Published online May 27, 2024. doi: 10.4254/wjh.v16.i5.860
Revised: February 29, 2024
Accepted: April 9, 2024
Published online: May 27, 2024
Processing time: 113 Days and 14.9 Hours
The development of type 2 diabetes mellitus is a major contributing factor to the worldwide health burden of metabolic dysfunction-associated steatotic liver disease (MASLD). Insulin resistance, subclinical inflammation, dyslipidemia, obesity, and hypertension are all factors in this reciprocal interaction that contribute to the development of MASLD, which includes hepatocellular carci
Core Tip: A recent large-scale study inculpates gestational diabetes mellitus (GDM) as a novel risk factor for metabolic dysfunction-associated steatotic liver disease (MASLD). The impact of GDM on disease progression is exerted throughout life. Early screening and management strategies are crucial in mitigating MASLD progression and preventing adverse cardiovascular events in affected individuals.
- Citation: Milionis C, Ilias I, Koukkou E. Gestational diabetes mellitus may predispose to metabolic dysfunction-associated steatotic liver disease. World J Hepatol 2024; 16(5): 860-862
- URL: https://www.wjgnet.com/1948-5182/full/v16/i5/860.htm
- DOI: https://dx.doi.org/10.4254/wjh.v16.i5.860
In a recent comprehensive review published in this journal, the authors provided an extensive analysis of metabolic dysfunction-associated steatotic liver disease (MASLD), recognized as the most prevalent liver disorder globally[1]. Type 2 diabetes mellitus (DM2) emerges as a pivotal factor in the progression of non-alcoholic steatohepatitis (NASH)/metabolic dysfunction-associated steatohepatitis (MASH) to advanced liver fibrosis/cirrhosis and hepatocellular carcinoma, as well as a contributor to liver-related mortality. The intricate relationship between MASLD and DM2 involves bidirectional influences, with insulin resistance and subclinical inflammation playing pivotal roles in MASLD pathogenesis. Dyslipidemia in MASLD manifests through impaired lipid uptake, enhanced de novo lipogenesis, and altered lipid export, culminating in abnormal plasma lipoprotein profiles associated with atherosclerosis. Additionally, obesity significantly exacerbates MASLD by inciting intrahepatic inflammation and fibrosis, thereby increasing the risk of cirrhosis and neoplasia. The prevalence of hypertension in MASLD patients underscores its association with systemic inflammation, insulin resistance, lipid deposition, elevated homocysteine levels, and intestinal dysbiosis. Notably, cardiovascular disease stands as the leading cause of mortality in MASLD patients, with risk factors intricately linked to metabolic syndrome (MetS). Early screening for these comorbidities is imperative for disease management and preventing cardiovascular events in MASLD patients.
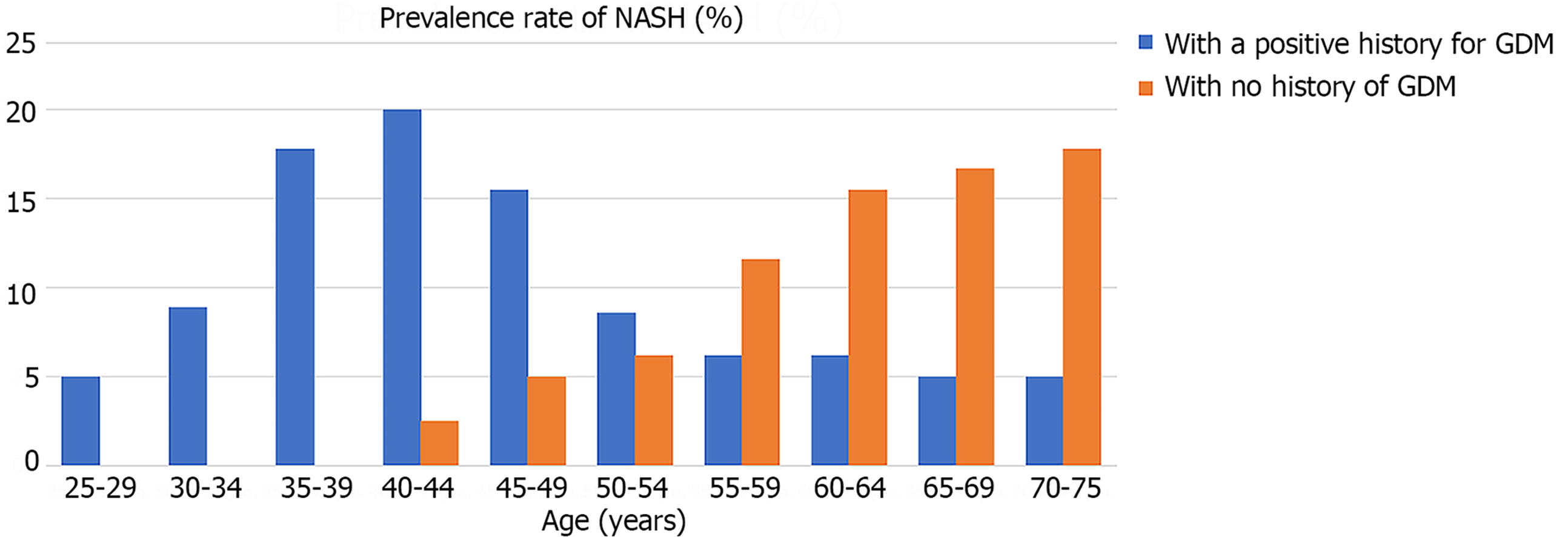
Expanding upon the established contributors to MASLD/NASH, we propose the inclusion of gestational diabetes mellitus (GDM), affecting at least 5% of pregnancies worldwide (and potentially up to one-third of pregnancies)[2,3]. A recent study investigated the association between a history of GDM and the lifelong development of NASH, while controlling for the influence of DM2[4], using the validated Explorys database (formerly IBM Watson, now Merative, Ann Arbor, MI, United States), which encompasses data from over 360 hospitals. The researchers categorized adult females into those with NASH [coded by Systematized Nomenclature of Medicine Clinical Terms (SNOMED-CT) as 442685003] and those without. Regression analysis was performed to adjust for potential confounding factors. Among 70632640 individuals aged 18 years and above screened in the database, 36550 women were diagnosed with NASH and were compared to 38556480 women without NASH. Significantly more women with NASH were Caucasian [odds ratio (OR): 2.13] and/or obese (OR: 4.83). Furthermore, women with NASH were more likely to have had a medical history of GDM (OR: 1.23) or had received a diagnosis of DM2 (OR: 4.52), hyperlipidemia (OR: 2.59), MetS (OR: 3.07), polycystic ovary disease (OR: 1.72) or hypothyroidism (OR: 1.59)[4]. Notably, NASH prevalence was higher among middle-aged women (35-44 years old) with a history of GDM, while in women without GDM, NASH was more prevalent among those aged 65 and above (Figure 1).
These findings above underscore the increased risk of NASH development throughout life in women with a history of GDM, independently of other potential confounders. However, the study's methodology regarding subjects diagnosed with non-alcoholic fatty liver disease (SNOMED code: 197315008) remains unclear. Additionally, the study's limitations include possible data entry bias and the potential for outcome/diagnosis overestimation due to the extensive database size. While the precise pathogenesis remains elusive, the authors postulated that during pregnancy, transient dysfunction of the pancreatic beta cells might trigger the extensive release of mediators of inflammation, subsequently impacting adjacent and remote organs, including the liver[4].
Thus, the inclusion of GDM as a contributing factor unveils a novel dimension and enriches the comprehensive overview of MASLD recently published[1].
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Greece
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Soldera J, Brazil S-Editor: Liu JH L-Editor: A P-Editor: Cai YX
| 1. | Vargas M, Cardoso Toniasso SC, Riedel PG, Baldin CP, Dos Reis FL, Pereira RM, Brum MCB, Joveleviths D, Alvares-da-Silva MR. Metabolic disease and the liver: A review. World J Hepatol. 2024;16:33-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (3)] |
| 2. | American Diabetes Association Professional Practice Committee. 15. Management of Diabetes in Pregnancy: Standards of Care in Diabetes-2024. Diabetes Care. 2024;47:S282-S294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 96] [Article Influence: 96.0] [Reference Citation Analysis (0)] |
| 3. | Lende M, Rijhsinghani A. Gestational Diabetes: Overview with Emphasis on Medical Management. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 4. | Boustany A, Onwuzo S, Zeid HKA, Almomani A, Kumar P, Hitawala A, Asaad I. Non-alcoholic steatohepatitis is independently associated with a history of gestational diabetes mellitus. J Gastroenterol Hepatol. 2023;38:984-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |