Published online Jan 27, 2024. doi: 10.4254/wjh.v16.i1.103
Peer-review started: August 25, 2023
First decision: September 14, 2023
Revised: October 24, 2023
Accepted: December 12, 2023
Article in press: December 12, 2023
Published online: January 27, 2024
Processing time: 151 Days and 8.2 Hours
Pylephlebitis is an extremely rare form of septic thrombophlebitis involving the portal vein, carrying high rates of morbidity and mortality.
We present a case of a 42-year-old male with no past medical history who present
Our case highlights the importance of considering pylephlebitis in the broad differential for abdominal pain, especially if there are co-existing risk factors for hypercoagulability. We also demonstrate that fulminant hepatic failure in these patients can potentially be reversible with the immediate initiation of antibiotics and anticoagulation.
Core Tip: Septic thrombosis of the portal vein, also known as pylephlebitis, is difficult to diagnose as it often presents with non-specific symptoms including fever and abdominal pain. As a result, a high clinical suspicion for pylephlebitis is warranted since this condition is life-threatening without treatment. We aim to highlight acute liver failure as a possible life-threatening sequela of pylephlebitis. Furthermore, we demonstrate that prompt initiation of antibiotics and possible anticoagulation can result in complete resolution of fulminant hepatic failure.
- Citation: Hapshy V, Imburgio S, Sanekommu H, Nightingale B, Taj S, Hossain MA, Patel S. Pylephlebitis-induced acute liver failure: A case report and review of literature. World J Hepatol 2024; 16(1): 103-108
- URL: https://www.wjgnet.com/1948-5182/full/v16/i1/103.htm
- DOI: https://dx.doi.org/10.4254/wjh.v16.i1.103
Acute liver failure (ALF) is a life-threatening form of severe hepatocyte necrosis that results in impaired synthetic function and encephalopathy in individuals without preexisting liver disease[1]. Abrupt damage to the liver parenchyma can result in a triad of clinical findings including rapid elevation of aminotransferase enzymes levels, altered mental status, and impaired coagulation[2]. ALF typically manifests within a few days of an acute insult, has a disease course of less than 26 wk, and can be distinguished from acute on chronic decompensated liver failure by the absence of previous liver disease[3,4]. Approximately 3000 annual cases of ALF occur in the United States each year with the most common cause being acetaminophen toxicity[5]. Other reported etiologies include viral hepatitis, drug-induced liver injury, ischemia, autoimmune hepatitis, and Budd-Chiari syndrome[6]. To date, few case reports have demonstrated portal vein thrombosis as a cause of new-onset hepatic dysfunction[7-9]. Even more rare is septic thrombophlebitis of the portal vein, known as pylephlebitis, resulting in ALF. To our knowledge, we present the first reported case of pylephlebitis resulting in fulminant hepatic failure in a young patient which was successfully reversed with prompt initiation of antibiotics and anticoagulation.
A 42-year-old male with no past medical history presented with a three-day history of right upper quadrant abdominal pain and altered mental status.
Three-day history of right upper quadrant abdominal pain and altered mental status.
Non-contributory.
Non-contributory.
In the emergency department, he was visibly jaundiced. Vitals were significant for fever of 38.5° C or 101.4° F, tachycardia at 135 beats-per-minute, and hypotension with blood pressure of 88/48 mmHg.
Initial laboratory tests were normal except for leukocytosis of 22.2 ×103/μL (Ref: 4.5-11.0 ×103/μL) and elevated lactic acid at 4.1 mmol/L (Ref: 0.5-2.0 mmol/L).
Due to concern of sepsis, broad-spectrum antibiotics were started, along with fluid resuscitation. However, a computed tomography (CT) scan of the abdomen and pelvis with intravenous (IV) contrast did not reveal any signs of infection or evidence of cirrhosis. Additional investigations for a source of infection including chest X-ray, urinalysis, right upper quadrant ultrasound, magnetic resonance cholangiopancreatography, and transthoracic echocardiogram failed to reveal an infective source.
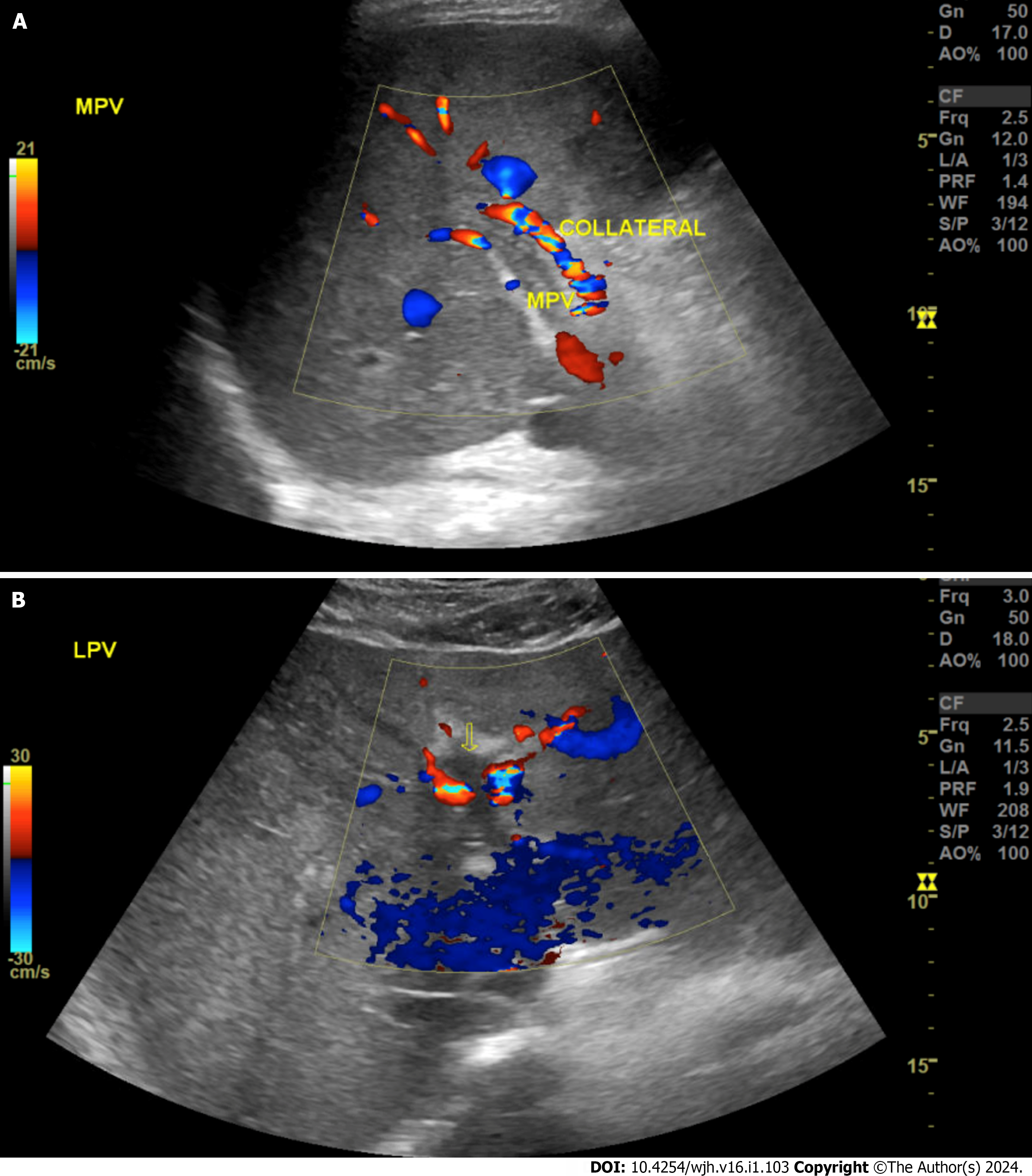
Two days after admission, blood cultures grew Fusobacterium necrophorum and Bacteroides ovatus. The blood culture susceptibility report demonstrated sensitivity to ampicillin/sulbactam with the antibiotic regimen narrowed appropriately. Ultimately, a vascular abdominal ultrasound was ordered, demonstrating complete thrombosis of both the main and left portal veins (Figure 1, respectively). The diagnosis of spontaneous pylephlebitis was made.
A therapeutic dose heparin drip was started. Repeat blood cultures two days later showed resolution of the bacteremia. An investigation for the patient’s risk factors for hypercoagulability revealed an extensive smoking history of 20-pack years and obesity with a body mass index of 31.2 kg/m2, in addition to the sepsis-induced inflammatory state. A peripherally inserted central catheter was placed and the patient was discharged on a six-week total course of IV ampicillin/sulbactam 3 g every six hours and also transitioned to a six-month total course of oral rivaroxaban 20 mg daily.
The patient was scheduled for outpatient follow-up in the clinic one week later with repeat blood work at that time demonstrating complete resolution of the liver impairment and discharged from the hospital after an nine day hospital course.
Thrombophlebitis is characterized by a venous inflammation accompanied by venous thrombosis[10]. When an endovascular thrombus occurs in the setting of concurrent infection, it is referred to as septic thrombophlebitis[11]. The specific term pylephlebitis is used to describe an extremely rare form of septic thrombophlebitis of the portal vein with an estimated annual incidence of 0.37-2.7 cases per 100000[12]. Pylephlebitis typically occurs in response to an abdominal inflammatory process that results in uncontrolled infection in the regions adjacent or draining into the portal venous system, most often caused by Gram-negative anaerobic bacteria[13]. This is similar to Lemierre’s syndrome, caused by the same organism as seen in our case, Fusobacterium necrophorum, in which the bacterium extends to the parapharyngeal space causing septic thrombophlebitis of the internal jugular vein[14]. In this same vein, pylephlebitis shares similar pathophysiologic concepts as Lemierre’s syndrome and can be attributed to vascular changes from gram-negative anaerobic bacteria infiltration[14].
Multiple case reports have described various intra-abdominal inflammatory conditions such as diverticulitis, appendicitis, and pancreatitis developing into septic portal vein thrombosis due to direct invasion from an adjacent nonvascular infection[15-18]. Diagnosis is often challenging as common presentations include non-specific symptoms such as generalized abdominal pain and fever[19]. A CT scan with oral and IV contrast is the imaging modality of choice as it can detect both the portal vein thrombosis and intra-abdominal infection.
In the absence of a source of inflammation or infection like our case, another proposed mechanism involves an obstructive clot that promotes bacterial colonization in a manner similar to that of ascending cholangitis[20]. In cases of pylephlebitis where no intra-abdominal infection can be identified, an investigation as to the pathogenesis of the underlying acute thrombosis of the portal vein is warranted. A majority of cases of portal vein thrombosis occur in patients with cirrhosis or malignancy due to the inherent hypercoagulable nature of these conditions[21]. However, a small subset of patients may develop thrombosis in this unusual vascular territory as a result of other prothrombogenic conditions including inherited and acquired thrombophilias[22]. After these conditions are ruled out, it is reasonable to attribute the portal vein clot to a multifactorial etiology if various pro-thromboembolic risk factors are present such as ongoing inflammation, extensive smoking history, and obesity as in our patient[23].
Complications of pylephlebitis are scarcely documented in the literature but small bowel infarction, hepatic abscesses, and septic pulmonary emboli have been reported[24]. To our knowledge, there have been no documented cases of new-onset ALF as a sequela of pylephlebitis to date. As a result, the mechanism of ALF in pylephlebitis is poorly understood. The potential pathogenesis may first involve the natural progression of pylephlebitis which typically first involves thrombophlebitis of the smaller mesenteric veins with subsequent migration of the thrombosis to the larger portal veins[25]. It is possible that this thromboembolic event may rapidly occur in the same manner as pulmonary embolism, preventing adequate hemodynamic compensatory responses. It is also possible that liver failure may originate from an alternative mechanism of diffuse microemboli in the smaller hepatic vessels similar to those postulated and seen in patients with coronavirus disease 2019[26]. With approximately 75% of hepatic blood flow coming from the portal venous system, acute suppurative thrombosis can cause significant damage to hepatocytes and allow progression to ALF when there is immediate complete occlusion of one or more portal veins[27]. Unlike cases of portal vein thrombosis in cirrhotic patients where the obstructive clot forms slowly in the portal venous system, the rapid nature of pylephlebitis may not allow for normal hepatic artery vasodilation and the development of venous collaterals which typically takes 3-5 wk to fully develop[28].
Recognizing ALF as a complication of septic thrombophlebitis is of clinical importance as this condition carries significant morbidity and a mortality rate of 30-50%[29]. Antibiotics are the primary form of therapy with parenteral antibiotics recommended, followed by a transition to an oral regimen for a total duration of 4-6 wk[30]. While Rivaroxaban was utilized in our case with success, the role of anticoagulation is an area of current controversy[13,31]. Emerging research, however, points to improved patient outcomes with the use of anticoagulation. To highlight this point, one retrospective review by Naymagon et al[32] reviewed 67 patients with pylephlebitis and found that the use of anticoagulation significantly improved the rate of portal vein thrombosis resolution. Additional studies with larger patient populations are needed to further confirm these findings, along with a special focus on which specific type of anticoagulation has the greatest efficacy. Despite the life-threatening nature of septic portal vein thrombophlebitis, it is often overlooked in the differential diagnosis of new-onset abdominal pain and fever. Awareness of pylephlebitis is important as swift recognition and initiation of broad-spectrum antibiotics in conjunction with possible anticoagulation is paramount to reducing mortality[33]. Ultimately, our case aims to highlight acute liver failure as an extremely rare presentation of septic portal vein thrombosis and demonstrates that this disease process is reversible with prompt intervention.
Septic thrombosis of the portal vein, also known as pylephlebitis, is difficult to diagnose as it often presents with non-specific symptoms including fever and abdominal pain. A high degree of clinical suspicion for pylephlebitis is warranted since this condition carries high morbidity and mortality without treatment. It is important to recognize acute liver failure as a possible life-threatening sequela of pylephlebitis. Antibiotics should be administered immediately, along with consideration for anticoagulation, as it can potentially lead to complete resolution of fulminant hepatic failure in these patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Harmanci O, Turkey; Valerio L, Germany S-Editor: Liu JH L-Editor: A P-Editor: Cai YX
| 1. | Bernal W, Wendon J. Acute liver failure. N Engl J Med. 2013;369:2525-2534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 736] [Cited by in RCA: 845] [Article Influence: 70.4] [Reference Citation Analysis (2)] |
| 2. | McDowell Torres D, Stevens RD, Gurakar A. Acute liver failure: a management challenge for the practicing gastroenterologist. Gastroenterol Hepatol (N Y). 2010;6:444-450. [PubMed] |
| 3. | Montrief T, Koyfman A, Long B. Acute liver failure: A review for emergency physicians. Am J Emerg Med. 2019;37:329-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Bajaj JS, O'Leary JG, Lai JC, Wong F, Long MD, Wong RJ, Kamath PS. Acute-on-Chronic Liver Failure Clinical Guidelines. Am J Gastroenterol. 2022;117:225-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 118] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 5. | Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065-2076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 515] [Cited by in RCA: 526] [Article Influence: 35.1] [Reference Citation Analysis (0)] |
| 6. | Stravitz RT, Lee WM. Acute liver failure. Lancet. 2019;394:869-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 572] [Article Influence: 95.3] [Reference Citation Analysis (0)] |
| 7. | Suzuki Y, Suzuki A, Kakisaka K, Takikawa Y. Acute liver failure precipitated by acute Budd-Chiari syndrome and complete portal vein thrombosis. Clin Case Rep. 2021;9:e04326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 8. | Danion J, Genser L, Scatton O. Sleeve Gastrectomy: You Might Lose your Liver! Obes Surg. 2019;29:350-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Plessier A, Darwish-Murad S, Hernandez-Guerra M, Consigny Y, Fabris F, Trebicka J, Heller J, Morard I, Lasser L, Langlet P, Denninger MH, Vidaud D, Condat B, Hadengue A, Primignani M, Garcia-Pagan JC, Janssen HL, Valla D; European Network for Vascular Disorders of the Liver (EN-Vie). Acute portal vein thrombosis unrelated to cirrhosis: a prospective multicenter follow-up study. Hepatology. 2010;51:210-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 390] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 10. | Rudofsky G. [Pathogenesis, diagnosis and therapy of thrombophlebitis and varicophlebitis]. Herz. 1989;14:283-286. [PubMed] |
| 11. | Miceli M, Atoui R, Thertulien R, Barlogie B, Anaissie E, Walker R, Jones-Jackson L. Deep septic thrombophlebitis: an unrecognized cause of relapsing bacteremia in patients with cancer. J Clin Oncol. 2004;22:1529-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Abdallah M, Gohar A, Naryana Gowda S, Abdullah HM, Al-Hajjaj A. Pylephlebitis Associated with Inferior Mesenteric Vein Thrombosis Treated Successfully with Anticoagulation and Antibiotics in a 37-Year-Old Male. Case Rep Gastrointest Med. 2020;2020:3918080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Valerio L, Riva N. Head, Neck, and Abdominopelvic Septic Thrombophlebitis: Current Evidence and Challenges in Diagnosis and Treatment. Hamostaseologie. 2020;40:301-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 14. | Al Duwaiki SM, Al Barwani AS, Taif S. Lemierre's Syndrome. Oman Med J. 2018;33:523-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Lee BK, Ryu HH. A case of pylephlebitis secondary to cecal diverticulitis. J Emerg Med. 2012;42:e81-e85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Guerra F, Dorma MPF, Giuliani G, Caravaglios G, Coratti A. Pylephlebitis: An uncommon complication of sigmoid diverticulitis. Am J Emerg Med. 2023;66:174.e3-174.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 17. | Nouira K, Bedioui H, Azaiez O, Belhiba H, Messaoud MB, Ksantini R, Jouini M, Menif E. Percutaneous drainage of suppurative pylephlebitis complicating acute pancreatitis. Cardiovasc Intervent Radiol. 2007;30:1242-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Levin C, Koren A, Miron D, Lumelsky D, Nussinson E, Siplovich L, Horovitz Y. Pylephlebitis due to perforated appendicitis in a teenager. Eur J Pediatr. 2009;168:633-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Plemmons RM, Dooley DP, Longfield RN. Septic thrombophlebitis of the portal vein (pylephlebitis): diagnosis and management in the modern era. Clin Infect Dis. 1995;21:1114-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 190] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 20. | Jaber MR, Holland C. Septic pylephlebitis mimicking biliary obstruction. Am J Gastroenterol. 2008;103:807-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Plessier A, Rautou PE, Valla DC. Management of hepatic vascular diseases. J Hepatol. 2012;56 Suppl 1:S25-S38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 131] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 22. | Cohoon KP, Heit JA. Inherited and secondary thrombophilia. Circulation. 2014;129:254-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Harmanci O, Bayraktar Y. Portal hypertension due to portal venous thrombosis: etiology, clinical outcomes. World J Gastroenterol. 2007;13:2535-2540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Saxena R, Adolph M, Ziegler JR, Murphy W, Rutecki GW. Pylephlebitis: a case report and review of outcome in the antibiotic era. Am J Gastroenterol. 1996;91:1251-1253. [PubMed] |
| 25. | Choudhry AJ, Baghdadi YM, Amr MA, Alzghari MJ, Jenkins DH, Zielinski MD. Pylephlebitis: a Review of 95 Cases. J Gastrointest Surg. 2016;20:656-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 108] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 26. | Kondo R, Kawaguchi N, McConnell MJ, Sonzogni A, Licini L, Valle C, Bonaffini PA, Sironi S, Alessio MG, Previtali G, Seghezzi M, Zhang X, Sun Z, Utsumi T, Strazzabosco M, Iwakiri Y. Pathological characteristics of liver sinusoidal thrombosis in COVID-19 patients: A series of 43 cases. Hepatol Res. 2021;51:1000-1006. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 27. | Carneiro C, Brito J, Bilreiro C, Barros M, Bahia C, Santiago I, Caseiro-Alves F. All about portal vein: a pictorial display to anatomy, variants and physiopathology. Insights Imaging. 2019;10:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 28. | Ponziani FR, Zocco MA, Campanale C, Rinninella E, Tortora A, Di Maurizio L, Bombardieri G, De Cristofaro R, De Gaetano AM, Landolfi R, Gasbarrini A. Portal vein thrombosis: insight into physiopathology, diagnosis, and treatment. World J Gastroenterol. 2010;16:143-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 227] [Cited by in RCA: 195] [Article Influence: 13.0] [Reference Citation Analysis (2)] |
| 29. | Chang YS, Min SY, Joo SH, Lee SH. Septic thrombophlebitis of the porto-mesenteric veins as a complication of acute appendicitis. World J Gastroenterol. 2008;14:4580-4582. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Garrett A, Carnish E, Das N, Slome M, Measley R. Once universally fatal: pylephlebitis. Am J Med. 2014;127:595-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Baril N, Wren S, Radin R, Ralls P, Stain S. The role of anticoagulation in pylephlebitis. Am J Surg. 1996;172:449-52; discussion 452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 130] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 32. | Naymagon L, Tremblay D, Schiano T, Mascarenhas J. The role of anticoagulation in pylephlebitis: a retrospective examination of characteristics and outcomes. J Thromb Thrombolysis. 2020;49:325-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 33. | Chau NG, Bhatia S, Raman M. Pylephlebitis and pyogenic liver abscesses: a complication of hemorrhoidal banding. Can J Gastroenterol. 2007;21:601-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |