characteristic of hepatic stenosis. A 2022 study concluded that NAFLD impacts the lives of more than 47 individuals per 1000 people, with another study from the same year projecting that NAFLD will affect more than half the population by 2040[1,2]. Taken together, these findings indicate that NAFLD is a significant public health concern that necessitates immediate action as uncontrolled NAFLD can progress to severe conditions, such as hepatocellular carcinoma, and is coupled with an increase in the risk of cardiovascular diseases that substantially increases the risk of mortality[3,4]. The effect of NAFLD is not limited to an increased risk of mortality. The direct and indirect costs of managing the condition alongside the loss of productivity of its patients are substantial[5]. In the United States alone, NAFLD expenditures can reach 103 billion USD; this excludes its complications, which, if considered, can increase the costs to more than 908 billion USD[6,7].
Other conditions, such as type 2 diabetes mellitus, metabolic syndrome, and obesity, have also been on the rise over the last few decades. This is not surprising given that these conditions are not independent; rather they are associated with one another in various ways[8,9]. For example, patients with NAFLD and obesity often have increased intraabdominal fat, which is hypothesized contributes to insulin resistance (IR). This resistance may lead to increased delivery of free fatty acids to the liver, stimulating lipogenesis and aggravating hepatic steatosis. Conversely, in rat models, fat accumulation in the liver might be the primary cause of hepatic IR[10]. Furthermore, hepatic insulin sensitivity is improved in individuals who consume a diet intended to reduce hepatic fat[11].
Diet, lifestyle, and inflammatory cytokines all have major effects on IR. Currently, insulin sensitizers and lifestyle alterations are essential for managing and treating this illness. The use of insulin receptor cascade regulators and fresh perspectives on the prevention and treatment of primary IR are examples of future therapeutic targets. However, new discoveries have led to an improved understanding of insulin signaling and the mechanisms underlying IR. Additionally, sedentary lifestyles, high-fat and refined-carbohydrate diets, and inflammatory cytokines have all been connected to IR[12-14]. Among the endocrine disorders associated with this illness are obesity, type 2 diabetes, hypercholesterolemia, hypertriglyceridemia, and arterial hypertension[12]. An ideal lifestyle and, in the case of obesity, weight loss is the most crucial treatment component[14,15]. For instance, it has been clinically demonstrated that metformin causes insulin sensitization in high-risk individuals. With the use of laboratory concepts related to insulin and glucose, the disease was discovered and confirmed to be a significant entity in metabolism. This work is currently being conducted and put into practice[16]. Research has investigated the relationship between IR and the development of cardiometabolic disorders[17,18]. Realistic therapeutic targets were identified after a thorough analysis of insulin signaling and IR mechanisms[19]. Additionally, as possible therapeutic targets for the treatment of IR, researchers are investigating the actions of insulin receptor cascade regulators[19]. Research is being conducted to learn more about the functions of the intestinal microbiota, peroxisome proliferator-activated receptors, autonomic nervous system, endocrine hormones, and vitamin D deficiency in the prevention and management of IR[17].
There is currently no Food and Drug Administration-approved treatment for NAFLD. However, management strategies have been proposed. One popular strategy is weight loss, with studies showing that a reduction of up to 5% in body weight improves liver fat content and fibrosis[4,20]. Some pharmacological agents have been suggested, but all remain under investigation. For example, metformin has yielded varying results in improving the liver conditions associated with NAFLD. Some studies have reported improved liver function[21,22], but others have shown no significant changes[23,24]. Another proposed class of pharmacological agent is thiazolidinediones, which have demonstrated the potential to improve liver function and decrease hepatic fat content in nonalcoholic steatohepatitis patients[25-27]. Other treatments, such as statins, omega-3 fatty acids, and antioxidant therapies, have shown mixed results[28-31].
It is essential to review and analyze existing studies to understand the current trends and gaps in research on the relationship between IR and NAFLD. A bibliometric analysis, which uses statistical methods to examine research publications, can help. This approach provides an overview of significant developments, major contributors, and notable papers. In addition, visualization techniques can reveal research and collaboration patterns and central themes resulting from the bibliometric analysis[32-34].
Numerous studies have examined research trends within the microbiota and liver, encompassing various diseases[35-42]. While there have been several studies on IR[43-45] and NAFLD[46-49], few have explored the relationship between them. Understanding the relationship between IR and NAFLD is essential for improving patient health outcomes. Thus, this study aimed to conduct a bibliometric analysis and to visualize the scientific literature on IR and NAFLD. By mapping the research landscape, this study highlights critical areas of focus, influential works, and future directions.
This comprehensive cross-sectional analysis used bibliometric methods to analyze publications addressing IR and NAFLD that were published between 1999 and 2022.
The progression and expansion of the literature concerning IR and NAFLD were examined in publications retrieved from the SciVerse Scopus database. The use of this database is justified for several reasons[50-55]. First, Scopus includes more than 30000 indexed journals across health and the social, life, and physical sciences. Second, SciVerse entirely includes PubMed journals and surpasses the Web of Science the number of indexed journals. Third, Scopus offers various features that streamline bibliometric analysis. It is important to note that this database is biased toward publications from English-speaking countries and English-language journals[56]. As, the Web of Science faces a similar bias issue, Scopus was the most pragmatic choice. For these reasons, Scopus is widely regarded as exceptionally comprehensive because it encompasses publications from both PubMed and Web of Science[53,54].
A comprehensive literature search was conducted using the Scopus database to identify relevant studies investigating the association between IR and NAFLD. The search included publications up to December 31, 2022. It was conducted on November 17, 2023 to ensure that all relevant research items were retrieved and to reduce bias from database updates. Multiple broad terms and phrases were used to ensure that all IR and NAFLD research was retrieved.
The data for this study were extracted according to the following steps. Step 1: A group of search terms related to NAFLD was used. The terms were extracted from existing systematic reviews, meta-analyses, and medical subject headings from PubMed. For article retrieval, the terms were then inserted into the “Article Title” field of the Scopus search engine. Step 2: The retrieved publications were further refined by restricting the scope to those containing “IR and associated terms” within their titles. Terms pertaining to IR were meticulously selected from a collection of previous systematic reviews and meta-analyses[57-59]. Subsequently, the terms “IR” and “insulin sensitivity” were used as search criteria within the article titles. Step 3: The research deliberately restricted its focus to scientific journal articles, meticulously excluding nonscholarly publications such as books, book chapters, retracted articles, and errata.
The investigation substantiated the search query by applying two distinct criteria. Two experts specializing in bibliometric sciences assessed the top 50 most common documents and documents with even numerical identifiers (55, 60, 65, 70, etc) in the retrieved document list. The experts scrutinized the documents in an Excel spreadsheet to identify false-positive results. In instances of disagreement, the principal investigator adjudicated the final judgment. The absence of false-positive results served as the validity indicator, and the author iteratively refined the search query until both reviewers concurred on its absence.
After this validation, the experts were instructed to compare the publication counts of the top 20 active authors with the number of articles attributed to each author, as documented in their respective Scopus profiles. The results obtained by both methods underwent correlation testing to assess significance and correlation. The correlation test revealed a robust correlation coefficient (r = 0.976), and the statistical significance (P < 0.001) emphasized the precision of the search query. This dual-method approach aimed to confirm the absence of false-negative outcomes, drawing inspiration from established bibliometric studies[60,61]. Notably, the inclusion of keywords in the title search, as opposed to a title/abstract search, was employed to enhance the reliability of the approach. Consequently, the title search method emerged as reliable, with minimal retrieval of false-positive documents. In contrast, the title/abstract search method[62-65] yielded numerous false positives that did not have a specific focus on IR and NAFLD.
This study systematically assigned the fundamental bibliometric indicators to four main classifications following established norms used in previous bibliometric analyses[66-69]. The four main classifications were: (1) Analysis of the research output and publication progress concerning IR and NAFLD, which included metrics such as the total number of articles, the year of publication, and the trends of the publications; (2) Identification of origin and study patterns in publications, which focused on identifying the countries that contributed substantially to the collective body of research; (3) Evaluation of publication productivity, which investigated the top prolific institutions and funding agencies actively involved in this field; and (4) Assessment of the quality of publication output, which examined the most frequently cited articles, citation patterns, the Hirsch index (h-index), and most prolific journals and their corresponding impact factors. The impact index per article was displayed for the top 10 highly cited papers sourced from the Reference Citation Analysis (RCA) database. RCA, an open multidisciplinary citation analysis database, is owned by Baishideng Publishing Group Inc. headquartered in Pleasanton, CA 94566, United States[70-72].
VOSviewer software (version 1.6.20; Van Eck & Waltman, www.vosviewer.com) was used to construct visual representations illustrating collaborations among countries via network maps[73-75]. To generate a term co-occurrence map in VOSviewer, only terms occurring at least 20 times in the title and abstract were considered under binary counting. The terms with the highest relevance scores were selected to construct a term map for network visualization. The algorithm was designed to ensure that terms with more frequent co-occurrences manifested as larger bubbles and that similar terms were positioned close together. A unique color was assigned to each term to visually represent the frequency of occurrence of each in the overlay. In contrast to yellow and green, which denote keywords that appeared more recently, blue was used to indicate keywords that appeared earlier in the time course[73-75].
A global search of publications between 1973 and 2022 revealed a substantial collection of 23124 NAFLD-related documents, as indicated in their titles. Among these scholarly works, 715 examined NAFLD and its association with IR from 1999 to 2022. Articles were the most prevalent form of NAFLD and IR literature, accounting for 573 publications (80.14%). A total of 88 reviews were found, representing 12.31% of the total. The remaining five publication types, which included letters, notes, editorials, meeting minutes, and brief surveys, accounted for 54 documents, or 7.56% of the total.
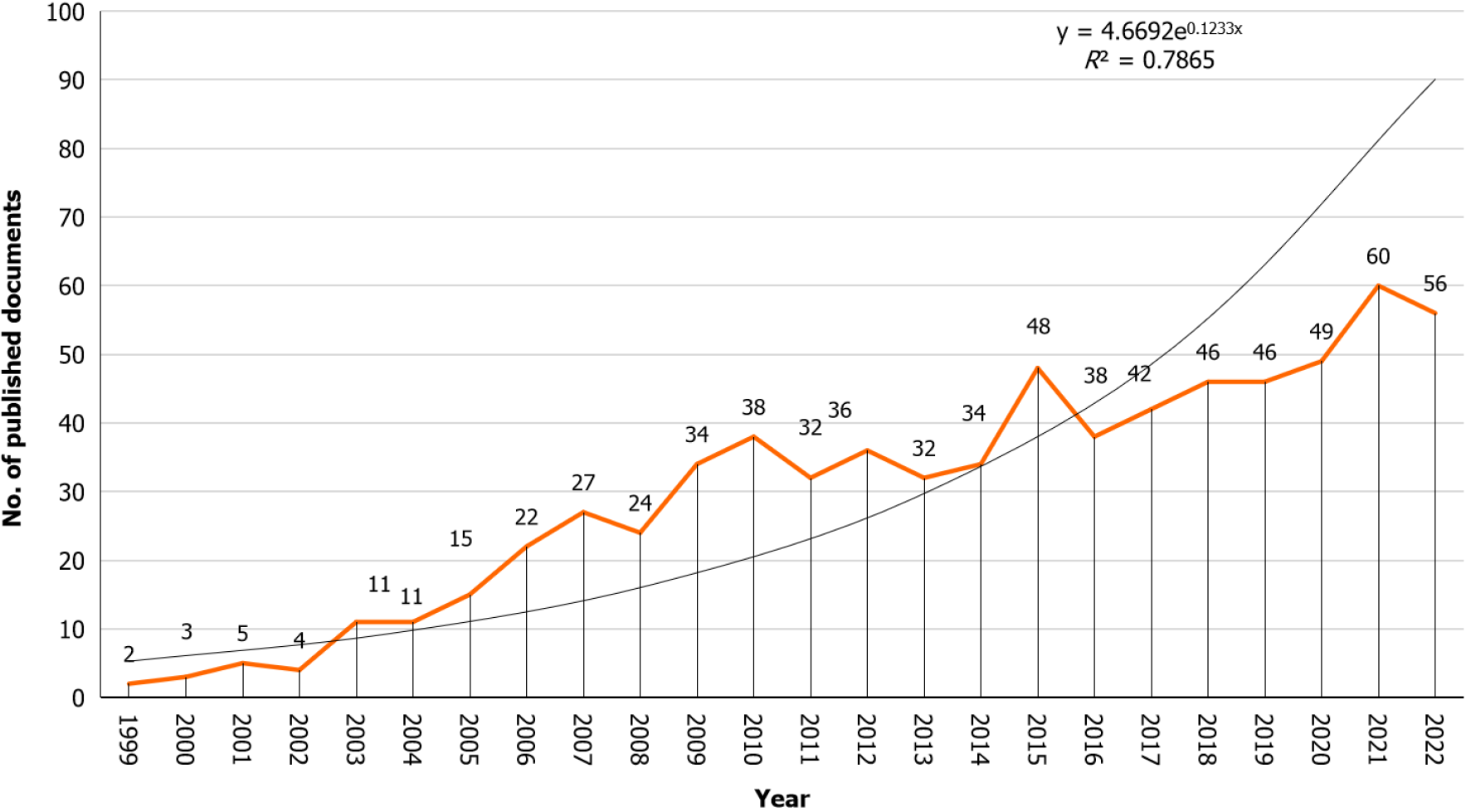
The volume of publications on IR and NAFLD has steadily increased from 1999 to 2022. This growth can be divided into two distinct phases. The first phase, spanning from 1999 to 2010, was characterized by rapid growth, and the second phase, from 2011 to 2022, had a more stable and consistent increase. Reflecting this trend, the average annual publication rate increased from 16.33 per year in the first phase to 43.25 per year in the second phase. Statistical analysis using linear regression confirmed this observation, revealing a modest positive correlation (R2 = 0.7865, P < 0.001) between the annual publication count and the corresponding year of publication (Figure 1).
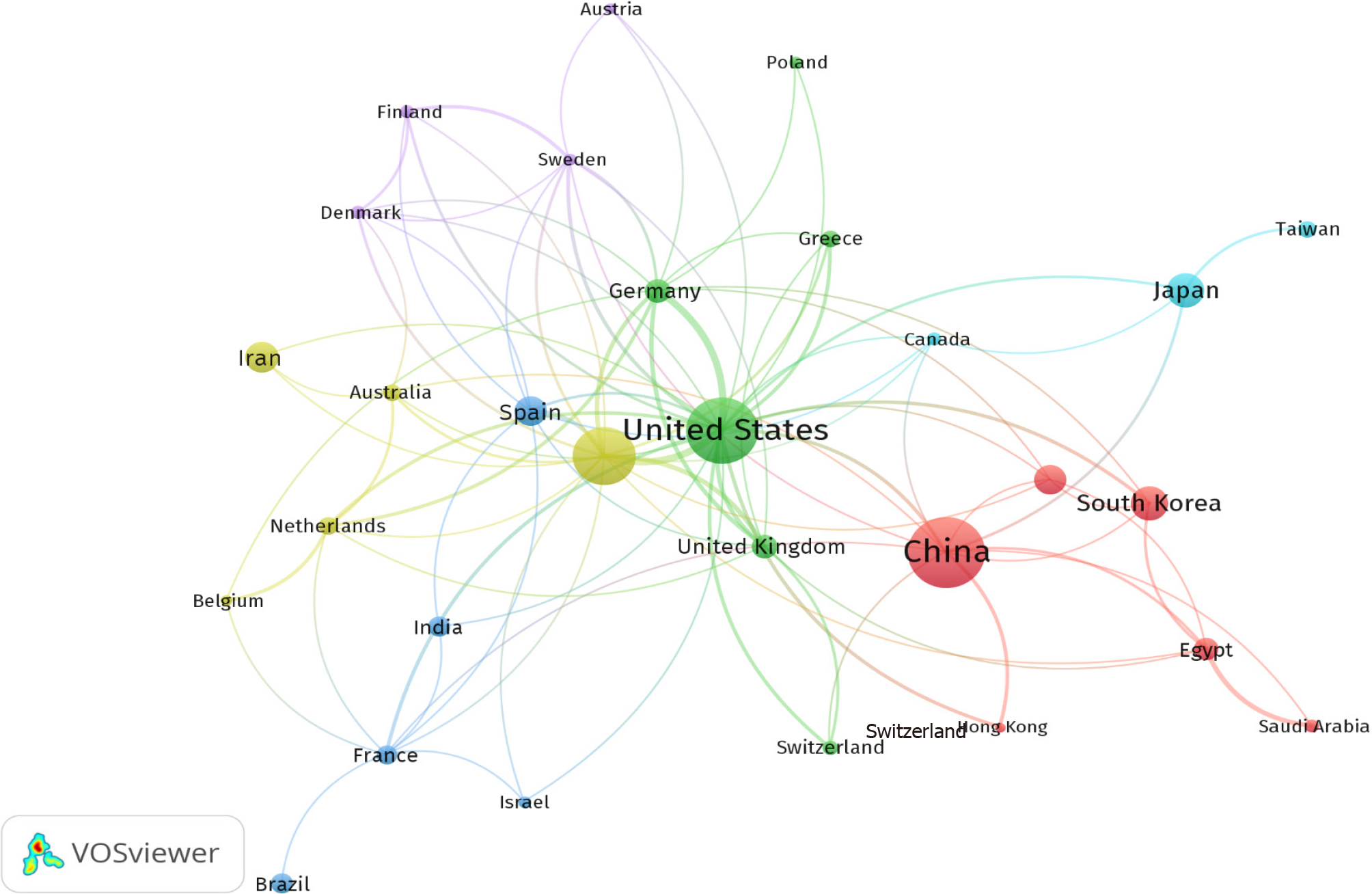
Between 1999 and 2022, more than 60 countries actively conducted and published studies on NAFLD and its correlation with IR. The top 10 countries collectively authored 524 articles, constituting 73.28% of all the contributions in this field (Table 1). Notably, China was the foremost contributor, with 134 articles (18.74%), followed by the United States, with 122 articles (17.06%); Italy, with 97 articles (13.57%); and Japan, with 41 articles (5.73%). Furthermore, the United States and China led in international collaboration, boasting the greatest number of publications involving scholars from various countries. For a visual representation of international research collaborations on IR and NAFLD from 1999 to 2022, refer to Figure 2, which shows a network map of the key participating countries.
| Ranking1 | Country | Number of documents | % |
| 1st | China | 134 | 18.74 |
| 2nd | United States | 122 | 17.06 |
| 3rd | Italy | 97 | 13.57 |
| 4th | Japan | 41 | 5.73 |
| 4th | South Korea | 41 | 5.73 |
| 6th | Iran | 35 | 4.90 |
| 7th | Spain | 32 | 4.48 |
| 8th | Turkey | 32 | 4.48 |
| 9th | Germany | 23 | 3.22 |
| 10th | United Kingdom | 23 | 3.22 |
Table 2 shows the 10 most productive institutes with publications on NAFLD and its association with IR from 1999 to 2022. These institutions collectively accounted for 12.30% (n = 88) of the published articles. The Università degli Studi di Torino in Italy was the most prolific contributor, with 29 articles (4.06%), followed by the Consiglio Nazionale delle Ricerche in Italy, with 19 articles (2.66%), and the Alma Mater Studiorum Università di Bologna in Italy, with 16 articles (2.24%). Italy had seven institutions on the list, the United States had two, and South Korea had one.
| Ranking1 | Institute | Country | No. of documents | % |
| 1st | Università degli Studi di Torino | Italy | 29 | 4.06 |
| 2nd | Consiglio Nazionale delle Ricerche | Italy | 19 | 2.66 |
| 3rd | Alma Mater Studiorum Università di Bologna | Italy | 16 | 2.24 |
| 4th | Sapienza Università di Roma | Italy | 13 | 1.82 |
| 5th | IRCCS Ospedale Pediatrico Bambino Gesù | Italy | 12 | 1.68 |
| 6th | Istituto di Fisiologia Clinica del CNR | Italy | 11 | 1.54 |
| 6th | SKKU School of Medicine | South Korea | 11 | 1.54 |
| 6th | Yale School of Medicine | United States | 11 | 1.54 |
| 9th | Università degli Studi di Milano | Italy | 10 | 1.40 |
| 10th | University of Florida | United States | 9 | 1.26 |
A total of 275 publications, accounting for 38.5% of the retrieved articles, were supported by funding. Table 3 lists the top 10 funding agencies associated with NAFLD and its correlation with IR from 1999 to 2022. These 10 agencies collectively contributed 19.86% (n = 142) of the published articles. The National Institute of Diabetes and Digestive and Kidney Diseases in the United States (n = 48; 6.71%) emerged as the most active funding agency in the field, followed by the National Natural Science Foundation of China (n = 37; 5.17%), and the National Institutes of Health in the United States (n = 31; 4.34%).
| Ranking1 | Funding agency | Country | No. of documents | % |
| 1st | National Institute of Diabetes and Digestive and Kidney Diseases | United States | 48 | 6.71 |
| 2nd | National Natural Science Foundation of China | China | 37 | 5.17 |
| 3rd | National Institutes of Health | United States | 31 | 4.34 |
| 4th | National Center for Research Resources | United States | 18 | 2.52 |
| 5th | Japan Society for the Promotion of Science | Japan | 17 | 2.38 |
| 6th | National Center for Advancing Translational Sciences | United States | 13 | 1.82 |
| 7th | Seventh Framework Programme | European Union’s | 10 | 1.40 |
| 8th | Horizon 2020 Framework Programme | European Union’s | 9 | 1.26 |
| 9th | Instituto de Salud Carlos III | Spain | 8 | 1.12 |
| 9th | National Heart, Lung, and Blood Institute | United States | 8 | 1.12 |
| 9th | United States Department of Veterans Affairs | United States | 8 | 1.12 |
Table 4 shows that the leading 10 journals/sources contributed 19.18% (n = 137) of the overall research publications focused on NAFLD and its correlation with IR. Hepatology [impact factor (IF) 14.0, 2022] had the most publications, with 27, followed by the Journal of Hepatology (IF 25.7, 2022), with 17, and the Journal of Clinical Endocrinology and Metabolism (IF 5.8, 2022), with 13.
| Ranking1 | Journal/source title | No. of documents | % | IF2 |
| 1st | Hepatology | 27 | 3.78 | 14.0 |
| 2nd | Journal of Hepatology | 17 | 2.38 | 25.7 |
| 3rd | Journal of Clinical Endocrinology and Metabolism | 13 | 1.82 | 5.8 |
| 3rd | Nutrients | 13 | 1.82 | 5.9 |
| 5th | Scientific Reports | 11 | 1.54 | 4.6 |
| 6th | Liver International | 10 | 1.40 | 6.7 |
| 6th | Chinese Journal of Hepatology | 10 | 1.40 | NA |
| 8th | American Journal of Gastroenterology | 9 | 1.26 | 10.2 |
| 8th | Plos One | 9 | 1.26 | 3.7 |
| 8th | World Chinese Journal of Digestology | 9 | 1.26 | NA |
| 8th | World Journal of Gastroenterology | 9 | 1.26 | 4.3 |
The collected articles had received a total of 42590 citations, with an average of 59.57 and an h-index of 99. Among these articles, 71 were not cited, and 96 had more than 100 citations. The citation count for these articles varied from 0 to 1826. Table 5 shows the top 10 publications on NAFLD and its association with IR, and they account for 9149 citations. The number of citations for these publications ranged from 545 to 1826[10,11,76-83]. The impact index per article of the 10 most cited articles ranged from 23.9 to 116.0 (Table 5).
| Ref. | Title | Year | Source title | Cited by | Impact index per article1 |
| Sanyal et al[76], 2001 | Nonalcoholic steatohepatitis: Association of insulin resistance and mitochondrial abnormalities | 2001 | Gastroenterology | 1826 | 62.4 |
| Marchesini et al[77], 1999 | Association of nonalcoholic fatty liver disease with insulin resistance | 1999 | American Journal of Medicine | 1331 | 42.0 |
| Jung and Choi[78], 2014 | Obesity and its metabolic complications: The role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease | 2014 | International Journal of Molecular Sciences | 1265 | 116.0 |
| Samuel et al[10], 2004 | Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease | 2004 | Journal of Biological Chemistry | 1062 | 47.1 |
| Pagano et al[79], 2002 | Nonalcoholic steatohepatitis, insulin resistance, and metabolic syndrome: Further evidence for an etiologic association | 2002 | Hepatology | 659 | 23.9 |
| Utzschneider and Kahn[11], 2006 | Review: The role of insulin resistance in nonalcoholic fatty liver disease | 2006 | Journal of Clinical Endocrinology and Metabolism | 657 | 32.6 |
| Musso et al[80], 2003 | Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis | 2003 | Hepatology | 627 | 24.2 |
| Gaggini et al[81], 2013 | Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease | 2013 | Nutrients | 594 | 49.7 |
| Bugianesi et al[82], 2005 | Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: Sites and mechanisms | 2005 | Diabetologia | 583 | 26.2 |
| Birkenfeld and Shulman[83], 2014 | Nonalcoholic fatty liver disease, hepatic insulin resistance, and type 2 Diabetes | 2014 | Hepatology | 545 | 49.8 |
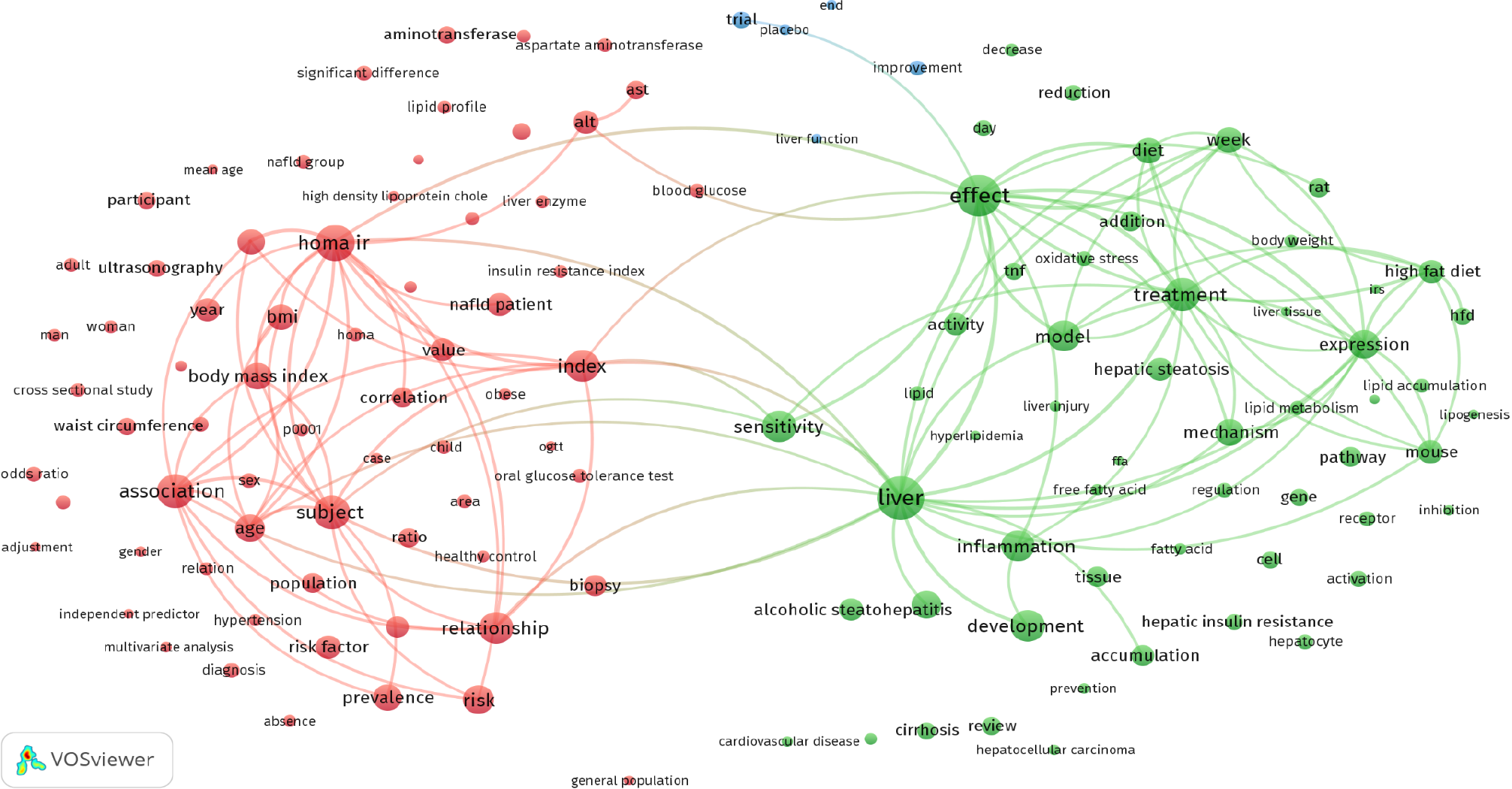
VOSviewer was used to perform a co-occurrence analysis of the title and abstract content of the publications, explicitly emphasizing IR and NAFLD (Figure 3). The resulting co-occurrence network revealed three distinct clusters representing the primary research priorities concerning IR and NAFLD. Each cluster was distinguished by different colors (red for cluster 1, green for cluster 2, and blue for cluster 3), and terms associated with specific research topics were included. Cluster 1 includes publications on “population health implications”, addressing IR and NAFLD’s significant population health ramifications in light of the global increase in obesity and metabolic disorders. Ongoing discussions center on public health strategies for prevention and management. Cluster 2 focused on “inflammation and high-fat diets”, exploring the potential contribution of high-fat diets, particularly those imbalanced in omega-3 and omega-6 fatty acids and those rich in highly saturated and trans fats, to inflammation, which is linked to IR and NAFLD. Cluster 3 publications addressed “therapeutic approaches”, emphasizing the challenge of developing effective therapeutic strategies for IR and NAFLD through clinical trials. The exploration included lifestyle interventions, pharmacological treatments, and novel therapies to manage and potentially reverse these conditions. Notably, the terms within each cluster have robust connections, underscoring the coherence of the research within these thematic areas.
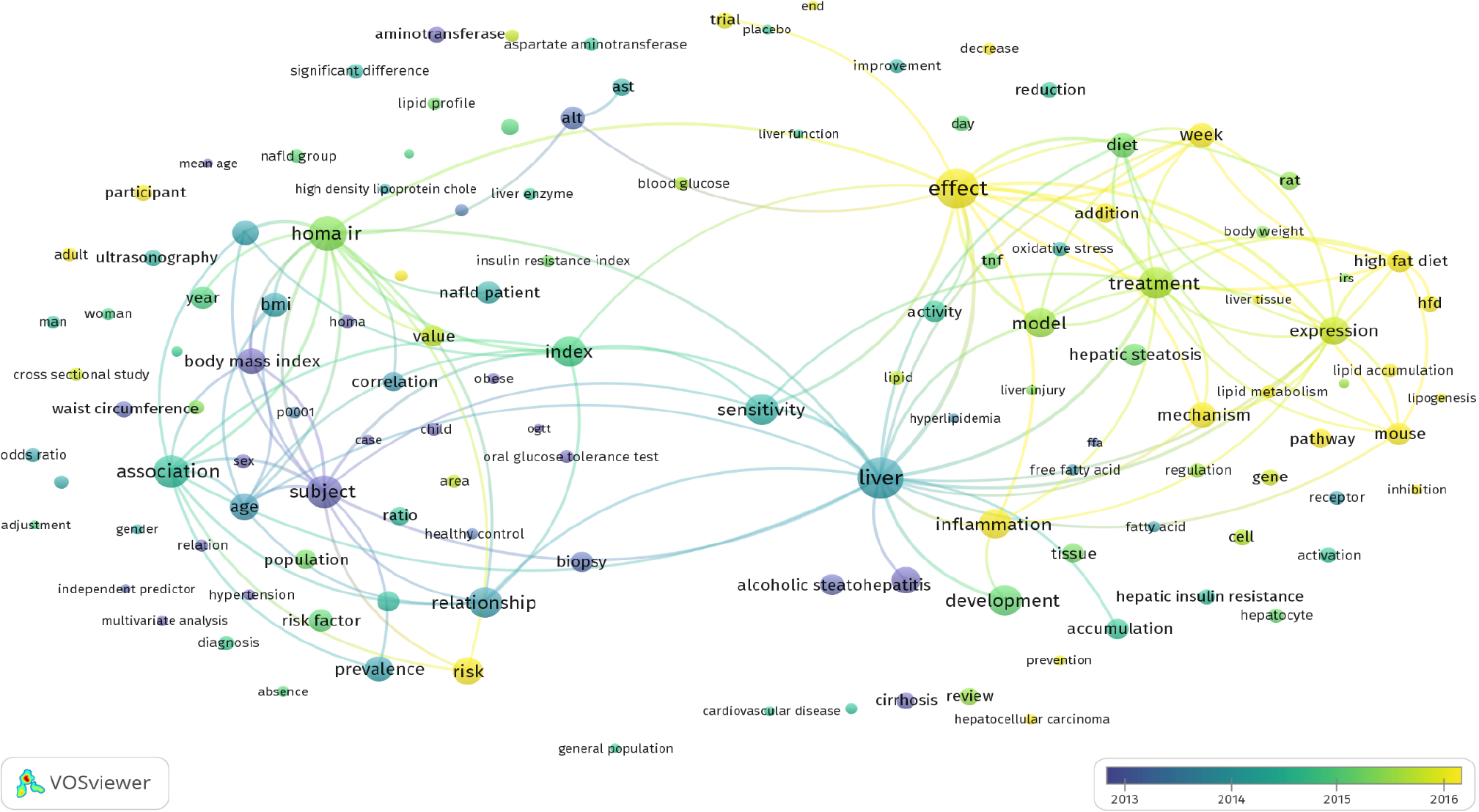
The term co-occurrence analysis (Figure 4) revealed evolving trends in publications on NAFLD and IR. Notably, recent studies (post-2015) investigated the effects of inflammation and a high-fat diet on the development of IR and NAFLD, as well as therapeutic approaches. These investigations underscore the challenge of devising effective therapeutic strategies, emphasizing the shift from earlier publications (pre-2015) that primarily focused on “population health implications”. These earlier works addressed the significant population health implications of IR and NAFLD in the context of the global rise in obesity and metabolic disorders.
This is the first bibliometric analysis to provide an overview of the NAFLD and IR research landscape. The study covered research published between 1999 and 2022, including research trends, collaborations, and main thematic areas. Additionally, publication type, annual research output, contributing countries and institutions, funding agencies, journal impact factors, citation patterns, and highly cited references were analyzed.
The analysis revealed that after 2011, there was a substantial increase in publication output, which could signify that this point marked the beginning of significant interest in the topic. This increase might also indicate that at that time, the scientific community began to recognize the urgency of understanding the relationship between NAFLD and IR. A significant positive correlation was found between the year of publication and the publication output using linear regression, further corroborating these findings.
The growth in publications on this subject was gradual and consistent with the increased interest in the topic. Some of those publications include Watt et al’s[84] analysis, of the effect of impaired liver lipid metabolism in NAFLD on the release of liver proteins, metabolites, and miRNAs, which influence metabolism in other tissues and lead to IR. Subsequently, elevated levels of IR, as described in a study by Angelico et al[85], more commonly coincide with severe stenosis. This relationship between NAFLD and IR was also observed by Kumashiro et al[86], who posited that the hepatic diacylglycerol content is the most accurate marker of IR.
These studies collectively emphasize that NAFLD is a threat to global health, highlighting the lack of a comprehensive understanding of NAFLD pathogenesis. Studies have suggested using preclinical models for more extensive research on this condition to mitigate this lack of understanding, and some have proposed combining herbal remedies with conventional lifestyle interventions and pharmacological management strategies for better NAFLD control[31,87-90].
A global effort can be observed in NAFLD and IR research involving more than 60 countries, with China and the United States in the number of publications, consistent with their longstanding leadership in biomedical research[91,92]. This notable publication lead in the United States can be attributed to substantial funding, advanced research facilities, and a solid scientific culture. Additionally, the United States’ focus on these areas may stem from increasing rates of obesity and metabolic syndrome[93]. Financial support from agencies such as the National Institute of Diabetes and Digestive and Kidney Diseases and the National Institutes of Health drove this research, as indicated by our findings and those of other studies[94-97].
China is also seeing more funding and an increased publication output in this field, partly due to substantial research investments and the increased number of metabolic syndrome cases caused by rapid urbanization[98-100]. The National Natural Science Foundation of China is the most influential funding source for this research, as shown in other studies[101-103] and corroborated by our findings. Josol et al’s[90] bibliometric analysis shows that this phenomenon is not exclusive to China but is also apparent in Southeast Asia. Research productivity is linked to socioeconomic factors, particularly economic status and research and development spending. In addition, NAFLD research in the region has focused on topics such as metabolic syndrome, diagnostics, treatment, and epigenetics.
In addition to China and the United States, countries such as Italy, Japan, South Korea, Iran, Spain, Turkey, Germany, and the United Kingdom are significant contributors to NAFLD research, driven by global interest in NAFLD and the goal of finding its treatment. This diversity of research locations can also be observed in the top institutional contributions, with Italian institutions such as the Università degli Studi di Torino and the Consiglio Nazionale delle Ricerche leading in publications. The research interest of these institutions in the subject is demonstrated by the establishment of the “NAFLD Study Group” at the Università degli Studi di Torino and the contributions of the Consiglio Nazionale delle Ricerche to various NAFLD-related projects[104,105].
The analysis of publication journals revealed that journals such as Hepatology, the Journal of Hepatology, and the Journal of Clinical Endocrinology and Metabolism are leading in publishing high-impact research. Citation analysis further highlights the impact of the research in this field. A high average citation count and h-index highlight the impact. Of NAFLD-IR research impact and its ongoing relevance[11,76,79]. Co-occurrence analysis revealed distinct research clusters that have evolved over time. The shift from discussing population health implications in early publications to a more recent focus on inflammation and high-fat diets and therapeutic approaches mirrors the shifting global focus on lifestyle factors and therapeutic advancements in understanding and managing NAFLD and IR[106-111].
This study had several limitations. First, it relied solely on Scopus, possibly overlooking studies not in this database. Second, the approach may have missed discussions of the relationship between NAFLD and IR in other types of articles. Third, inaccuracies could have arisen in identifying research origins based on affiliations. Fourth, the focus was on NAFLD and IR, excluding factors such as genetics. Fifth, only English-language publications were considered. Finally, the study is primarily descriptive and did not evaluate the quality or impact of individual studies in NAFLD research.
This was the first bibliometric analysis of NAFLD and IR research. The increase in publications, especially after 2011, indicates growing interest in this field. The significant topics of interest included lifestyle impact, treatment strategies, and metabolic disorders. Notable contributions came from several countries, with China and the United States being the most prominent. Given the urgency and worldwide impact of NAFLD, it is now necessary for global policymakers and health authorities to pay attention to this topic.
The author thanks An-Najah National University for all the administrative assistance during the implementation of the project.
| 1. | Teng ML, Ng CH, Huang DQ, Chan KE, Tan DJ, Lim WH, Yang JD, Tan E, Muthiah MD. Global incidence and prevalence of nonalcoholic fatty liver disease. Clin Mol Hepatol. 2023;29:S32-S42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 310] [Article Influence: 155.0] [Reference Citation Analysis (0)] |
| 2. | Le MH, Yeo YH, Zou B, Barnet S, Henry L, Cheung R, Nguyen MH. Forecasted 2040 global prevalence of nonalcoholic fatty liver disease using hierarchical bayesian approach. Clin Mol Hepatol. 2022;28:841-850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 153] [Article Influence: 51.0] [Reference Citation Analysis (0)] |
| 3. | Ma W, Wu W, Wen W, Xu F, Han D, Lyu J, Huang Y. Association of NAFLD with cardiovascular disease and all-cause mortality: a large-scale prospective cohort study based on UK Biobank. Ther Adv Chronic Dis. 2022;13:20406223221122478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Kudaravalli P, John S. Nonalcoholic Fatty Liver. 2023 Apr 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 5. | Stepanova M, De Avila L, Afendy M, Younossi I, Pham H, Cable R, Younossi ZM. Direct and Indirect Economic Burden of Chronic Liver Disease in the United States. Clin Gastroenterol Hepatol. 2017;15:759-766.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 118] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 6. | Ofosu A, Ramai D, Reddy M. Non-alcoholic fatty liver disease: controlling an emerging epidemic, challenges, and future directions. Ann Gastroenterol. 2018;31:288-295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Younossi ZM, Blissett D, Blissett R, Henry L, Stepanova M, Younossi Y, Racila A, Hunt S, Beckerman R. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64:1577-1586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 694] [Cited by in RCA: 911] [Article Influence: 101.2] [Reference Citation Analysis (0)] |
| 8. | Ezquerra EA, Vázquez JMC, Barrero AA. Obesity, Metabolic Syndrome, and Diabetes: Cardiovascular Implications and Therapy. Revista Española de Cardiología (English Ed). 2008;61:752-764. [DOI] [Full Text] |
| 9. | Shahwan M, Jairoun AA, Alaila RF, Alnuaimi GRH, Alalalmeh SO, Hegazi OE, Al-hemyari SS. Relation of erythrocyte sedimentation rate, glycemic parameters and lipid profile for the prediction of major adverse cardiovascular events: A single-center, cross-sectional study in Palestine. Obes Med. 2023;43:100513. [DOI] [Full Text] |
| 10. | Samuel VT, Liu ZX, Qu X, Elder BD, Bilz S, Befroy D, Romanelli AJ, Shulman GI. Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J Biol Chem. 2004;279:32345-32353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 945] [Cited by in RCA: 984] [Article Influence: 46.9] [Reference Citation Analysis (0)] |
| 11. | Utzschneider KM, Kahn SE. Review: The role of insulin resistance in nonalcoholic fatty liver disease. J Clin Endocrinol Metab. 2006;91:4753-4761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 555] [Cited by in RCA: 640] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 12. | Gierach M, Gierach J, Junik R. Insulin resistance and thyroid disorders. Endokrynol Pol. 2014;65:70-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Schmiedt RA, Tiuca RA, Tilinca RM, Custura LM, Detesan O, Bacso BI, Abalasei BL, Bell AC, Streza MA, Tilinca MC. Insulin resistance as risk factor for the development of type 2 diabetes mellitus: a systematic approach. Acta Marisiensis - Seria Medica. 2021;67:187-192. [DOI] [Full Text] |
| 14. | Pollak F, Araya V, Lanas A, Sapunar J, Arrese M, Aylwin CG, Bezanilla CG, Carrasco E, Carrasco F, Codner E, Díaz E, Durruty P, Galgani J, García H, Lahsen R, Liberman C, López G, Maíz A, Mujica V, Poniachik J, Sir T, Soto N, Valderas J, Villaseca P, Zavala C. Second Consensus of the Chilean Society of Endocrinology and Diabetes about insulin resistance. Rev Med Chil. 2015;143:627-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Pollak CF. Resistencia a la insulina: verdades y controversias. Revista Médica Clínica Las Condes. 2016;27:171-178. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Sharma VR, Matta ST, Haymond MW, Chung ST. Measuring Insulin Resistance in Humans. Horm Res Paediatr. 2020;93:577-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Fang P, Shi M, Yu M, Bo P. New insight into the regulation of insulin resistance. In: Insulin Resistance: New Developments. 2013: 41-66. |
| 18. | Le TKC, Dao XD, Nguyen DV, Luu DH, Bui TMH, Le TH, Nguyen HT, Le TN, Hosaka T, Nguyen TTT. Insulin signaling and its application. Front Endocrinol (Lausanne). 2023;14:1226655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 34] [Reference Citation Analysis (0)] |
| 19. | Halenova TI, Kuznetsova MY, Savchuk OM, Ostapchenko LI. Low molecular weight regulators of the intracellular insulin signal transduction as the method of correction of insulin resistance in the treatment of type 2 diabetes mellitus. Biochem Moscow Suppl Ser B. 2015;9:106-113. [DOI] [Full Text] |
| 20. | Brunner KT, Henneberg CJ, Wilechansky RM, Long MT. Nonalcoholic Fatty Liver Disease and Obesity Treatment. Curr Obes Rep. 2019;8:220-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 21. | Nair S, Diehl AM, Wiseman M, Farr GH Jr, Perrillo RP. Metformin in the treatment of non-alcoholic steatohepatitis: a pilot open label trial. Aliment Pharmacol Ther. 2004;20:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 249] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 22. | Marchesini G, Brizi M, Bianchi G, Tomassetti S, Zoli M, Melchionda N. Metformin in non-alcoholic steatohepatitis. Lancet. 2001;358:893-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 479] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 23. | Uygun A, Kadayifci A, Isik AT, Ozgurtas T, Deveci S, Tuzun A, Yesilova Z, Gulsen M, Dagalp K. Metformin in the treatment of patients with non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2004;19:537-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 276] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 24. | Tiikkainen M, Häkkinen AM, Korsheninnikova E, Nyman T, Mäkimattila S, Yki-Järvinen H. Effects of rosiglitazone and metformin on liver fat content, hepatic insulin resistance, insulin clearance, and gene expression in adipose tissue in patients with type 2 diabetes. Diabetes. 2004;53:2169-2176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 378] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 25. | Cnop M, Havel PJ, Utzschneider KM, Carr DB, Sinha MK, Boyko EJ, Retzlaff BM, Knopp RH, Brunzell JD, Kahn SE. Relationship of adiponectin to body fat distribution, insulin sensitivity and plasma lipoproteins: evidence for independent roles of age and sex. Diabetologia. 2003;46:459-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1014] [Cited by in RCA: 1060] [Article Influence: 48.2] [Reference Citation Analysis (0)] |
| 26. | Yamauchi T, Kamon J, Minokoshi Y, Ito Y, Waki H, Uchida S, Yamashita S, Noda M, Kita S, Ueki K, Eto K, Akanuma Y, Froguel P, Foufelle F, Ferre P, Carling D, Kimura S, Nagai R, Kahn BB, Kadowaki T. Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat Med. 2002;8:1288-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3051] [Cited by in RCA: 3047] [Article Influence: 132.5] [Reference Citation Analysis (0)] |
| 27. | Acosta RC, Molina EG, O'brien CB, Cobo MC, Amaro R, Neff GW, Schiff ER. The Use of piogliatazone in menalcoholic stealohepatitis. Gastroenterology. 2001;120:A546. [DOI] [Full Text] |
| 28. | Basaranoglu M, Acbay O, Sonsuz A. A controlled trial of gemfibrozil in the treatment of patients with nonalcoholic steatohepatitis. J Hepatol. 1999;31:384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 200] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 29. | Chang CY, Argo CK, Al-Osaimi AM, Caldwell SH. Therapy of NAFLD: antioxidants and cytoprotective agents. J Clin Gastroenterol. 2006;40 Suppl 1:S51-S60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 30. | Hatzitolios A, Savopoulos C, Lazaraki G, Sidiropoulos I, Haritanti P, Lefkopoulos A, Karagiannopoulou G, Tzioufa V, Dimitrios K. Efficacy of omega-3 fatty acids, atorvastatin and orlistat in non-alcoholic fatty liver disease with dyslipidemia. Indian J Gastroenterol. 2004;23:131-134. [PubMed] |
| 31. | Hegazi OE, Alalalmeh SO, Alnuaimi GRH, Shahwan M, Jairoun AA, Alorfi NM, Majrashi SA, Alkhanani MF, Alkhattabi A, Alourfi MM, Alsolami FA, Alsharif S, Alshahrani H. NAFLD and nutraceuticals: a review of completed phase III and IV clinical trials. Front Med (Lausanne). 2023;10:1227046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 32. | Zyoud SH. The state of current research on COVID-19 and antibiotic use: global implications for antimicrobial resistance. J Health Popul Nutr. 2023;42:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 33. | Zhang Y, Hu M, Wang J, Wang P, Shi P, Zhao W, Liu X, Peng Q, Meng B, Feng X, Zhang L. A Bibliometric Analysis of Personal Protective Equipment and COVID-19 Research. Front Public Health. 2022;10:855633. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 34. | Zyoud SH, Zyoud AH. Coronavirus disease-19 in environmental fields: a bibliometric and visualization mapping analysis. Environ Dev Sustain. 2021;23:8895-8923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 35. | Chen Z, Ding C, Gu Y, He Y, Chen B, Zheng S, Li Q. Association between gut microbiota and hepatocellular carcinoma from 2011 to 2022: Bibliometric analysis and global trends. Front Oncol. 2023;13:1120515. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 36. | Liao Y, Wang L, Liu F, Zhou Y, Lin X, Zhao Z, Xu S, Tang D, Jiao Y, Yang L, Yu W, Gao P. Emerging trends and hotspots in metabolic dysfunction-associated fatty liver disease (MAFLD) research from 2012 to 2021: A bibliometric analysis. Front Endocrinol (Lausanne). 2023;14:1078149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 37. | Shibo C, Sili W, Yanfang Q, Shuxiao G, Susu L, Xinlou C, Yongsheng Z. Emerging trends and hotspots in the links between the bile acids and NAFLD from 2002 to 2022: A bibliometric analysis. Endocrinol Diabetes Metab. 2024;7:e460. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 38. | Li Y, Zhou Y, Wang L, Lin X, Mao M, Yin S, Zhu L, Jiao Y, Yu W, Gao P, Yang L. Emerging trends and hotspots in the links between the gut microbiota and MAFLD from 2002 to 2021: A bibliometric analysis. Front Endocrinol (Lausanne). 2022;13:990953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 39. | Zhu X, Zhou Z, Pan X. Research reviews and prospects of gut microbiota in liver cirrhosis: a bibliometric analysis (2001-2023). Front Microbiol. 2024;15:1342356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 40. | Wang Q, Chen CX, Zuo S, Cao K, Li HY. Global research trends on the links between intestinal microbiota and liver diseases: a bibliometric analysis. Am J Transl Res. 2023;15:5364-5372. [PubMed] |
| 41. | Dai JJ, Zhang YF, Zhang ZH. Global trends and hotspots of treatment for nonalcoholic fatty liver disease: A bibliometric and visualization analysis (2010-2023). World J Gastroenterol. 2023;29:5339-5360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 17] [Article Influence: 8.5] [Reference Citation Analysis (1)] |
| 42. | Pezzino S, Sofia M, Mazzone C, Castorina S, Puleo S, Barchitta M, Agodi A, Gallo L, La Greca G, Latteri S. Gut Microbiome in the Progression of NAFLD, NASH and Cirrhosis, and Its Connection with Biotics: A Bibliometric Study Using Dimensions Scientific Research Database. Biology (Basel). 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 43. | Zyoud SH, Shakhshir M, Abushanab AS, Koni A, Shahwan M, Jairoun AA, Al-jabi SW. Global research trends on the links between insulin resistance and obesity: a visualization analysis. Transl Med Commun. 2022;7:18. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 44. | Zhou X, Kang C, Hu Y, Wang X. Study on insulin resistance and ischemic cerebrovascular disease: A bibliometric analysis via CiteSpace. Front Public Health. 2023;11:1021378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 45. | Zyoud SH, Shakhshir M, Koni A, Abushanab AS, Shahwan M, Jairoun AA, Al Subu R, Abu Taha A, Al-Jabi SW. Mapping the global research landscape on insulin resistance: Visualization and bibliometric analysis. World J Diabetes. 2022;13:786-798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 46. | Yang S, Yu D, Liu J, Qiao Y, Gu S, Yang R, Chai X, Wang W. Global publication trends and research hotspots of the gut-liver axis in NAFLD: A bibliometric analysis. Front Endocrinol (Lausanne). 2023;14:1121540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 47. | Li Z, Cao S, Zhao S, Kang N. A bibliometric analysis and visualization of nonalcoholic fatty liver disease from 2012 to 2021. Clin Exp Med. 2023;23:1961-1971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 48. | Gu S, Qiao Y, Liu S, Yang S, Cong S, Wang S, Yu D, Wang W, Chai X. Frontiers and hotspots of adipose tissue and NAFLD: a bibliometric analysis from 2002 to 2022. Front Physiol. 2023;14:1278952. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 49. | Zhang TS, Qin HL, Wang T, Li HT, Li H, Xia SH, Xiang XH. Bibliometric analysis of top 100 cited articles in nonalcoholic fatty liver disease research. World J Hepatol. 2016;8:1478-1488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 50. | AlRyalat SAS, Malkawi LW, Momani SM. Comparing Bibliometric Analysis Using PubMed, Scopus, and Web of Science Databases. J Vis Exp. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 132] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 51. | Anker MS, Hadzibegovic S, Lena A, Haverkamp W. The difference in referencing in Web of Science, Scopus, and Google Scholar. ESC Heart Fail. 2019;6:1291-1312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 52. | Bakkalbasi N, Bauer K, Glover J, Wang L. Three options for citation tracking: Google Scholar, Scopus and Web of Science. Biomed Digit Libr. 2006;3:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 354] [Cited by in RCA: 341] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 53. | Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. FASEB J. 2008;22:338-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1736] [Cited by in RCA: 1637] [Article Influence: 90.9] [Reference Citation Analysis (0)] |
| 54. | Kulkarni AV, Aziz B, Shams I, Busse JW. Comparisons of citations in Web of Science, Scopus, and Google Scholar for articles published in general medical journals. JAMA. 2009;302:1092-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 459] [Cited by in RCA: 459] [Article Influence: 28.7] [Reference Citation Analysis (0)] |
| 55. | Sember M, Utrobicić A, Petrak J. Croatian Medical Journal citation score in Web of Science, Scopus, and Google Scholar. Croat Med J. 2010;51:99-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 56. | Mongeon P, Paul-hus A. The journal coverage of Web of Science and Scopus: a comparative analysis. Scientometrics. 2016;106:213-228. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1180] [Cited by in RCA: 822] [Article Influence: 82.2] [Reference Citation Analysis (0)] |
| 57. | Su KZ, Li YR, Zhang D, Yuan JH, Zhang CS, Liu Y, Song LM, Lin Q, Li MW, Dong J. Relation of Circulating Resistin to Insulin Resistance in Type 2 Diabetes and Obesity: A Systematic Review and Meta-Analysis. Front Physiol. 2019;10:1399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 82] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 58. | Sampath Kumar A, Maiya AG, Shastry BA, Vaishali K, Ravishankar N, Hazari A, Gundmi S, Jadhav R. Exercise and insulin resistance in type 2 diabetes mellitus: A systematic review and meta-analysis. Ann Phys Rehabil Med. 2019;62:98-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 246] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 59. | Shoshtari-Yeganeh B, Zarean M, Mansourian M, Riahi R, Poursafa P, Teiri H, Rafiei N, Dehdashti B, Kelishadi R. Systematic review and meta-analysis on the association between phthalates exposure and insulin resistance. Environ Sci Pollut Res Int. 2019;26:9435-9442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 60. | Sweileh WM. Analysis and mapping of global research publications on shift work (2012-2021). J Occup Med Toxicol. 2022;17:22. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 61. | Sweileh WM. Analysis and Mapping of Scientific Literature on Detention and Deportation of International Migrants (1990-2022). J Immigr Minor Health. 2023;25:1065-1076. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 62. | Zyoud SH. Research landscape on COVID-19 and liver dysfunction: A bibliometric analysis. World J Gastroenterol. 2023;29:4356-4367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 63. | Zyoud SH, Shakhshir M, Abushanab AS, Koni A, Shahwan M, Jairoun AA, Al-Jabi SW. Bibliometric mapping of the landscape and structure of nutrition and depression research: visualization analysis. J Health Popul Nutr. 2023;42:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 64. | Sweileh WM. Substandard and falsified medical products: bibliometric analysis and mapping of scientific research. Global Health. 2021;17:114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 65. | Sweileh WM. Global research activity on mathematical modeling of transmission and control of 23 selected infectious disease outbreak. Global Health. 2022;18:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 42] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 66. | Al-Jabi SW. Current global research landscape on COVID-19 and depressive disorders: Bibliometric and visualization analysis. World J Psychiatry. 2021;11:253-264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 24] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 67. | Al-Jabi SW. Global research trends and mapping knowledge structure of depression in dialysis patients. World J Psychiatry. 2023;13:593-606. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Reference Citation Analysis (0)] |
| 68. | Barqawi A, Abushamma FA, Akkawi M, Al-Jabi SW, Shahwan MJ, Jairoun AA, Zyoud SH. Global trends in research related to sleeve gastrectomy: A bibliometric and visualized study. World J Gastrointest Surg. 2021;13:1509-1522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 69. | Zyoud SH, Shakhshir M, Abushanab AS, Koni A, Shahwan M, Jairoun AA, Abu Taha A, Al-Jabi SW. Gut microbiota and autism spectrum disorders: where do we stand? Gut Pathog. 2023;15:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 70. | Wang JL, Ma YJ, Ma L, Ma N, Guo DM, Ma LS. Baishideng's Reference Citation Analysis database announces the first Article Influence Index of multidisciplinary scholars. World J Clin Cases. 2022;10:10391-10398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (2)] |
| 71. | Wang JL, Ma YJ, Ma L, Ma N, Guo DM, Ma LS. Baishideng's Reference Citation Analysis database announces the first Journal Article Influence Index of 101 core journals and a list of high-quality academic journals in gastroenterology and hepatology. World J Gastroenterol. 2022;28:5383-5394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (3)] |
| 72. | Wang JL, Ma YJ, Ma L, Ma N, Guo DM, Ma LS. Baishideng's Reference Citation Analysis database announces the first Journal Article Influence Index of 104 core journals and a list of high-quality academic journals in orthopedics. World J Orthop. 2022;13:891-902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 73. | van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4505] [Cited by in RCA: 5067] [Article Influence: 316.7] [Reference Citation Analysis (0)] |
| 74. | van Eck NJ, Waltman L. Citation-based clustering of publications using CitNetExplorer and VOSviewer. Scientometrics. 2017;111:1053-1070. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 507] [Cited by in RCA: 557] [Article Influence: 69.6] [Reference Citation Analysis (0)] |
| 75. | Waaijer CJ, van Bochove CA, van Eck NJ. On the map: Nature and Science editorials. Scientometrics. 2011;86:99-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 76. | Sanyal AJ, Campbell-Sargent C, Mirshahi F, Rizzo WB, Contos MJ, Sterling RK, Luketic VA, Shiffman ML, Clore JN. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology. 2001;120:1183-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1458] [Cited by in RCA: 1507] [Article Influence: 62.8] [Reference Citation Analysis (0)] |
| 77. | Marchesini G, Brizi M, Morselli-Labate AM, Bianchi G, Bugianesi E, McCullough AJ, Forlani G, Melchionda N. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med. 1999;107:450-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1074] [Cited by in RCA: 1097] [Article Influence: 42.2] [Reference Citation Analysis (1)] |
| 78. | Jung UJ, Choi MS. Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. Int J Mol Sci. 2014;15:6184-6223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1040] [Cited by in RCA: 1304] [Article Influence: 118.5] [Reference Citation Analysis (0)] |
| 79. | Pagano G, Pacini G, Musso G, Gambino R, Mecca F, Depetris N, Cassader M, David E, Cavallo-Perin P, Rizzetto M. Nonalcoholic steatohepatitis, insulin resistance, and metabolic syndrome: further evidence for an etiologic association. Hepatology. 2002;35:367-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 546] [Cited by in RCA: 542] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 80. | Musso G, Gambino R, De Michieli F, Cassader M, Rizzetto M, Durazzo M, Fagà E, Silli B, Pagano G. Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology. 2003;37:909-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 526] [Cited by in RCA: 534] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 81. | Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients. 2013;5:1544-1560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 476] [Cited by in RCA: 605] [Article Influence: 50.4] [Reference Citation Analysis (0)] |
| 82. | Bugianesi E, Gastaldelli A, Vanni E, Gambino R, Cassader M, Baldi S, Ponti V, Pagano G, Ferrannini E, Rizzetto M. Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: sites and mechanisms. Diabetologia. 2005;48:634-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 503] [Cited by in RCA: 538] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 83. | Birkenfeld AL, Shulman GI. Nonalcoholic fatty liver disease, hepatic insulin resistance, and type 2 diabetes. Hepatology. 2014;59:713-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 527] [Cited by in RCA: 562] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 84. | Watt MJ, Miotto PM, De Nardo W, Montgomery MK. The Liver as an Endocrine Organ-Linking NAFLD and Insulin Resistance. Endocr Rev. 2019;40:1367-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 407] [Article Influence: 67.8] [Reference Citation Analysis (2)] |
| 85. | Angelico F, Del Ben M, Conti R, Francioso S, Feole K, Fiorello S, Cavallo MG, Zalunardo B, Lirussi F, Alessandri C, Violi F. Insulin resistance, the metabolic syndrome, and nonalcoholic fatty liver disease. J Clin Endocrinol Metab. 2005;90:1578-1582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 194] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 86. | Kumashiro N, Erion DM, Zhang D, Kahn M, Beddow SA, Chu X, Still CD, Gerhard GS, Han X, Dziura J, Petersen KF, Samuel VT, Shulman GI. Cellular mechanism of insulin resistance in nonalcoholic fatty liver disease. Proc Natl Acad Sci U S A. 2011;108:16381-16385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 400] [Cited by in RCA: 436] [Article Influence: 31.1] [Reference Citation Analysis (0)] |
| 87. | Xu Y, Guo W, Zhang C, Chen F, Tan HY, Li S, Wang N, Feng Y. Herbal Medicine in the Treatment of Non-Alcoholic Fatty Liver Diseases-Efficacy, Action Mechanism, and Clinical Application. Front Pharmacol. 2020;11:601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 85] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 88. | Yao H, Qiao YJ, Zhao YL, Tao XF, Xu LN, Yin LH, Qi Y, Peng JY. Herbal medicines and nonalcoholic fatty liver disease. World J Gastroenterol. 2016;22:6890-6905. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 113] [Cited by in RCA: 101] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 89. | Flessa CM, Nasiri-Ansari N, Kyrou I, Leca BM, Lianou M, Chatzigeorgiou A, Kaltsas G, Kassi E, Randeva HS. Genetic and Diet-Induced Animal Models for Non-Alcoholic Fatty Liver Disease (NAFLD) Research. Int J Mol Sci. 2022;23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 54] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 90. | Josol VJD, Salvador PBU, Cruz LLA, Ornos EDB, Tantengco OAG. Trends of nonalcoholic fatty liver research in Southeast Asia from 2004 to 2022: A bibliometric analysis. Obesity Med. 2024;45:100527. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 91. | Wilson SH, Merkle S, Brown D, Moskowitz J, Hurley D, Brown D, Bailey BJ, McClain M, Misenhimer M, Buckalew J, Burks T. Biomedical research leaders: report on needs, opportunities, difficulties, education and training, and evaluation. Environ Health Perspect. 2000;108 Suppl 6:979-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 92. | Dzau VJ, Fineberg HV. Restore the US lead in biomedical research. JAMA. 2015;313:143-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 93. | Liang X, Or B, Tsoi MF, Cheung CL, Cheung BMY. Prevalence of metabolic syndrome in the United States National Health and Nutrition Examination Survey 2011-18. Postgrad Med J. 2023;99:985-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 84] [Article Influence: 42.0] [Reference Citation Analysis (0)] |
| 94. | Chen J, Wildman RP, Hamm LL, Muntner P, Reynolds K, Whelton PK, He J; Third National Health and Nutrition Examination Survey. Association between inflammation and insulin resistance in U.S. nondiabetic adults: results from the Third National Health and Nutrition Examination Survey. Diabetes Care. 2004;27:2960-2965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 102] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 95. | National Institute of Diabetes and Digestive and Kidney Diseases. Insulin Resistance & Prediabetes. [cited 29 April 2024]. Available from: https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance. |
| 96. | National Institute of Diabetes and Digestive and Kidney Diseases. Clinical Trials for NAFLD & NASH. [cited 29 April 2024]. Available from: https://www.niddk.nih.gov/health-information/Liver-disease/nafld-nash/clinical-trials. |
| 97. | Clerx E, Kupfer SS, Leffler DA; North American Society for the Study of Celiac Disease. Disparities Among Gastrointestinal Disorders in Research Funding From the National Institutes of Health. Gastroenterology. 2017;153:877-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 98. | Marginson S. 'All things are in flux': China in global science. High Educ (Dordr). 2022;83:881-910. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 99. | Bai A, Wu C, Yang K. Evolution and Features of China's Central Government Funding System for Basic Research. Front Res Metr Anal. 2021;6:751497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 100. | Shen J, Goyal A, Sperling L. The emerging epidemic of obesity, diabetes, and the metabolic syndrome in China. Cardiol Res Pract. 2012;2012:178675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 101. | Guo X, Yin X, Liu Z, Wang J. Non-Alcoholic Fatty Liver Disease (NAFLD) Pathogenesis and Natural Products for Prevention and Treatment. Int J Mol Sci. 2022;23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 174] [Reference Citation Analysis (1)] |
| 102. | Yang N, He L, Li Y, Xu L, Ping F, Li W, Zhang H. Reduced Insulin Resistance Partly Mediated the Association of High Dietary Magnesium Intake with Less Metabolic Syndrome in a Large Chinese Population. Diabetes Metab Syndr Obes. 2020;13:2541-2550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 103. | Zhao M, Hu Y, Shi C, Wang K, Li J, Song J, Huo C, Xi Y, Bu S, Huang Q. NFI, a clinical scoring tool for predicting non-alcoholic fatty liver in the Chinese population. Public Health. 2022;202:12-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 104. | European Commission. Bioenergetic Remodeling in the Pathophysiology and Treatment of Non-Alcoholic Fatty Liver Disease. [cited 29 April 2024]. Available from: https://cordis.europa.eu/project/id/722619. |
| 105. | Unito.it. Non-alcoholic fatty liver disease (NAFLD) Study Group. [cited 29 April 2024]. Available from: https://www.dsm.unito.it/do/home.pl/View?doc=gruppi_ricerca/Gastroenterologia/NAFLD.html. |
| 106. | Rippe JM. Lifestyle Medicine: The Health Promoting Power of Daily Habits and Practices. Am J Lifestyle Med. 2018;12:499-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 119] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 107. | Huang X, Chen H, Wen S, Dong M, Zhou L, Yuan X. Therapeutic Approaches for Nonalcoholic Fatty Liver Disease: Established Targets and Drugs. Diabetes Metab Syndr Obes. 2023;16:1809-1819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 108. | Ferguson D, Finck BN. Emerging therapeutic approaches for the treatment of NAFLD and type 2 diabetes mellitus. Nat Rev Endocrinol. 2021;17:484-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 321] [Article Influence: 80.3] [Reference Citation Analysis (0)] |
| 109. | Lian CY, Zhai ZZ, Li ZF, Wang L. High fat diet-triggered non-alcoholic fatty liver disease: A review of proposed mechanisms. Chem Biol Interact. 2020;330:109199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 175] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 110. | Huang WC, Xu JW, Li S, Ng XE, Tung YT. Effects of exercise on high-fat diet-induced non-alcoholic fatty liver disease and lipid metabolism in ApoE knockout mice. Nutr Metab (Lond). 2022;19:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 111. | Bodai BI, Nakata TE, Wong WT, Clark DR, Lawenda S, Tsou C, Liu R, Shiue L, Cooper N, Rehbein M, Ha BP, Mckeirnan A, Misquitta R, Vij P, Klonecke A, Mejia CS, Dionysian E, Hashmi S, Greger M, Stoll S, Campbell TM. Lifestyle Medicine: A Brief Review of Its Dramatic Impact on Health and Survival. Perm J. 2018;22:17-025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 104] [Article Influence: 14.9] [Reference Citation Analysis (0)] |