Published online Feb 27, 2023. doi: 10.4254/wjh.v15.i2.282
Peer-review started: November 4, 2022
First decision: January 3, 2023
Revised: January 15, 2023
Accepted: February 7, 2023
Article in press: February 7, 2023
Published online: February 27, 2023
Processing time: 111 Days and 19 Hours
Alcoholic liver disease (ALD) remains one of the major indications for liver transplantation in the United States and continues to place a burden on the na
To assess the trends for ALD admissions during the COVID-19 pandemic, and compare it to a similar pre-pandemic period.
This retrospective study analyzed all admissions at a tertiary health care system, which includes four regional hospitals. ALD admissions were identified by querying a multi-hospital health system’s electronic database using ICD-10 codes. ALD admissions were compared for two one-year periods; pre-COVID-19 from April 2019 to March 2020, and during-COVID-19 from April 2020 to March 2021. Data were analyzed using a Poisson regression model and admission rates were compared using the annual quarterly average for the two time periods, with stratification by age and gender. Percent increase or decrease in admissions from the Poisson regression model were reported as incident rate ratios.
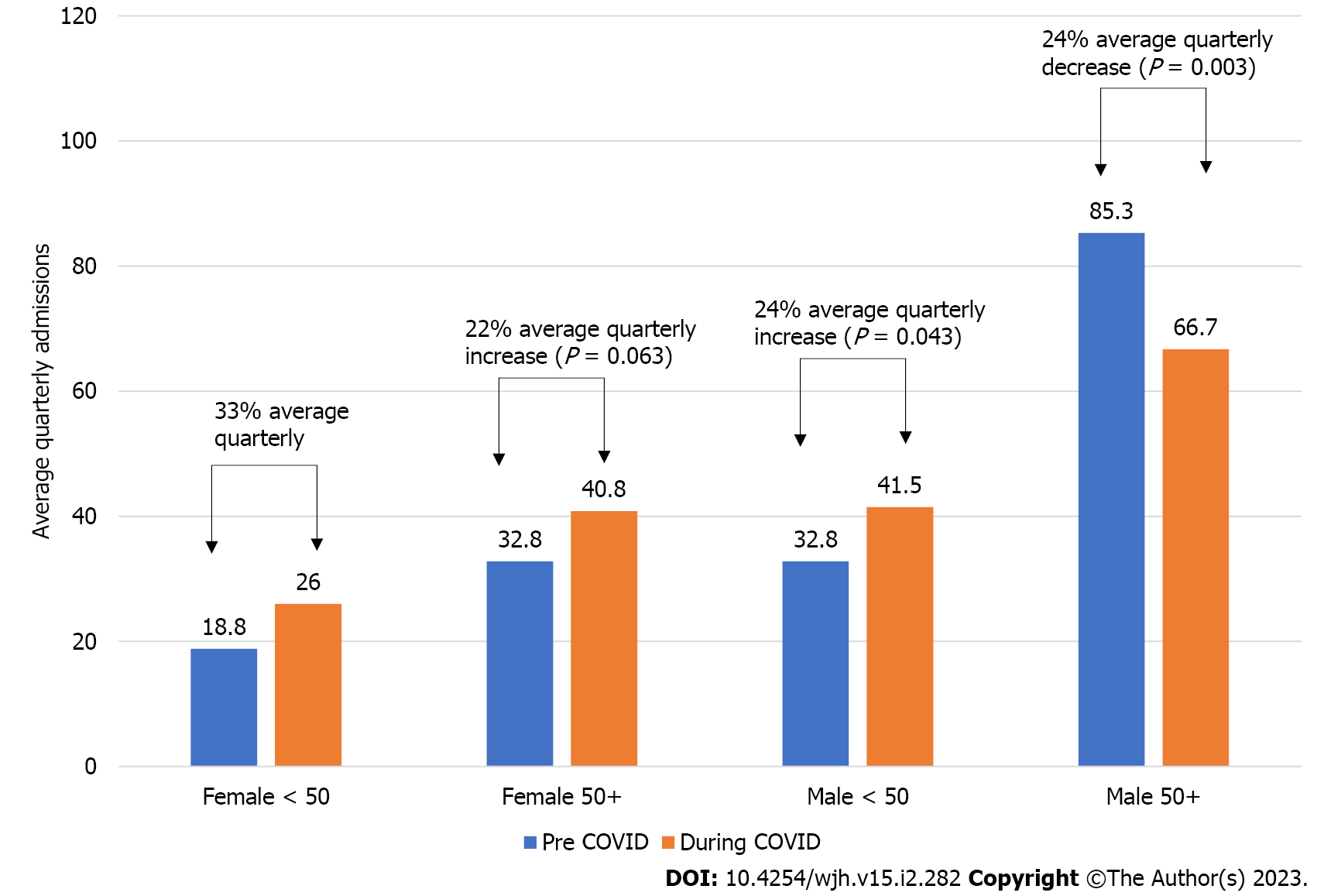
One thousand three hundred and seventy-eight admissions for ALD were included. 80.7% were Caucasian, and 34.3% were female. An increase in the number of admissions for ALD during the COVID-19 pandemic was detected. Among women, a sharp rise (33%) was noted in those below the age of 50 years, and an increase of 22% in those above 50 years. Among men, an increase of 24% was seen for those below 50 years, and a 24% decrease in those above 50 years.
The COVID-19 pandemic has had widespread implications, and an increase in ALD admissions is just one of them. However, given that women are often prone to rapid progression of ALD, this finding has important preventive health implications.
Core Tip: An increase in alcoholic liver disease admissions was observed in the first year of the pandemic compared to the year prior to the pandemic with various “lock-downs” in place. This trend was most pronounced in the cohort of women below the age of 50.
- Citation: Campbell JP, Jahagirdar V, Muhanna A, Kennedy KF, Helzberg JH. Hospitalizations for alcoholic liver disease during the COVID-19 pandemic increased more for women, especially young women, compared to men. World J Hepatol 2023; 15(2): 282-288
- URL: https://www.wjgnet.com/1948-5182/full/v15/i2/282.htm
- DOI: https://dx.doi.org/10.4254/wjh.v15.i2.282
The spectrum of alcoholic liver disease (ALD) includes an array of pathologies, from reversible fatty liver, to alcoholic hepatitis and advanced cirrhosis with portal hypertension[1]. Although women have lower and less active alcohol dehydrogenase in the GI tract and liver compared to men, ALD has traditionally been a disease primarily of middle-aged and older men[2]. A study by Shirazi et al[3], analyzing the National Inpatient Sample from 2007-2014 showed significantly higher hospitalization rates in males vs females, for alcohol associated hepatitis and cirrhosis.
The coronavirus disease 2019 (COVID-19) pandemic has had deep and far reaching consequences on people across the globe, affecting individuals at personal, economic, and social levels. It is alleged to have provoked more significant financial and emotional hardships on women compared to men[4,5]. During the initial phase of the pandemic, liquor stores in the United States were considered essential businesses, and alcohol sales increased by more than 34%[6]. The current study was designed to evaluate whether increased alcohol consumption during the COVID-19 pandemic was associated with an increase in ALD admissions, particularly in women.
An IRB exception was obtained for this study, prior to any data acquisition or analysis. Admissions to a multi-hospital health system for ALD were compared for two one-year periods [April 2019-March 2020 (pre-COVID-19, “PC”) and April 2020-March 2021 (during-COVID-19, “COV”)]. One thousand three hundred and seventy-eight admissions from the four regional hospitals for ALD were identified by querying an electronic database using the International Classification of Diseases (ICD-10) codes (K70 and its sub-categories representing the spectrum of alcoholic fatty liver, hepatitis, cirrhosis, fibrosis). Patients with more than one or overlapping diagnoses were only counted once. Data were analyzed using a Poisson regression model and admission rates were compared using the annual quarterly average for the two time periods, with stratification by age and gender. Percent increase or decrease in admissions from the Poisson regression model were reported as incident rate ratios. Continuous variables were compared using Student’s t-test, while categorical variables were compared using chi-square of Fisher’s exact test. All data were analyzed using SAS v9.4 software (Cary, NC).
Comparing admissions for ALD pre-COVID-19 (PC) and during-COVID-19 (COV) periods, an average quarterly increase of 33% was identified in women below 50 years (75 PC vs 104 COV, P = 0.031), and an increase of 22% in women above 50 years (131 PC vs 163 COV, P = 0.063). During the same two periods, ALD admissions for men below 50 years increased 24% (131 PC vs 166 COV, P = 0.043) (Figure 1).
Interestingly, a 24% decrease in admissions for ALD was observed in males above 50 years (341 PC vs 267 COV, P = 0.003). Although this group had the greatest number of hospitalizations, a significant proportional decline was observed among them, compared to the other groups.
The total number of admissions for ALD in men and women only increased from 678 pre-COVID-19 to 709 during-COVID-19 (Table 1). Strikingly, the proportion of women increased from 30.4% (n = 206) to 38.1% (n = 267), demonstrating an increase of 29% (P = 0.005). Total admissions for males decreased from 69.6% (n = 472) to 61.9% (n = 433), a 9% decrease (P = 0.195).
| Variable | Total (n = 1378) | COVID-19 period (n = 700) | Pre-COVID-19 period (n = 678) | P value |
| Age (yr) | 53.9 ± 13.1 | 53.1 ± 12.9 | 54.7 ± 13.2 | 0.025 |
| Gender | 0.002 | |||
| Female | 473 (34.3%) | 267 (38.1%) | 206 (30.4%) | |
| Male | 905 (65.7%) | 433 (61.9%) | 472 (69.6%) | |
| Race | 0.628 | |||
| Black or African American | 168 (12.2%) | 91 (13.0%) | 77 (11.4%) | |
| White or Caucasian | 1112 (80.7%) | 559 (79.9%) | 553 (81.6%) | |
| Diagnosis name | 0.274 | |||
| Alcoholic cirrhosis of liver with ascites | 491 (35.6%) | 246 (35.1%) | 245 (36.1%) | |
| Alcoholic cirrhosis of liver without ascites | 336 (24.4%) | 164 (23.4%) | 172 (25.4%) | |
| Alcoholic fatty liver | 43 (3.1%) | 20 (2.9%) | 23 (3.4%) | |
| Alcoholic fibrosis and sclerosis of liver | 1 (0.1%) | 0 (0.0%) | 1 (0.1%) | |
| Alcoholic hepatic failure with coma | 4 (0.3%) | 3 (0.4%) | 1 (0.1%) | |
| Alcoholic hepatic failure without coma | 141 (10.2%) | 79 (11.3%) | 62 (9.1%) | |
| Alcoholic hepatitis with ascites | 85 (6.2%) | 52 (7.4%) | 33 (4.9%) | |
| Alcoholic hepatitis without ascites | 205 (14.9%) | 105 (15.0%) | 100 (14.7%) | |
| Alcoholic liver disease, unspecified | 72 (5.2%) | 31 (4.4%) | 41 (6.0%) | |
| Discharge disposition | 0.034 | |||
| Expired | 57 (4.2%) | 34 (4.9%) | 23 (3.4%) | |
| Home or self-care | 832 (60.6%) | 412 (59.1%) | 420 (62.1%) | |
| Home-health care service | 154 (11.2%) | 86 (12.3%) | 68 (10.1%) | |
| Hospice/home | 30 (2.2%) | 16 (2.3%) | 14 (2.1%) | |
| Hospice/medical facility | 38 (2.8%) | 14 (2.0%) | 24 (3.6%) | |
| Left against medical advice | 47 (3.4%) | 30 (4.3%) | 17 (2.5%) | |
| Rehab facility | 29 (2.1%) | 18 (2.6%) | 11 (1.6%) | |
| Short term hospital | 58 (4.2%) | 34 (4.9%) | 24 (3.6%) | |
| Skilled nursing facility | 76 (5.5%) | 35 (5.0%) | 41 (6.1%) |
No significant racial/ethnic difference was identified, with the majority of the patients being Caucasian (80.7%). Approximately 35% of patients in both groups were decompensated with ascites. For patients with ALD, the length of stay during the pandemic was higher than pre-pandemic (110 h vs 96 h, P = 0.014). Interestingly, during the COVID-19 period, more patients left the hospital prematurely, against medical advice (4.3% vs 2.5%, P = 0.03). A higher proportion of patients were discharged to a rehabilitation facility during the pandemic as well (2.6% vs 1.5%, P = 0.03).
The current study, comparing the pre-COVID and during-COVID periods, detected a significant increase in the number of ALD hospital admissions for both women and men below the age of 50 years (33% and 24% increase respectively). With the onset of stressors including those brought by prolonged social isolation and socio-economic instability associated with the pandemic, an increase in substance abuse, not only among the high-risk groups, but also in the general population is not surprising and has been described[7].
Importantly, a significant increase in the number of younger women requiring admission for ALD was identified. To a lesser extent, this trend was observed in women over 50 years of age as well. The contextual, environmental, and social influences impacting alcohol consumption during the COVID-19 pandemic have not been comprehensively evaluated. The current study identified multiple significant trends that are likely related to psychosocial factors and social processes the study was not designed to evaluate. Previous studies have suggested anxiety and depression may be more prevalent in women than men, and the uncertainties during the pandemic may have compounded this[8]. A national survey reported a significant impact of the pandemic on the mental health of women, with 1 in 5 women respondents reporting an increase in alcohol or drug use after the onset of the COVID-19 outbreak[9]. One can speculate the increased consumption of alcohol could be related to stresses in the home added to existing marital responsibilities including: Stresses associated with both partners working remotely, the added stress of having children in the home, and the responsibilities associated with coordinating education for remote learning. The traditional gender gap in alcohol use also tends to be narrowing. A study by Williams et al[10] examining heavy drinking trajectories demonstrated an increase in heavy drinking frequency among younger women. These trends are concerning, given that women are not only at a higher risk of developing liver disease with alcohol intake, but are also at increased risk for progression of ALD with increasing alcohol intake compared to men[11]. Differences in gastric alcohol dehydrogenase levels and body fat are thought to be the reason behind this gender difference. A recent study by Bertha et al[11], analyzing a national inpatient database, reported that although ALD is seen predominantly in men, there has been a disproportionate increase in ALD mortality among women. Specifically, mortality in women below 34 years has progressed at a significantly high rate[1].
Another trend the current study identified was a decrease in ALD hospitalizations for older males during the COVID-19 pandemic. During the pandemic many individuals made every attempt to avoid hospital visits. Men are especially prone to denial of symptoms and avoidance of healthcare. It is also plausible that the overall consumption of alcoholic beverages by men decreased during the pandemic while increasing in women. Davies et al[12] found that drinking in the home with a partner, compared to drinking outside the home, is associated with lower consumption of alcohol. With the temporary closing and restricted capacities of establishments serving alcohol (bars, pubs, and restaurants), males may have consumed less alcohol due to limited access. In addition, social cues may have limited alcohol consumption in the home. Although liquor store sales increased during the pandemic, it is plausible overall consumption by men decreased due to limited access to previously visited establishments.
Recent studies mirror these findings. Deutsch-Link et al[13] reviewed the Centers for Disease Control and Prevention data, and discovered that mortality from ALD rose from 2017 to 2020 in the United States, with females and younger adults having the highest relative increase. Gonzalez et al[14] documented an increase in the proportion of female ALD admissions during the pandemic, in their study of 337 patients in the Detroit area. They also found an increase in Black/African American admissions. Sohal et al[15] also reported an increase in alcohol-related hepatitis requiring inpatient management, especially in patients under the age of 40 and in women during the pandemic with 329 patients studied in three community hospitals in Fresno, California, United States.
The strength of the current study lies in its longitudinal population-based evaluation of temporal trends for ALD in a large multi-hospital system, reviewing 1378 admissions for ALD. Limitations of the current study include its retrospective design and limited geographical reach. This study definitely underestimates the prevalence of ALD during the COVID-19 era, as only patients with significant ALD would have been admitted. Patient hesitancy to present to hospitals during the pandemic, as well as cessation of elective admissions may have also contributed to underestimating the prevalence of ALD during the pandemic. Further studies are indicated to determine whether these increasing trends of ALD hospitalizations persist, particularly in younger women, and to evaluate the psychosocial factors impacting alcohol consumption during the COVID-19 pandemic.
This large multi-hospital analysis demonstrates a concerning gender disparity with women, especially young women, being significantly more likely to be admitted with ALD during the COVID-19 period compared to the twelve months prior to the pandemic. Intensive public health interventions, especially those focused towards women, may help to curb the rising rates of alcoholic liver disease in the United States.
Alcoholic liver disease (ALD) has traditionally been a disease of middle-aged and older men, though recent studies indicate an increasing prevalence of women with ALD.
The coronavirus disease 2019 (COVID-19) pandemic has had widespread consequences affecting many socially and economically. This appears to have resulted in increased alcohol consumption in many individuals.
To assess the trends for ALD admissions during the COVID-19 pandemic and compare it to a similar pre-pandemic period.
This was a retrospective analysis of hospitalizations for ALD in a large multi-center hospital system in the United States from April 2019 to March 2021.
An increase in admissions for ALD in women was noted (33% rise in women< 50 years and 22% rise in women > 50 years). Though ALD admissions for men < 50 years rose 24%, a fall of 24% in those > 50 years was noted.
This study found a significant increase in younger women requiring hospital admission for ALD.
It is of significant medical interest to gastroenterologists and hepatologists to determine whether the trend of increased ALD hospitalizations in women persist in future years.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: American College of Gastroenterology; American Society for Gastrointestinal Endoscopy; American Gastroenterological Association; American Association for the Study of Liver Diseases.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ferrarese A, Italy; Yao SK, China S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Basra S, Anand BS. Definition, epidemiology and magnitude of alcoholic hepatitis. World J Hepatol. 2011;3:108-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (3)] |
| 2. | Chrostek L, Jelski W, Szmitkowski M, Puchalski Z. Gender-related differences in hepatic activity of alcohol dehydrogenase isoenzymes and aldehyde dehydrogenase in humans. J Clin Lab Anal. 2003;17:93-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Shirazi F, Singal AK, Wong RJ. Alcohol-associated Cirrhosis and Alcoholic Hepatitis Hospitalization Trends in the United States. J Clin Gastroenterol. 2021;55:174-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 4. | National Institute on Alcohol Abuse and Alcoholism. As Male and Female Drinking Patterns Become More Similar, Adverse Alcohol Risks for Women Become More Apparent. National Institute on Alcohol Abuse and Alcoholism. September 9, 2021. [cited August 2, 2022]. Available from: https://niaaa.scienceblog.com/378/as-male-and-female-drinking-patterns-become-more-similar-adverse-alcohol-risks-for-women-become-more-apparent. |
| 5. | Noguchi Y. Sharp, 'Off The Charts' Rise In Alcoholic Liver Disease Among Young Women. March 16, 2021. [cited August 2, 2022]. Available from: https://www.npr.org/sections/health-shots/2021/03/16/973684753/sharp-off-the-charts-rise-in-alcoholic-liver-disease-among-young-women. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Lee BP, Dodge JL, Leventhal A, Terrault NA. Retail Alcohol and Tobacco Sales During COVID-19. Ann Intern Med. 2021;174:1027-1029. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 76] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 7. | Dubey MJ, Ghosh R, Chatterjee S, Biswas P, Dubey S. COVID-19 and addiction. Diabetes Metab Syndr. 2020;14:817-823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 228] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 8. | Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci. 2015;40:219-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 752] [Cited by in RCA: 1000] [Article Influence: 100.0] [Reference Citation Analysis (0)] |
| 9. | Devoto A, Himelein-Wachowiak M, Liu T, Curtis B. Women's Substance Use and Mental Health During the COVID-19 Pandemic. Womens Health Issues. 2022;32:235-240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Williams E, Mulia N, Karriker-Jaffe KJ, Lui CK. Changing Racial/Ethnic Disparities in Heavy Drinking Trajectories Through Young Adulthood: A Comparative Cohort Study. Alcohol Clin Exp Res. 2018;42:135-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Bertha M, Shedden K, Mellinger J. Trends in the inpatient burden of alcohol-related liver disease among women hospitalized in the United States. Liver Int. 2022;42:1557-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 12. | Davies EL, Cooke R, Maier LJ, Winstock AR, Ferris JA. Where and What You Drink Is Linked to How Much You Drink: An Exploratory Survey of Alcohol Use in 17 Countries. Subst Use Misuse. 2021;56:1941-1950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Deutsch-Link S, Jiang Y, Peery AF, Barritt AS, Bataller R, Moon AM. Alcohol-Associated Liver Disease Mortality Increased From 2017 to 2020 and Accelerated During the COVID-19 Pandemic. Clin Gastroenterol Hepatol. 2022;20:2142-2144.e2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 54] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 14. | Gonzalez HC, Zhou Y, Nimri FM, Rupp LB, Trudeau S, Gordon SC. Alcohol-related hepatitis admissions increased 50% in the first months of the COVID-19 pandemic in the USA. Liver Int. 2022;42:762-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 15. | Sohal A, Khalid S, Green V, Gulati A, Roytman M. The Pandemic Within the Pandemic: Unprecedented Rise in Alcohol-related Hepatitis During the COVID-19 Pandemic. J Clin Gastroenterol. 2022;56:e171-e175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 35] [Article Influence: 11.7] [Reference Citation Analysis (0)] |