Published online May 27, 2023. doi: 10.4254/wjh.v15.i5.715
Peer-review started: December 19, 2022
First decision: February 21, 2023
Revised: March 2, 2023
Accepted: April 10, 2023
Article in press: April 10, 2023
Published online: May 27, 2023
Processing time: 155 Days and 19.2 Hours
Ventriculoperitoneal (VP) shunt placement has become a standard of care procedure in managing hydrocephalus for drainage and absorption of cerebr
A 49-year-old man with history of congenital hydrocephalus status post bilateral VP shunt placement presented with progressively worsening dyspnea on exertion, abdominal discomfort/distention. Abdominal computed tomography (CT) scan revealed a large CSF pseudocyst in the right hepatic lobe with the tip of VP shunt catheter into the hepatic cyst cavity. Patient underwent robotic laparoscopic cyst fenestration with a partial hepatectomy, and repositioning of VP shunt catheter to the right lower quadrant of the abdomen. Follow-up CT demonstrated a significant reduction in hepatic CSF pseudocyst.
A high index of clinical suspicion is required for early detection of liver CSF pseudocysts since their presentation is often asymptomatic and cunning early in the course. Late-stage liver CSF pseudocysts could have adverse outcomes on the treatment course of hydrocephalus as well as on hepatobiliary dysfunction. There is paucity of data to define the management of liver CSF pseudocyst in current guidelines due to rare nature of this entity. The reported occurrences have been managed by laparotomy with debridement, paracentesis, radiological imaging guided fluid aspiration and laparoscopic-associated cyst fenestration. Robotic surgery is an additional minimally invasive option in the management of hepatic CSF pseudocyst; however, its use is limited by lack of widespread availability and cost of surgery.
Core Tip: Liver cerebrospinal fluid (CSF) pseudocysts are a rare subtype of abdominal cysts that are a late complication of ventriculoperitoneal (VP) shunt. The majority of patients are asymptomatic in early stages, however, as the size of the liver CSF pseudocyst increases this may result in ineffective drainage of CSF, thereby aggravating hydrocephalus symptoms. Liver CSF pseudocyst may be confused with other cystic lesions of liver. Early diagnosis and repositioning VP shunt catheter may prevent both neurological and hepatic complications.
- Citation: Yousaf MN, Naqvi HA, Kane S, Chaudhary FS, Hawksworth J, Nayar VV, Faust TW. Cerebrospinal fluid liver pseudocyst: A bizarre long-term complication of ventriculoperitoneal shunt: A case report. World J Hepatol 2023; 15(5): 715-724
- URL: https://www.wjgnet.com/1948-5182/full/v15/i5/715.htm
- DOI: https://dx.doi.org/10.4254/wjh.v15.i5.715
Hydrocephalus is a condition of excess cerebrospinal fluid (CSF) accumulation into the ventricles of the brain causing neurologic manifestations due to pressure effects of expended ventricles on surrounding neural tissues. Placement of shunts to re-direct CSF has become a treatment option that has significantly improved outcomes and survival of patients with congenital hydrocephalus. Conventionally, shunts can drain CSF fluid into the abdominal peritoneal cavity or right atrium. Drainage of CSF into the right atrium could present with pulmonary emboli which is a life-threatening complication[1]. Numerous studies have determined the presence of ventriculoperitoneal (VP) shunts leading to pulmonary embolism[1]. The primary hypotheses derived from the presence of a foreign body into the heart leading to thrombus formation and CSF creating a procoagulant environment in the heart and lungs. These reasons lead to VP shunts being preferred over right atrial drainage since the peritoneal cavity can absorb fluid efficiently due to larger surface area and better diffusion property of fluids, thus making it a safe and sustainable options for drainage of CSF in the management of hydrocephalus. Generally, due to the increased lifespan of these individuals, complications of the VP shunt are seen later in adulthood. These are associated with abdominal cysts typically at the location of the tip of shunt catheter. A liver CSF pseudocyst is a bizarre long-term complication of this common procedure (VP shunt) that may be confused with other liver cystic lesions. Early diagnosis and repositioning VP shunt catheter may prevent both neurological and hepatic complications.
Patient presented with progressively worsening dyspnea on exertion, abdominal discomfort/distention.
A 49-year-old man with history of intellectual disability due to congenital hydrocephalus status post (s/p) VP shunt placement on right side at 3 mo and left side at 7 years of age, presented with progressively worsening dyspnea on exertion, abdominal discomfort/distention and bilateral lower extremity swelling associated with pain, erythema, and drainage. Patient denied abdominal pain, nausea, vomiting, diarrhea, or constipation. Patients VP shunt placement at 3 mo and 7 years of age never required exchange due to malfunction.
His medical history was also significant for gallstone pancreatitis s/p cholecystectomy.
The patient denied family history of congenital abnormalities or cancers.
On physical examination, vitals were significant for tachycardia (115/min) and elevated blood pressure (151/81 mmHg), while he was afebrile (36.7 °C), saturating 96% on room air and respiratory rate of 18 breaths per min. Physical examination revealed mild abdominal distension, hepatomegaly without abdominal tenderness and bilateral lower extremity edema with mild erythema.
Laboratory work up was significant for mildly elevated glucose 157 mg/dL (65-140 mg/mL), D-dimer 2.20 mcg/mL (0-0.5 mcg/mL) and Hemoglobin A1C 8.5% (4.8%-5.6%). The patient had normal level of aspartate transaminase 27 u/L (0-33 u/L), alanine transaminase 38 u/L (10-49 u/L), total bilirubin 0.5 mg/dL (0.3-1.2 mg/dL), slightly elevated alkaline phosphate 126 u/L (46-116 u/L), and low albumin 3.1 g/dL (3.2-4.8 g/dL).
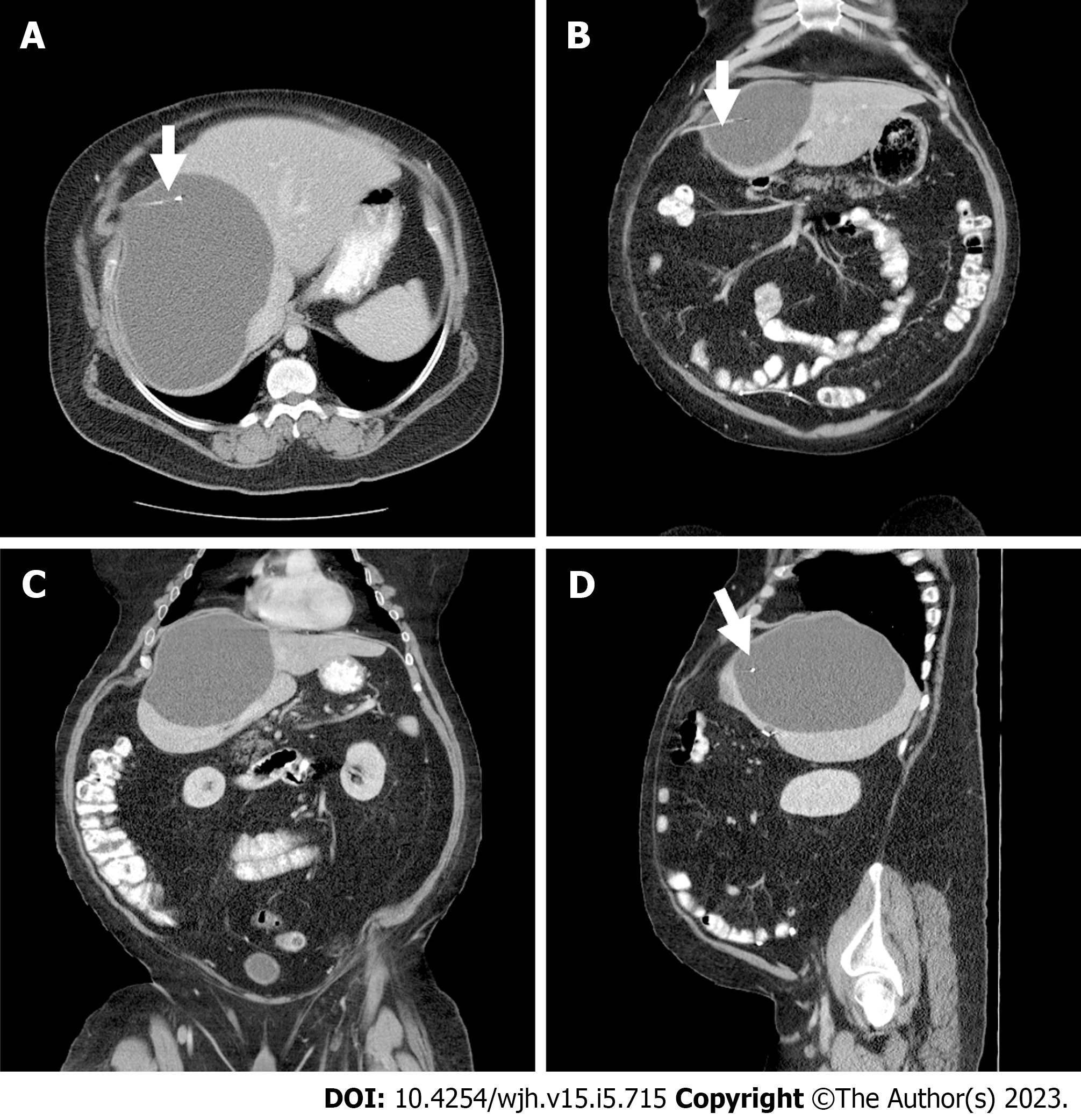
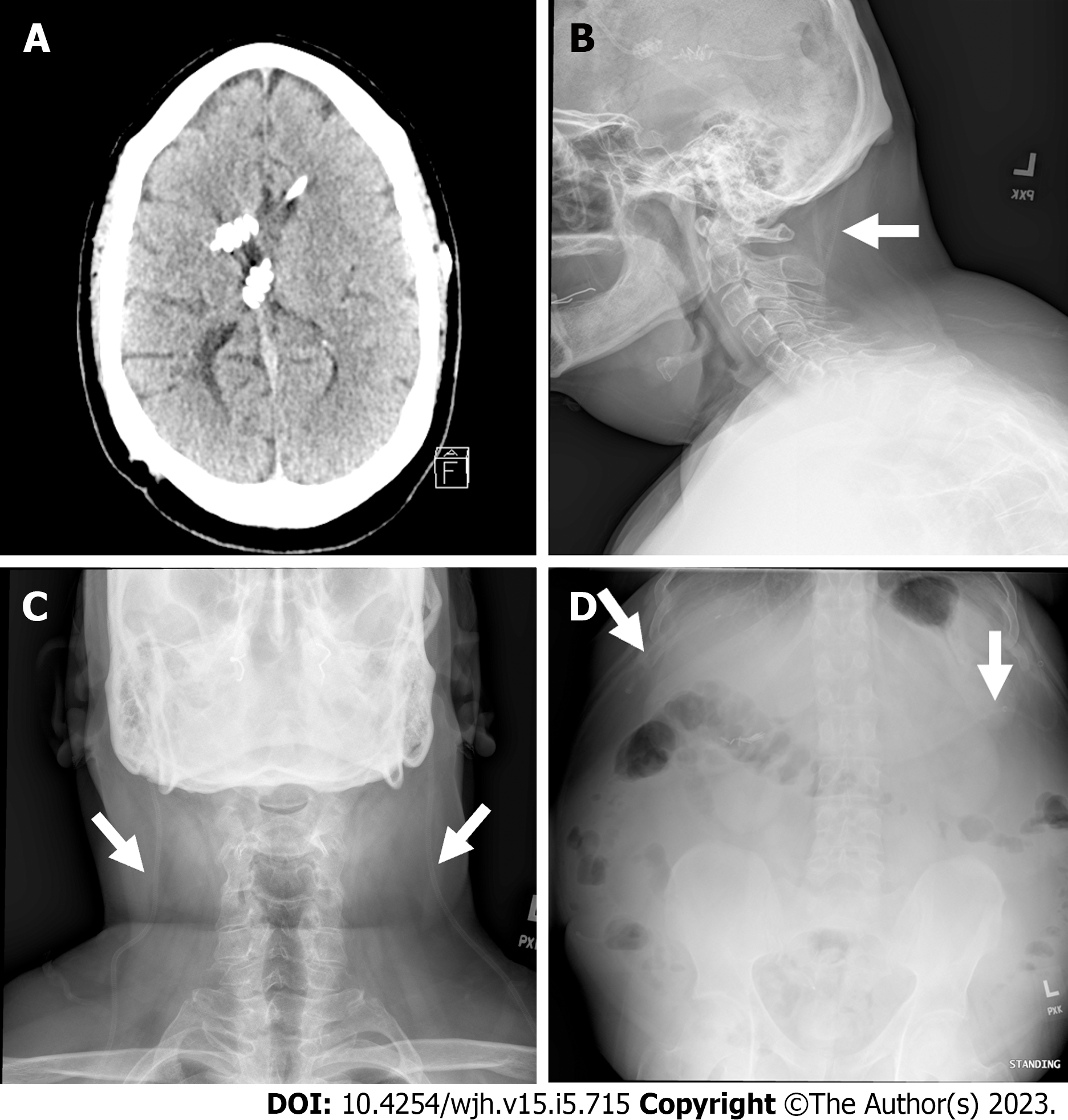
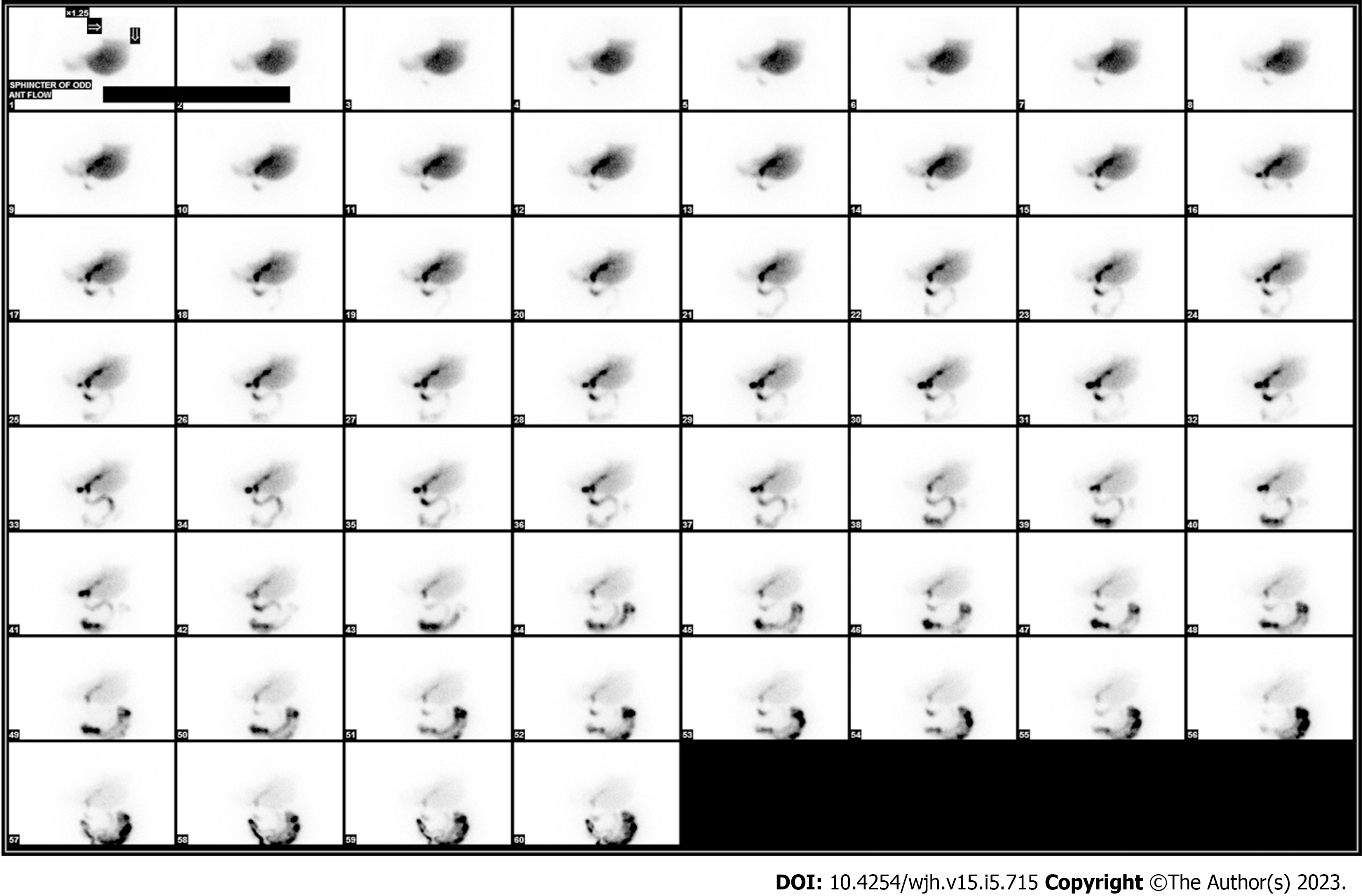
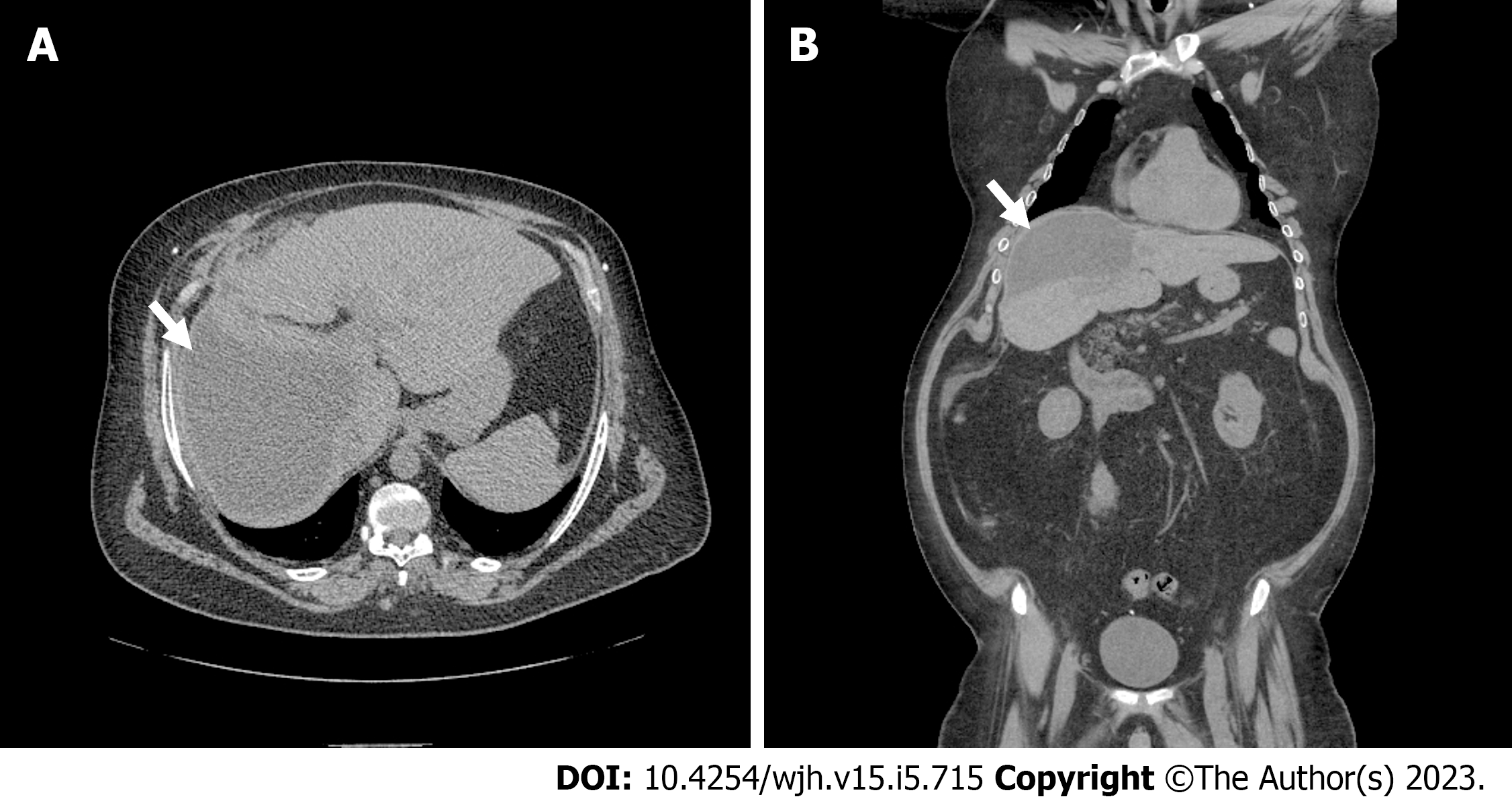
Chest computed tomography (CT) with intravenous contrast was negative for pulmonary embolism however revealed a large 18 cm × 13 cm × 13.5 cm hepatic cyst in the right lobe of liver. A subsequent CT abdomen and pelvis demonstrated a 17.5 cm × 12.6 cm × 12.7 cm cystic lesion in the right hepatic lobe with the tip of VP shunt catheter into the cavity of liver cyst (Figure 1). A head CT was negative for worsening hydrocephalus and confirmed the unchanged position of the intraventricular ends of VP shunt catheters compared to previous radiological imaging of brain (Figure 2A). Shunt series radiographs were also negative for disruption of the VP shunt catheters (Figure 2B-D). A hepatobiliary nuclear scan was unremarkable for biliary leak or sphincter of the Oddi dysfunction (Figure 3).
A diagnosis of bilateral lower extremities cellulitis with incidental right hepatic lobe CSF pseudocyst was made.
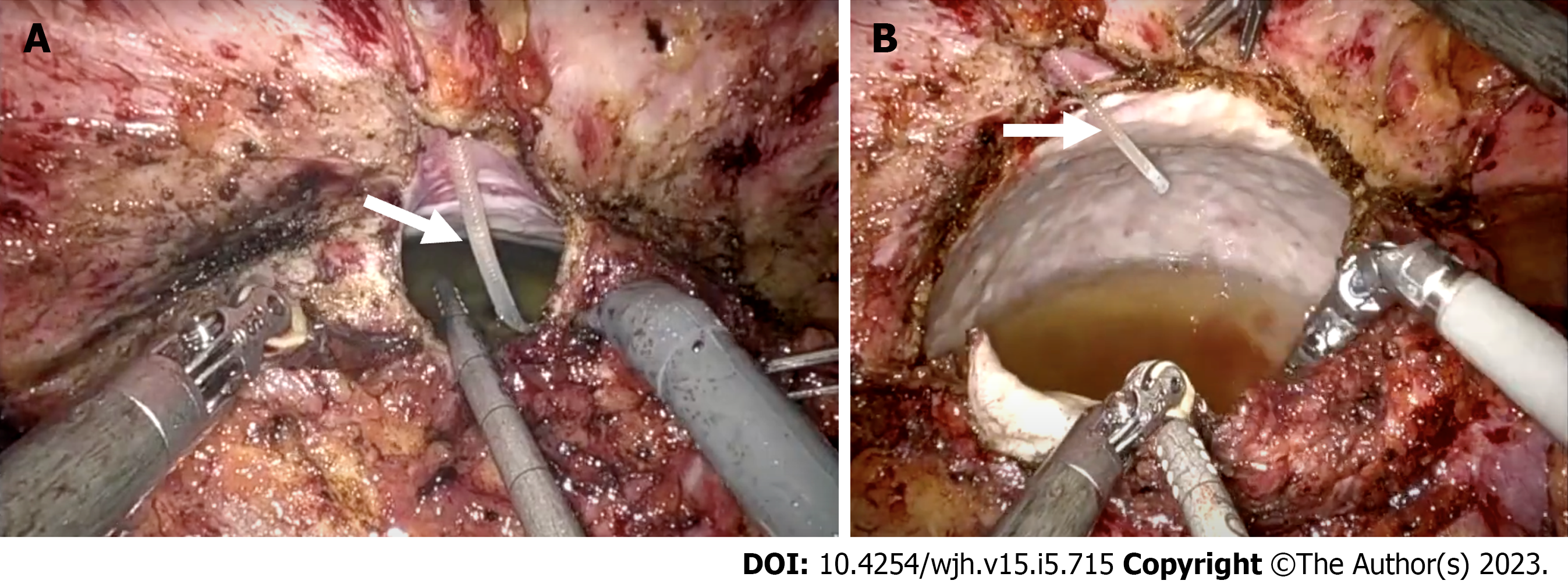
Patient underwent robotic laparoscopic liver cyst fenestration with partial hepatectomy and repositioning of VP shunt catheter to the right lower quadrant of the abdomen (Figure 4). During the procedure, intraoperative ultrasound was used to locate the liver cyst and to evaluate the cyst wall thickness. The cyst cavity was opened and clear cyst fluid was drained into the peritoneal cavity. Multiple other fenestrations were done in the thin walls of the cyst to facilitate further drainage. Cyst fluid was not collected for analysis given it was clear cyst fluid, without noticeable pus, blood, or pseudo-membrane in the cyst cavity concerning for infectious etiology. However, cyst wall biopsy was obtained to rule out malignancy. Patient’s cellulitis was managed with oral clindamycin 300 mg every 6 h for 7 d. His postoperative recovery was uneventful. There was no evidence of malignancy or parasitic infection on hepatic pseudocyst wall biopsy. The patient was discharged home on postoperative day 2.
Follow up abdominal CT scan done 5 wk after hospital discharge showed a significant reduction of right hepatic pseudocyst size 10 cm × 13 cm (Figure 5). On follow up, patient denied abdominal pain, distention/discomfort, and signs of VP shunt malfunction.
Abdominal CSF pseudocyst was first reported in 1954 as a complication of VP shunt[2]. The incidence rate of these pseudocysts ranges from 0.25% to 10%[3,4]. However, hepatic CSF pseudocysts are extremely uncommon and only scant number of cases were reported in the medical literature (Table 1)[2-28]. The etiology of liver CSF pseudocysts associated with VP shunts is unknown, however, inflammation triggered with prolonged irritation of hepatic surface and peritoneum due to shunt catheter is the proposed mechanism resulting in pseudocyst formation[4,9,10]. Infective complications of pseudocysts are observed in very few cases and are typically caused by Staphylococcus aureus, followed by S. epidermidis, Escherichia coli, Salmonella typhi, Propionibacterium acnes, Streptococcus faecalis, Acinetobacter sp. and Pseudomonas aeruginosa[4,6,10,18]. The proposed pathogenesis of pseudocyst infection with intestinal and dermal bacteria results from systemic and localized inflammation around VP shunt catheter. Several risk factors such as abdominal trauma, abdominal surgeries, repeated shunt revisions, peritoneal adhesions, ascites and peritonitis predispose to CSF-pseudocyst infection[4,6,10,18].
| Ref. | Year | Age | Sex | Cyst location | Etiology of hydrocephalus | Treatment | Follow-up (wk) | Outcome |
| Current case | 2023 | 49 | M | Intra-axial | Congenital | Robotic laparoscopic pseudocyst fenestration, partial hepatectomy, and a repositioning of VPS | 4 | Complete resolution of symptoms without any complications |
| Achufusi et al[5] | 2020 | 39 | F | N/A | Congenital | Laparotomy with pseudocyst drainage followed by removal of VPS and insertion of new VPS | Complete resolution of pseudocyst; no recurrence | |
| Arsanious and Sribnick[8] | 2019 | 21 | F | N/A | Meningitis | Laparotomy and pseudocyst drainage with externalization and repositioning of VPS | 6 | Complete resolution of pseudocyst; no recurrence |
| Koide et al[6] | 2019 | 12 | M | Extra-axial | Myelomeningocele | US-PCA of pseudocyst with externalization of VPS followed by reinsertion of new VPS | 3 | Complete resolution of pseudocyst; no recurrence |
| Bettis et al[7] | 2019 | 56 | M | Intra-axial | Trauma | N/A | N/A | N/A |
| Canaz et al[9] | 2017 | 34 | F | Extra-axial | NPH | Laparotomy and pseudocyst drainage followed by repositioning of VPS | 36 | Spontaneous resolution of hepatic CSF pseudocysts |
| Canaz et al[9] | 2017 | 25 | F | Extra-axial | Meningitis | Laparotomy and pseudocyst drainage followed by repositioning of VPS | 24 | Pseudocysts were spontaneously reabsorbed and post op CSF culture showed cyst fluid was sterile |
| Tomiyama et al[10] | 2014 | 50 | F | N/A | SAH | VPS removal and reinsertion and cyst drainage | 8 | No recurrence of intraperitoneal pseudocyst on post-operative abdominal scans and improvement in hydrocephalus on brain CT |
| Dabdoub et al[4] | 2013 | 40 | M | Intra-axial | Trauma | VPS removal and reinsertion and cyst drainage | 36 | No clinical recurrence of hepatic CSF pseudocysts |
| Verma et al[11] | 2012 | 35 | M | Intra- and extra-axial | Tumor | Pseudocyst aspiration and externalization of shunt followed by reinsertion | 3 | Complete resolution of cyst on abdominal ultrasound |
| Berkmann et al[13] | 2011 | 34 | F | N/A | Congenital | Laparoscopic shunt removal and new shunt re-insertion | 24 | No recurrence and no adverse events |
| Peltier et al[12] | 2011 | 49 | M | Extra-axial | Meningitis | Ultrasound guided aspiration and repositioning of shunt | 1 | Complete resolution of the cyst; no recurrence |
| Faraj et al[3] | 2011 | 18 | M | Intra-axial | Bacterial meningitis | Laparotomy and pseudocyst drainage followed by repositioning of shunt | N/A | Patient made a full recovery |
| Kolić et al[14] | 2010 | 30 | F | Intra-axial | SAH | Ultrasound guided aspiration and external ventricular drainage | 4 | Patient died due to sepsis- 1 mo after hepatic CSF pseudocyst drainage |
| Aparici-Robles and Molina-Fabrega[15] | 2008 | 22-50 | F (4), M (2) | Intra-axial | Abscess; tumor; meningitis; and SAH | Laparotomy with pseudocyst drainage and repositioning of shunt | Relapse in 2 out of 6 patients (5-6 mo) | |
| Banka et al[17] | 2007 | 7 | M | N/A | Myelomeningocele | Repositioning of shunt | ||
| Kaplan et al[16] | 2007 | 10 | F | Extra-axial | Tumor | Laparotomy and pseudocyst drainage followed by repositioning of shunt | ||
| Hsieh et al[18] | 2006 | 39 | M | Extra-axial | Trauma | Externalization of shunt followed by reinsertion | Patient made full recovery and cysts were fully resolved (1 mo) | |
| Koçak et al[28] | 2004 | 15 | F | Extra-axial | Tuberculosis meningitis | Ultrasound aspiration and distal end removal followed by new shunt reinsertion | Almost complete resolution of the cyst observed after 1 wk | |
| Chitkara et al[19] | 2004 | 5 | F | Intra-axial | Noncommunicating | Externalization of shunt followed by reinsertion | Follow up done at 3 mo- patient was entirely asymptomatic and cyst had completely resolved | |
| Kumar et al[20] | 1995 | 23 | M | N/A | Meningitis | Ultrasound aspiration and distal end removal | ||
| Engelhard and Miller[21] | 1992 | 20 | M | N/A | Congenital | Removal of shunt and reinsertion | ||
| Wang and Miller[22] | 1989 | 3 | M | Extra-axial | Congenital | Pseudocyst resection and distal end revision | N/A | |
| Touho et al[24] | 1987 | 66 | M | N/A | Trauma | Repositioning of shunt | ||
| Wolbers et al[23] | 1987 | 29 | F | Extra-axial | Tumor | Repositioning of shunt | Patient made full recovery(2 yrs) | |
| Rana et al[25] | 1985 | 12 | M | Intra-axial | Tumor | Repositioning of shunt | Complete resolution of cyst in follow up CT scan | |
| Latchaw and Hahn[26] | 1981 | 40 | M | Intra-axial | Aqueductal stenosis | Drainage of hepatic pseudocyst and repositioning of the shunt | ||
| Fischer and Shillito[27] | 1969 | 3 | F | Extra-axial | Aqueductal stenosis | Drainage of hepatic pseudocyst and lumboperitoneal shunt | Patient did not experience or report any adverse complications (10 mo) |
Patients with small abdominal pseudocysts remain asymptomatic however those with larger pseudocysts commonly present with abdominal pain (63%), abdominal distention (37%), abdominal tenderness (31%) and abdominal mass (29%) on initial presentation[18]. The abdominal pain may be severe and diffuse, with a point of maximal intensity located at the terminal site of catheter, usually in the right or left upper quadrant of abdomen. A subset of patients may also have associated symptoms such as constipation, nausea or vomiting[4]. Since majority of the affected population is pediatric, the presenting symptoms tend to be related to increased intracranial pressure such as lethargy, headaches and altered mental status[9]. However, these symptoms are infrequent in adults who typically present with pain/pressure related symptoms depending upon location of the cyst or VP shunt catheter tip. The diagnosis is typically made using radiological modalities, however abdominal ultrasound is the initial diagnostic modality[4,5]. Abdominal CT scan is the preferred radiological imaging because it provides information on the characterization of cyst size, location, and position of the VP shunt catheter. It also helps to differentiate other possible etiologies of abdominal pain[4]. Rarely, in adults who present with altered mental status, CT scan of the head may be sought out to evaluate location of proximal end of VP shunt catheter, status of ventricular dilation and to rule out other intracranial abnormalities.
The liver CSF pseudocysts are broadly classified as intra or extra axial[4]. The intra-axial liver pseudocysts are those found within the hepatic parenchyma with the VP shunt tip lodged within the liver. The extra-axial liver pseudocysts are usually located under the hepatic subcapsular space due to penetration of the VP shunt tip in the Glisson’s capsule. The symptomatic clinical presentation is seen in the fourth or fifth decade of life[2-28]. The cysts have thus far also shown an equal male/female predominance[2-28]. There was an even distribution of the incidence of intra-axial and extra-axial location[2-28]. The patients in the reported cases had a range of etiologies for their hydrocephalus such as infectious, congenital, traumatic, and mechanical/obstructive leading to the shunt placement[6].
The characteristics and clinical presentation of our case is similar to previously reported cases of intra-axial hepatic CSF pseudocysts. However, duration since VP shunt placement to clinical presentation is relatively longer compared to previously reported cases. This is likely due to lack of predisposing risk factors in our case such as no prior history of abdominal surgery, trauma, peritonitis, ascites and his VP shunt catheter never required revision. Although liver CSF pseudocyst was identified on the CT chest, however, a dedicated CT abdomen pelvis is essential for evaluation of other abdominal cysts/collection and planning for surgical repositioning of VP shunt catheter.
The management of liver CSF pseudocyst is controversial because of rarity of disease[5,7,9]. In asymptomatic individuals wherein the cyst is an incidental finding on abdominal imaging, the consensus is expectant management with routine monitoring with abdominal ultrasound or radiological imaging[9]. The duration of surveillance imaging is unclear in the current literature. It is reasonable to performs ultrasound abdomen in 1-2 year for monitoring of pseudocyst size and planning of further treatment with conservative vs surgical approach. In symptomatic patients, management is variable ranging from robotic or laparoscopic repositioning/exchange of VP shunt catheter with or without cyst fenestration and antibiotic therapy[4,10]. Management is patient specific and varies on a case-by-case basis. Typically, a CT-guided biopsy is performed for a diagnostic purpose. If the biopsy reveals an infection, treatment involves antibiotic therapy as well as shunt externalization till the infection clears[4]. The shunt is repositioned during externalization after infection treatment. Depending upon the availability of expertise, the liver CSF pseudocysts are managed with elective laparoscopic excision of pseudocyst, debridement of cystic wall and/or reposition the VP shunt catheter in the lower quadrant of abdomen. The majority of case studies managed the liver CSF pseudocyst with surgical or ultrasound guided drainage, the VP shunt was removed and/or repositioned along with cyst drainage[4-6,8-10].
In the present case robotic laparoscopic cyst fenestration with partial hepatectomy and repositioning of VP shunt catheter was performed. Robotic surgery has several advantages over other surgical options such as wide cyst fenestrations could be achieved with robotic ergonomics that provide magnified three-dimensional view and enables access to cysts located in posterosuperior segments of liver[29]. Recurrence rate after robotic fenestration is lower than conventional laparoscopic or other surgical approaches as wristed technology of robotic surgery overcomes limitations of other surgical options[29]. The dual console system of robotic surgery plays an important role in surgical training by enabling direct mentorship to trainee where one click on button swap the control between trainee and mentors. Taken together, robotic surgery assisted cyst fenestration/deroofing is a safe and feasible approach in the management of hepatic CSF pseudocysts. The utility of robotic surgery should be balanced with cost, limited worldwide availability of robotic technology and expertise.
The pseudocysts that have been documented thus far have had a good prognosis, with near complete or complete resolution of symptoms at follow up appointments that were between 3 to 9 wk[2-28]. In our case there was a significant reduction of cyst size on follow up CT scan of abdomen. Most of the cysts (12 out of 15 case studies) showed near complete or complete resolution of hepatic CSF pseudocysts with either surgical or ultrasound guided drainage, however clinical characteristics and etiology of cysts are variable with no specific differences in clinical variables (Table 1)[2-28]. Large prospective studies are required to further investigate clinical characteristic of patients who will benefit surgical vs conservative approach for spontaneous resolution of hepatic CSF pseudocysts. Rare nature of hepatic CSF pseudocyst is predominant roadblock for conducting prospective studies. The physician dependent treatment plan had similar outcomes in both groups of patients, except that the self-absorbing cysts took longer to resolve (about 9 mo vs immediately after surgical procedure)[9]. The physician dependent treatment plan in managing patients with hepatic CSF pseudocyst is dependent on several factors, including the severity of symptoms, the size and location of the pseudocyst, the patient's overall health, and the physician's expertise to determine, surgical vs non-surgical management. Patients with acute illness, larger size pseudocyst and persistent symptoms despite conservative management, may benefit from surgical approach. The recurrence rate of the liver CSF pseudocysts on short term follow up is low. Only one case study has reported recurrent pseudocyst in 2 out of 6 patients. A fatal outcome due to sepsis was reported in on case study[14].
Liver CSF pseudocysts are a rare subtype of abdominal cysts that are a late complication of VP shunt. The majority of patients are asymptomatic in early stages, though larger liver CSF pseudocyst may result in ineffective drainage of CSF, thereby aggravating hydrocephalus symptoms. In asymptomatic patients with hepatic CSF pseudocysts, it is reasonable to performs ultrasound abdomen in 1-2 year for monitoring of pseudocyst size and planning of further treatment with conservative vs surgical approach. While there is no current consensus on the optimal treatment modality, however, laparoscopic drainage with repositioning of shunt catheter has favorable outcomes. Robotic surgery is an additional minimally invasive option in the management of hepatic CSF pseudocyst; however, its use is limited by lack of widespread availability and cost of surgery.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Society for Gastrointestinal Endoscopy; American College of Gastroenterology; American Gastroenterological Association; and American Association for the Study of Liver Diseases.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Masuda S, Japan; Sarr MG, United States S-Editor: Hu YR L-Editor: A P-Editor: Cai YX
| 1. | Wu D, Guan Z, Xiao L, Li D. Thrombosis associated with ventriculoatrial shunts. Neurosurg Rev. 2022;45:1111-1122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 2. | Harsh GR 3rd. Peritoneal shunt for hydrocephalus, utilizing the fimbria of the fallopian tube for entrance to the peritoneal cavity. J Neurosurg. 1954;11:284-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 66] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Faraj W, Ahmad HH, Mukherji D, Khalife M. Hepatic cerebrospinal fluid pseudocyst mimicking hydatid liver disease: a case report. J Med Case Rep. 2011;5:475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Dabdoub CB, Fontoura EA, Santos EA, Romero PC, Diniz CA. Hepatic cerebrospinal fluid pseudocyst: A rare complication of ventriculoperitoneal shunt. Surg Neurol Int. 2013;4:162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Achufusi TGO, Chebaya P, Rawlins S. Abdominal Cerebrospinal Fluid Pseudocyst as a Complication of Ventriculoperitoneal Shunt Placement. Cureus. 2020;12:e9363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Koide Y, Osako T, Kameda M, Ihoriya H, Yamamoto H, Fujisaki N, Aokage T, Yumoto T, Date I, Naito H, Nakao A. Huge abdominal cerebrospinal fluid pseudocyst following ventriculoperitoneal shunt: a case report. J Med Case Rep. 2019;13:361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Bettis T, Holsten S, Mitchell A. Conservative Management of a Hepatic CSF Pseudocyst in an Asymptomatic Patient. Am Surg. 2019;85:e389-e391. [PubMed] |
| 8. | Arsanious D, Sribnick E. Intrahepatic Cerebrospinal Fluid Pseudocyst: A Case Report and Systematic Review. World Neurosurg. 2019;125:111-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Canaz G, Emel E, Baydin S, Ulukent SC, Ozgunduz Y, Cevik OM. Safe surgical approach to extrahepatic pseudocyst, a rare shunt complication: 2 case reports. Chin Neurosurg J. 2017;3:36. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Tomiyama A, Harashina J, Kimura H, Ito K, Honda Y, Yanai H, Iwabuchi S. An Intra-Abdominal Pseudocyst around a Ventriculoperitoneal Shunt due to Streptococcus Infection 7 Years after Shunt Surgery. Surg Res Pract. 2014;2014:898510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Verma A, Mohan S, Gupta A. Ventriculo-peritoneal shunts can cause liver injury, juxta and intrahepatic pseudocysts: imaging findings and review of literature. Clin Neurol Neurosurg. 2012;114:389-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Peltier J, Demuynck F, Fichten A, Lefranc M, Toussaint P, Desenclos C, Nicot B, Pruvot AS, Le Gars D. Non-traumatic pseudocyst of Glisson capsule complicating a ventriculoperitoneal shunt. Neurochirurgie. 2011;57:31-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Berkmann S, Schreiber V, Khamis A. Recurrent intrahepatic dislocation of ventriculoperitoneal shunt. Minim Invasive Neurosurg. 2011;54:83-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Kolić Z, Kukuljan M, Bonifačić D, Vukas D. CSF liver pseudocyst as a complication of a ventriculoperitoneal shunt. Wien Klin Wochenschr. 2010;122:641-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Aparici-Robles F, Molina-Fabrega R. Abdominal cerebrospinal fluid pseudocyst: a complication of ventriculoperitoneal shunts in adults. J Med Imaging Radiat Oncol. 2008;52:40-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Kaplan M, Ozel SK, Akgun B, Kazez A, Kaplan S. Hepatic pseudocyst as a result of ventriculoperitoneal shunts: case report and review of the literature. Pediatr Neurosurg. 2007;43:501-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Banka S, Johnson K, Sgouros S. Liver cyst caused by the peritoneal catheter of a CSF shunt. Pediatr Neurosurg. 2007;43:444-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Hsieh CT, Pai CC, Tsai TH, Chiang YH, Su YH. Hepatic cerebrospinal fluid pseudocyst: a case report and review of the literature. Neurol India. 2006;54:86-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Chitkara N, Gupta R, Singla SL, Sharma NK. Lower end of ventriculoperitoneal shunt embedding in liver parenchyma. Neurol India. 2004;52:405. [PubMed] |
| 20. | Kumar MM, Jeyabalachandran M, Sekar S. Intrahepatic cyst--a complication of ventriculoperitoneal shunt. J Indian Med Assoc. 1995;93:403. [PubMed] |
| 21. | Engelhard HH, Miller FB. Abdominal pain resulting from cerebrospinal fluid pseudocyst and cholelithiasis. South Med J. 1992;85:851-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Wang F, Miller JH. Cerebrospinal fluid pseudocyst presenting as a hepatic mass: a complication of ventriculoperitoneal shunt. Pediatr Radiol. 1989;19:326-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Wolbers JG, van Zanten TE, van Alphen HA. Ventriculo-peritoneal shunt procedure complicated by liver capsule perforation. A case report. Clin Neurol Neurosurg. 1987;89:55-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Touho H, Nakauchi M, Tasawa T, Nakagawa J, Karasawa J. Intrahepatic migration of a peritoneal shunt catheter: case report. Neurosurgery. 1987;21:258-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Rana SR, Quivers ES, Haddy TB. Hepatic cyst associated with ventriculoperitoneal shunt in a child with brain tumor. Childs Nerv Syst. 1985;1:349-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Latchaw JP Jr, Hahn JF. Intraperitoneal pseudocyst associated with peritoneal shunt. Neurosurgery. 1981;8:469-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Fischer EG, Shillito J Jr. Large abdominal cysts: a complication of peritoneal shunts. Report of three cases. J Neurosurg. 1969;31:441-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Koçak A, Baysal T, Çaylı SR, Ateş O, Önal Ç. An unusual complication of ventriculo peritoneal shunt: Cerebrospinal fluid cyst in liver. Eur J Radiol. 2004;21-24. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 29. | Tsirlis T, Thakkar R, Sen G, Logue J, Robinson S, French JJ, White SA. Robotic fenestration of massive liver cysts using EndoWrist technology. Int J Med Robot. 2019;15:e1994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |