Published online Jun 27, 2022. doi: 10.4254/wjh.v14.i6.1226
Peer-review started: January 10, 2022
First decision: March 8, 2022
Revised: March 24, 2022
Accepted: May 14, 2022
Article in press: May 14, 2022
Published online: June 27, 2022
Processing time: 164 Days and 11.8 Hours
Type 2 diabetes mellitus (T2DM) is a risk factor for nonalcoholic fatty liver disease (NAFLD).
To determine the prevalence and clinical correlates of NAFLD in a large cohort of patients with T2DM.
Four hundred thirty-seven participants with T2DM who consulted at Meijo Hospital from April 2019 to September 2020 and underwent computed tomo
NAFLD was identified in 25.2% of the participants. Young age (odds ratio [OR] = −0.945; 95% confidence interval [CI]: 0.922–0.969), higher hemoglobin levels (OR = 1.501, 95%CI: 1.278–1.764), lower high-density lipoprotein (HDL) cholesterol levels (OR = 0.971, 95%CI: 0.953–0.989), and the absence of dialysis (OR = 0.109, 95%CI: 0.014–0.856) were independent predictors of NAFLD.
NAFLD was detected with CT in 25.2% of the participants. NAFLD was associated with younger age, higher hemoglobin levels, lower HDL cholesterol levels, and an absence of dialysis.
Core Tip: Type 2 diabetes mellitus (T2DM) is a risk factor for nonalcoholic fatty liver disease (NAFLD). The prevalence of NAFLD by computed tomography (CT) has been reported in a few studies. The clinical correlates of NAFLD are often ambiguous. We determined the prevalence and clinical correlates of NAFLD determined by CT in a large cohort of patients with T2DM. The prevalence of NAFLD by CT was 25.2%. NAFLD was associated with younger age, higher hemoglobin levels, lower HDL cholesterol levels, and an absence of dialysis.
- Citation: Yamane R, Yoshioka K, Hayashi K, Shimizu Y, Ito Y, Matsushita K, Yoshizaki M, Kajikawa G, Mizutani T, Watarai A, Tachi K, Goto H. Prevalence of nonalcoholic fatty liver disease and its association with age in patients with type 2 diabetes mellitus. World J Hepatol 2022; 14(6): 1226-1234
- URL: https://www.wjgnet.com/1948-5182/full/v14/i6/1226.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i6.1226
Nonalcoholic fatty liver disease (NAFLD) frequently coexists with type 2 diabetes mellitus (T2DM). Both synergistically increase adverse outcomes[1,2]. NAFLD, T2DM, and obesity are epidemiologically correlated, but their causal interrelationships remain incompletely understood. Liu et al[3] proposed the hypothesis of disease subphenotyping in which genetically-driven NAFLD promotes T2DM and central obesity but protects against overall obesity. In contrast, genetically-driven T2DM and obesity increase the NAFLD risk.
A meta-analysis showed that the prevalence of NAFLD in patients with T2DM was 56% with ultrasonography (US) and proton magnetic resonance spectroscopy (MRI)[4]. The prevalence of NAFLD in patients with T2DM was highest in Europe (68%), but varies widely depending on the population. Three studies from Japan using US reported that the prevalence of NAFLD was 31%, 69%, and 61%[5-7]. The sensitivity of diagnosing NAFLD varies with the method. The prevalence of NAFLD in patients with T2DM detected by computed tomography (CT) was 10% in the United States[8], 22% in Turkey[9], and 27% in Japan[10].
In patients with T2DM, NAFLD is associated with an increased risk of overall death[11] but not with liver-related deaths[8]. Meanwhile, in NAFLD patients, T2DM is associated with advanced liver fibrosis[12] and increased mortality related to liver-related deaths[13]. NAFLD in patients with T2DM is associated with an increased risk of cardiovascular disease[7,9,10,14]. However, some reports have denied this association[8,15-17]. A positive association between NAFLD and nephropathy in patients with T2DM has been reported in some studies[18,19], while others did not find an association[20-22]. The association of NAFLD with cardiovascular risk and chronic kidney disease in the general population was reported to start in childhood[23,24].
We studied the prevalence of NAFLD in patients with T2DM in our hospital using CT and determined the factors associated with NAFLD in patients with T2DM.
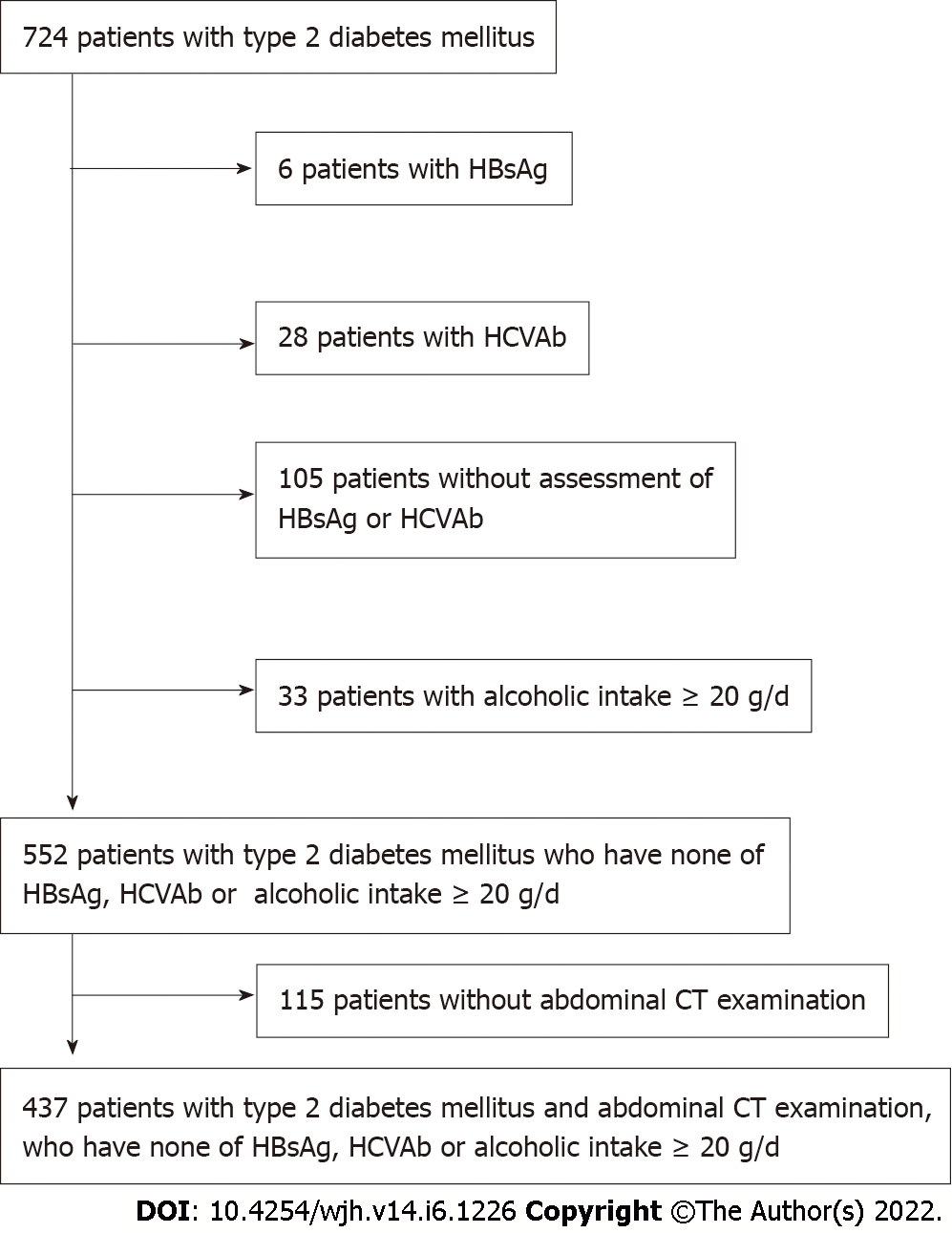
Data of patients with T2DM were retrieved from the hospital database. There were 724 Japanese diabetic patients who consulted at the Federation of National Public Service Personnel Mutual Aid Associations Meijo Hospital from April 2019 to September 2020. We excluded participants who had chronic hepatitis B (n = 6) and C (n = 28) infections, no assessment of hepatitis B surface antigen and hepatitis C virus antibody (n = 105), and an alcohol intake ≥ 20 g/d (n = 33). We also excluded 115 participants who did not have an abdominal CT examination; thus, 437 participants (269 men and 168 women) were included in the analysis (Figure 1). The mean age was 74 ± 13 years. There were 322 patients treated with oral hypoglycemic agents, 32 with insulin, one with a glucagon-like peptide-1 receptor agonist, and 82 with diet and exercise. All patients had more than a year with T2DM.
The study was conducted according to the Declaration of Helsinki and approved by the Ethics Committee of Federation of National Public Service Personnel Mutual Aid Associations Meijo Hospital (Approval No. 166). Written informed consent was waived because the data were analyzed anonymously based on information stored in the hospital database.
A non-enhanced CT was performed using either a 16-section multidetector scanner (Aquilion 16; Canon Medical Systems, Tochigi, Japan), a 64-section multidetector scanner (Aquilion 64; Canon Medical Systems, Tochigi, Japan), or an 80-section multidetector scanner (Aquilion Prime SP/iEdition; Canon Medical Systems, Tochigi, Japan). The CT indications were to screen for diseases in the chest and abdomen in 430 patients. The CT was performed to investigate liver diseases in seven patients. Nine and three regions of interest were positioned at the liver or spleen, respectively, to avoid macroscopic vessels. Median hepatic or splenic attenuation values were obtained. Hepatic attenuation minus splenic attenuation (CTL−S) less than 1 Hounsfield unit was considered fatty liver[25].
Student's t-test was used to analyze differences in continuous variables between two groups. Categorical variables were compared with the Chi-squared or Fisher's exact test. Linear regression was performed to assess the relationship between two variables. Multiple logistic regression was performed to determine the independent factors associated with the presence of NAFLD. P values < 0.05 were considered significant. All analyses were performed with StatFlex version 6.0 for Windows (StatFlex, Osaka, Japan).
Fatty liver was detected in 110 of 437 patients (25.2%). It was significantly associated with male gender (P = 0.005), younger age (P < 0.001), greater height (P < 0.001) and weight (P < 0.001), higher body mass index (BMI) (P < 0.001), blood parameters [higher white blood cell counts (P = 0.021) and higher hemoglobin (P < 0.001)], altered liver function tests [higher albumin (P < 0.001), higher total bilirubin (P = 0.015), aspartate aminotransferase (P = 0.014), alanine aminotransferase (P < 0.001), and gamma glutamyl transpeptidase (P < 0.001)], kidney function [lower creatinine (P = 0.012) and higher estimated glomerular filtration rate (eGFR) (P = 0.004)], metabolic status [higher total cholesterol (P = 0.012), lower high density lipoprotein (HDL) cholesterol (P = 0.039), higher triglycerides (P < 0.001), and higher low density lipoprotein (LDL) cholesterol (P = 0.001)], a lower fibrosis-4 (FIB-4) index (P = 0.005), and non-hypertensive (P = 0.013) and non-dialysis patients (P = 0.003) (Table 1). Fatty liver also tended to be associated with higher HbA1c (P = 0.066).
| Variables | ALL (n = 437) | Fatty liver (n = 110) | Non-fatty liver (n = 327) | P value |
| Gender (Male/Female) | 269/168 | 80/30 | 189/138 | 0.005 |
| Age (yr) | 74.0 ± 13.0 | 64.7 ± 13.0 | 77.1 ± 11.0 | < 0.001 |
| Height (cm) | 159.4 ± 10.2 | 163.2 ± 10.0 | 158.2 ± 9.9 | < 0.001 |
| Body weight (kg) | 61.3 ± 14.5 | 70.0 ± 16.6 | 58.5 ± 12.5 | < 0.001 |
| BMI (kg/m2) | 24.0 ± 4.9 | 26.0 ± 4.7 | 23.3 ± 4.7 | < 0.001 |
| HbA1c (%) | 7.0 ± 1.2 | 7.2 ± 1.2 | 6.9 ± 1.2 | 0.066 |
| Blood glucose (mg/dl) | 164 ± 80 | 170 ± 116 | 161 ± 63 | 0.297 |
| White blood cells (/μL) | 6618 ± 2299 | 7056 ± 1649 | 6470 ± 2463 | 0.021 |
| Hemoglobin (g/dL) | 12.6 ± 2.4 | 14.2 ± 2.1 | 12.0 ± 2.2 | < 0.001 |
| Platelets (104/μL) | 20.7 ± 7.0 | 20.4 ± 5.5 | 20.8 ± 7.4 | 0.615 |
| Prothrombin time (%) | 89.6 ± 22.3 | 89.2 ± 23.6 | 89.7 ± 22.1 | 0.895 |
| Albumin (g/dL) | 3.7 ± 0.7 | 3.9 ± 0.6 | 3.6 ± 0.6 | < 0.001 |
| Total bilirubin (mg/dL) | 0.76 ± 0.50 | 0.86 ± 0.49 | 0.72 ± 0.49 | 0.015 |
| ALP (U/L) | 266 ± 156 | 247 ± 80 | 272 ± 176 | 0.182 |
| AST (U/L) | 25.3 ± 22.8 | 29.0 ± 20.2 | 23.0 ± 23.4 | 0.014 |
| ALT (U/L) | 23.5 ± 20.8 | 35.0 ± 27.4 | 19.0 ± 16.1 | < 0.001 |
| GGT (U/L) | 46.2 ± 63.1 | 68.0 ± 74.4 | 38.0 ± 56.6 | < 0.001 |
| Creatinine (mg/dL) | 1.71 ± 2.10 | 1.27 ± 1.58 | 1.85 ± 2.22 | 0.012 |
| eGFR (mL/min) | 52.0 ± 29.2 | 58.9 ± 21.9 | 49.6 ± 30.9 | 0.004 |
| Total cholesterol (mg/dL) | 181 ± 50 | 193 ± 64 | 177 ± 43 | 0.012 |
| HDL cholesterol (mg/dL) | 53 ± 17 | 50 ± 15 | 54 ± 17 | 0.039 |
| Triglyceride (mg/dL) | 160 ± 179 | 228 ± 299 | 134 ± 87 | < 0.001 |
| LDL cholesterol (mg/dL) | 101 ± 36 | 111 ± 40 | 96 ± 33 | 0.001 |
| FIB-4 index | 2.20 ± 1.56 | 1.84 ± 1.08 | 2.32 ± 1.67 | 0.005 |
| Cirrhosis (%) | 8 (1.8) | 1 (0.9) | 7 (2.1) | 0.405 |
| Hepatocellular carcinoma (%) | 7 (1.6) | 1 (0.9) | 6 (1.8) | 0.504 |
| Cerebrovascular accident (%) | 45 (10) | 9 (8.2) | 36 (11) | 0.399 |
| Cardiovasculart disease (%) | 137 (31) | 29 (26) | 108 (33) | 0.193 |
| Dyslipidemia (%) | 205 (47) | 53 (48) | 152 (46) | 0.758 |
| Hypertension (%) | 270 (62) | 57 (51) | 213 (65) | 0.013 |
| Dialysis (%) | 45 (10) | 3 (2.7) | 42 (12) | 0.003 |
Multivariate logistic regression was used to elucidate the independent factors associated with fatty liver. Gender, age, BMI, HbA1c, white blood cell count, hemoglobin, albumin, eGFR, total cholesterol, HDL cholesterol, triglyceride, LDL cholesterol, hypertension, and dialysis therapy were analyzed. Age (P < 0.001), hemoglobin level (P < 0.001), HDL cholesterol level (P = 0.002), and absence of dialysis (P = 0.035) were independent factors associated with fatty liver (Table 2).
| Variables | Odds ratio | 95% confidence interval | P value |
| Age | 0.945 | 0.922-0.969 | < 0.001 |
| Hemoglobin | 1.501 | 1.278-1.764 | < 0.001 |
| HDL cholesterol | 0.971 | 0.953-0.989 | 0.002 |
| Dialysis | 0.109 | 0.014-0.856 | 0.035 |
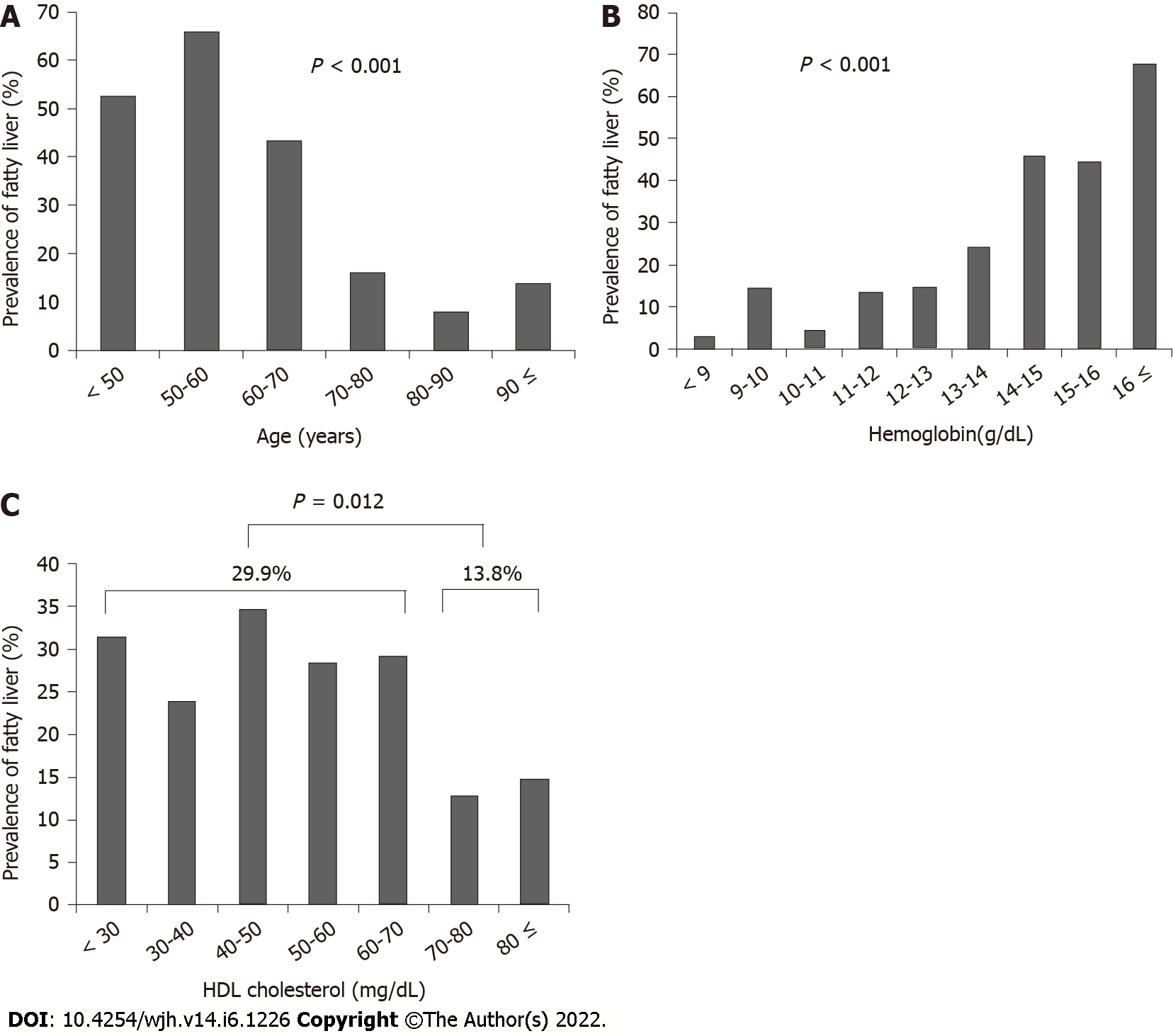
The patients were stratified according to age, hemoglobin level, and HDL cholesterol level, and the association with fatty liver was assessed. The prevalence of fatty liver significantly decreased with increasing age (P < 0.001) (Figure 2A), significantly increased as hemoglobin levels increased (P < 0.001) (Figure 2B), and was significantly higher in patients with HDL cholesterol < 70 mg/dL (29.9%) than patients with HDL cholesterol ≥ 70 mg/dL (13.8%) (P = 0.012) (Figure 2C).
The prevalence of NAFLD in patients with T2DM detected by CT was 25.2%. NAFLD was associated with younger age, higher hemoglobin levels, lower HDL cholesterol levels, and the absence of dialysis.
A previous meta-analysis found that the prevalence of NAFLD in patients with T2DM was 56% with US or proton magnetic resonance spectroscopy[4]. The prevalence of NAFLD in patients with T2DM detected by CT was 10% in the United States[8], 22% in Turkey[9], and 27% in Japan[10]. Lee et al[26] reported that the sensitivity of US (92%) for detecting more than 30% hepatic steatosis was higher than CT (64%). The prevalence of NAFLD in this study is comparable to the reported prevalence in patients with T2DM diagnosed by CT in Japan. In a preliminary study of 179 subjects who attended health screening in our hospital (120 males and 59 females; 53.7 ± 10.8 years), CT detected fatty liver in 40 (22%). Thus, the prevalence of NAFLD in T2DM is higher than in the general population considering older age.
The prevalence of NAFLD significantly decreased with increasing age in this study. In contrast, Targher et al[14] reported that the prevalence of NAFLD detected by US in patients with T2DM increased with age; 65% among patients aged 40 to 59 and 75% among those aged 60 and older. The difference in this study compared to Targher's regarding the association of NAFLD and age may be attributed to the difference in the mean age of the participants (74 vs 64 years, respectively). By combining Targher's results and this study, it is suggested that the prevalence of NAFLD increases with age until about 60 years (as in Targher's study) and then decreases with age, as shown in this study. An "inverted U curve," in which the prevalence of NAFLD reaches a peak in late adulthood and decreases afterward has been reported in the general population[27-29]. However, a meta-analysis observed a consistent increase in the NAFLD prevalence across all age groups[30].
Poor nutritional status is more common in older people[31]. Age-related changes in appetite, health problems, and social problems predispose older adults to less food intake. Poor nutritional status in older people is also common in patients with T2DM[32]. The decreasing prevalence of NAFLD with age shown in the present study may be attributed to poor nutritional status. Age significantly negatively correlated with BMI in this study (r = −0.32, P < 0.001, data not shown). A high BMI is associated with NAFLD[28] and a low BMI is associated with poor nutritional status[33]. BMI was associated with NAFLD in this study by univariate analysis but not by multivariate analysis.
In this study, lower hemoglobin values were associated with a lower prevalence of NAFLD. Anemia is common in the elderly and an indicator of poor nutritional status[34]. Therefore, the lower prevalence of NAFLD in patients with lower hemoglobin values may be attributed to the poor nutritional status of these patients. Hemoglobin values also significantly positively correlated with BMI (r = 0.21, P < 0.001, data not shown).
Higher HDL cholesterol values were associated with a lower prevalence of NAFLD. This association between HDL cholesterol and NAFLD has previously been reported[28].
Dialysis treatment was associated with a lower prevalence of NAFLD. Diabetic nephropathy affects approximately 25% of patients with T2DM and is the leading cause of renal failure. Two studies reported that NAFLD is inversely associated with nephropathy in patients with T2DM, similar to this study[20,21]; however, some studies have reported a positive or no association[18,19,22]. The difference in the studied populations may cause this discrepancy. When the study population was not limited to patients with T2DM, a meta-analysis showed a positive association between NAFLD and chronic kidney disease[35]. However, in patients with T2DM, this association is still ambiguous.
This study did not find an association between NAFLD and cardiovascular disease. This association has been previously reported[7,9,10,14]; however, other studies deny it[8,15-17]. Higher HDL cholesterol values associated with a lower prevalence of NAFLD in this study reduce the risk of cardiovascular disease[36]. Thus a follow-up study may reveal an association between NAFLD and cardiovascular disease.
In this study, the number of patients with cirrhosis or hepatocellular carcinoma (HCC) was small, and cirrhosis and HCC were not associated with NAFLD. In a follow-up study of patients with T2DM (mean, 10.9 years), Adams et al[11] reported that 5 of 116 patients with NAFLD and none of 221 patients without NAFLD died from liver-related causes. Dunn et al[8] reported that NAFLD was not associated with liver-related outcomes (transplant, HCC, or encephalopathy) in patients with T2DM in a five-year retrospective cohort study. Further studies are needed to assess these associations.
There are three limitations to this study. First, it is a cross-sectional study. There may be a question of whether NAFLD decreases with age. Poor nutritional status in older people may be one reason why NAFLD decreases with age. It is also possible that we assessed a certain subpopulation of T2DM with a low risk of NAFLD and survival until older age, while the patients with a high risk of NAFLD dropped out until older age because of complications. Thus, the temporal association of NAFLD with the factors assessed in this study has to be clarified by prospective cohort studies. Second, fatty liver was diagnosed by CT in this study. The sensitivity of MRI, US, and CT for detecting a fatty liver of 5% or higher is 77%-80%, 53%-62%, and 50% compared with liver biopsy[37]. However, a liver biopsy is invasive and has a risk of severe complications. Thus noninvasive modalities, such as US, CT, and MRI, have been commonly used to detect fatty liver. MRI is expensive and scarce. The disadvantage of US is its subjective nature. The high liver iron content increases CT Hounsfield units and may obliterate the diagnosis of fatty liver. However, CT is widely available in Japan, and the diagnosis is objective. Thus, CT is a promising modality for diagnosing fatty liver. Third, the present study was performed in a single hospital. The prevalence found has to be reevaluated in multicenter studies.
The prevalence of NAFLD in patients with T2DM detected by CT was 25.2%. NAFLD was associated with age, hemoglobin level, HDL cholesterol level, and the absence of dialysis treatment.
Type 2 diabetes mellitus (T2DM) is an established risk factor for the development of nonalcoholic fatty liver disease (NAFLD). Both synergistically increase adverse outcomes.
The prevalence of NAFLD assessed by computed tomography (CT) was reported only in a few studies. The clinical correlates of NAFLD are often ambiguous.
To determine the prevalence and clinical correlates of NAFLD assessed by CT in a large cohort of T2DM patients.
Four hundred thirty-seven participants with T2DM who consulted at Meijo Hospital from April 2019 to September 2020 and underwent CT were assessed.
The prevalence of NAFLD as detected by CT was 25.2% in T2DM patients, and NAFLD was associated with a younger age, higher hemoglobin levels, lower high density lipoprotein cholesterol levels, and absence of dialysis treatment.
The prevalence of NAFLD in T2DM is higher than in the general population considering older age and decreases with age.
The association of NAFLD with age has to be clarified by prospective cohort studies.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Di Sessa A, Italy; Ulasoglu C, Turkey; Zhang LL, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Hazlehurst JM, Woods C, Marjot T, Cobbold JF, Tomlinson JW. Non-alcoholic fatty liver disease and diabetes. Metabolism. 2016;65:1096-1108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 308] [Cited by in RCA: 380] [Article Influence: 42.2] [Reference Citation Analysis (0)] |
| 2. | Shima T, Uto H, Ueki K, Takamura T, Kohgo Y, Kawata S, Yasui K, Park H, Nakamura N, Nakatou T, Tanaka N, Umemura A, Mizuno M, Tanaka J, Okanoue T. Clinicopathological features of liver injury in patients with type 2 diabetes mellitus and comparative study of histologically proven nonalcoholic fatty liver diseases with or without type 2 diabetes mellitus. J Gastroenterol. 2013;48:515-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Liu Z, Zhang Y, Graham S, Wang X, Cai D, Huang M, Pique-Regi R, Dong XC, Chen YE, Willer C, Liu W. Causal relationships between NAFLD, T2D and obesity have implications for disease subphenotyping. J Hepatol. 2020;73:263-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 169] [Article Influence: 33.8] [Reference Citation Analysis (1)] |
| 4. | Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, Qiu Y, Burns L, Afendy A, Nader F. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol. 2019;71:793-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 773] [Cited by in RCA: 1494] [Article Influence: 249.0] [Reference Citation Analysis (0)] |
| 5. | Fukuda K, Seki Y, Ichihi M, Okada T, Hirata A, Kogita S, Sawai Y, Igura T, Tsugawa M, Imai Y. Usefulness of ultrasonographic estimation of preperitoneal and subcutaneous fat thickness in the diagnosis of nonalcoholic fatty liver disease in diabetic patients. J Med Ultrason (2001). 2015;42:357-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Miyasato M, Murase-Mishiba Y, Bessho M, Miyawaki M, Imbe H, Tsutsumi C, Tanimoto K, Imagawa A, Terasaki J, Hanafusa T. The cytokeratin-18 fragment level as a biomarker of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus. Clin Chim Acta. 2014;433:184-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Takeuchi Y, Ito H, Komatsu Y, Oshikiri K, Antoku S, Abe M, Mifune M, Togane M. Non-alcoholic fatty liver disease is an independent predictor for macroangiopathy in Japanese type 2 diabetic patients: a cross-sectional study. Intern Med. 2012;51:1667-1675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Dunn MA, Behari J, Rogal SS, O'Connell MR, Furlan A, Aghayev A, Gumus S, Saul MI, Bae KT. Hepatic steatosis in diabetic patients does not predict adverse liver-related or cardiovascular outcomes. Liver Int. 2013;33:1575-1582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Idilman IS, Akata D, Hazirolan T, Doganay Erdogan B, Aytemir K, Karcaaltincaba M. Nonalcoholic fatty liver disease is associated with significant coronary artery disease in type 2 diabetic patients: a computed tomography angiography study 2:. J Diabetes. 2015;7:279-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Ichikawa K, Miyoshi T, Osawa K, Miki T, Toda H, Ejiri K, Yoshida M, Nanba Y, Nakamura K, Morita H, Ito H. Prognostic value of non-alcoholic fatty liver disease for predicting cardiovascular events in patients with diabetes mellitus with suspected coronary artery disease: a prospective cohort study. Cardiovasc Diabetol. 2021;20:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 11. | Adams LA, Harmsen S, St Sauver JL, Charatcharoenwitthaya P, Enders FB, Therneau T, Angulo P. Nonalcoholic fatty liver disease increases risk of death among patients with diabetes: a community-based cohort study. Am J Gastroenterol. 2010;105:1567-1573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 224] [Cited by in RCA: 207] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 12. | Hossain N, Afendy A, Stepanova M, Nader F, Srishord M, Rafiq N, Goodman Z, Younossi Z. Independent predictors of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7:1224-1229, 1229.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 247] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 13. | Younossi ZM, Gramlich T, Matteoni CA, Boparai N, McCullough AJ. Nonalcoholic fatty liver disease in patients with type 2 diabetes. Clin Gastroenterol Hepatol. 2004;2:262-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 287] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 14. | Targher G, Bertolini L, Padovani R, Rodella S, Tessari R, Zenari L, Day C, Arcaro G. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;30:1212-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 702] [Cited by in RCA: 700] [Article Influence: 38.9] [Reference Citation Analysis (1)] |
| 15. | Cakır E, Ozbek M, Colak N, Cakal E, Delıbaşi T. Is NAFLD an independent risk factor for increased IMT in T2DM? Minerva Endocrinol. 2012;37:187-193. [PubMed] |
| 16. | Coracina A, Gaiani S, Cosma A, Pellizzari P, Pizzi C, de Kreutzenberg S, Cecchet D, Sacerdoti D, Tessari P. No association between the degree of liver steatosis and early signs of vasculopathy in T2DM. Nutr Metab Cardiovasc Dis. 2012;22:e11-e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Petit JM, Guiu B, Terriat B, Loffroy R, Robin I, Petit V, Bouillet B, Brindisi MC, Duvillard L, Hillon P, Cercueil JP, Verges B. Nonalcoholic fatty liver is not associated with carotid intima-media thickness in type 2 diabetic patients. J Clin Endocrinol Metab. 2009;94:4103-4106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 18. | Casoinic F, Sâmpelean D, Bădău C, Prună L. Nonalcoholic fatty liver disease--a risk factor for microalbuminuria in type 2 diabetic patients. Rom J Intern Med. 2009;47:55-59. [PubMed] |
| 19. | Targher G, Bertolini L, Rodella S, Zoppini G, Lippi G, Day C, Muggeo M. Non-alcoholic fatty liver disease is independently associated with an increased prevalence of chronic kidney disease and proliferative/laser-treated retinopathy in type 2 diabetic patients. Diabetologia. 2008;51:444-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 275] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 20. | Kim BY, Jung CH, Mok JO, Kang SK, Kim CH. Prevalences of diabetic retinopathy and nephropathy are lower in Korean type 2 diabetic patients with non-alcoholic fatty liver disease. J Diabetes Investig. 2014;5:170-175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 21. | Lv WS, Sun RX, Gao YY, Wen JP, Pan RF, Li L, Wang J, Xian YX, Cao CX, Zheng M. Nonalcoholic fatty liver disease and microvascular complications in type 2 diabetes. World J Gastroenterol. 2013;19:3134-3142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 22. | Zhan YT, Zhang C, Li L, Bi CS, Song X, Zhang ST. Non-alcoholic fatty liver disease is not related to the incidence of diabetic nephropathy in Type 2 Diabetes. Int J Mol Sci. 2012;13:14698-14706. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Di Sessa A, Umano GR, Miraglia Del Giudice E. The Association between Non-Alcoholic Fatty Liver Disease and Cardiovascular Risk in Children. Children (Basel). 2017;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Di Sessa A, Guarino S, Melone R, De Simone RF, Marzuillo P, Miraglia Del Giudice E. Relationship between nonalcoholic fatty liver disease and chronic kidney disease could start in childhood. World J Gastroenterol. 2021;27:5793-5795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Park YS, Park SH, Lee SS, Kim DY, Shin YM, Lee W, Lee SG, Yu ES. Biopsy-proven nonsteatotic liver in adults: estimation of reference range for difference in attenuation between the liver and the spleen at nonenhanced CT. Radiology. 2011;258:760-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 26. | Lee JY, Kim KM, Lee SG, Yu E, Lim YS, Lee HC, Chung YH, Lee YS, Suh DJ. Prevalence and risk factors of non-alcoholic fatty liver disease in potential living liver donors in Korea: a review of 589 consecutive liver biopsies in a single center. J Hepatol. 2007;47:239-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 185] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 27. | Alqahtani SA, Schattenberg JM. NAFLD in the Elderly. Clin Interv Aging. 2021;16:1633-1649. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 70] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 28. | Eguchi Y, Hyogo H, Ono M, Mizuta T, Ono N, Fujimoto K, Chayama K, Saibara T; JSG-NAFLD. Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: a multicenter large retrospective study. J Gastroenterol. 2012;47:586-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 401] [Article Influence: 30.8] [Reference Citation Analysis (2)] |
| 29. | Golabi P, Paik J, Reddy R, Bugianesi E, Trimble G, Younossi ZM. Prevalence and long-term outcomes of non-alcoholic fatty liver disease among elderly individuals from the United States. BMC Gastroenterol. 2019;19:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 82] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 30. | Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5322] [Cited by in RCA: 7533] [Article Influence: 837.0] [Reference Citation Analysis (0)] |
| 31. | Volkert D. Malnutrition in older adults - urgent need for action: a plea for improving the nutritional situation of older adults. Gerontology. 2013;59:328-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 32. | Tamura Y, Omura T, Toyoshima K, Araki A. Nutrition Management in Older Adults with Diabetes: A Review on the Importance of Shifting Prevention Strategies from Metabolic Syndrome to Frailty. Nutrients. 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 125] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 33. | Maeda K, Ishida Y, Nonogaki T, Mori N. Reference body mass index values and the prevalence of malnutrition according to the Global Leadership Initiative on Malnutrition criteria. Clin Nutr. 2020;39:180-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 124] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 34. | Mitrache C, Passweg JR, Libura J, Petrikkos L, Seiler WO, Gratwohl A, Stähelin HB, Tichelli A. Anemia: an indicator for malnutrition in the elderly. Ann Hematol. 2001;80:295-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 82] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 35. | Musso G, Gambino R, Tabibian JH, Ekstedt M, Kechagias S, Hamaguchi M, Hultcrantz R, Hagström H, Yoon SK, Charatcharoenwitthaya P, George J, Barrera F, Hafliðadóttir S, Björnsson ES, Armstrong MJ, Hopkins LJ, Gao X, Francque S, Verrijken A, Yilmaz Y, Lindor KD, Charlton M, Haring R, Lerch MM, Rettig R, Völzke H, Ryu S, Li G, Wong LL, Machado M, Cortez-Pinto H, Yasui K, Cassader M. Association of non-alcoholic fatty liver disease with chronic kidney disease: a systematic review and meta-analysis. PLoS Med. 2014;11:e1001680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 545] [Cited by in RCA: 524] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 36. | Arca M, Montali A, Valiante S, Campagna F, Pigna G, Paoletti V, Antonini R, Barillà F, Tanzilli G, Vestri A, Gaudio C. Usefulness of atherogenic dyslipidemia for predicting cardiovascular risk in patients with angiographically defined coronary artery disease. Am J Cardiol. 2007;100:1511-1516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 37. | Lee SS, Park SH, Kim HJ, Kim SY, Kim MY, Kim DY, Suh DJ, Kim KM, Bae MH, Lee JY, Lee SG, Yu ES. Non-invasive assessment of hepatic steatosis: prospective comparison of the accuracy of imaging examinations. J Hepatol. 2010;52:579-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 288] [Article Influence: 19.2] [Reference Citation Analysis (2)] |