Published online Jun 27, 2022. doi: 10.4254/wjh.v14.i6.1150
Peer-review started: January 31, 2022
First decision: March 25, 2022
Revised: April 1, 2022
Accepted: June 3, 2022
Article in press: June 3, 2022
Published online: June 27, 2022
Processing time: 143 Days and 0.4 Hours
Patients who undergo living donor liver transplantation (LDLT) may suffer complications that require intensive care unit (ICU) readmission.
To identify the incidence, causes, and outcomes of ICU readmission after LDLT.
A retrospective cohort study was conducted on patients who underwent LDLT. The collected data included patient demographics, preoperative characteristics, intraoperative details; postoperative stay, complications, causes of ICU readmis
The present study included 299 patients. Thirty-one (10.4%) patients were readmitted to the ICU after discharge. Patients who were readmitted to the ICU were older in age (53.0 ± 5.1 vs 49.4 ± 8.8, P = 0.001) and had a significantly higher percentage of women (29% vs 13.4%, P = 0.032), diabetics (41.9% vs 24.6%, P = 0.039), hypertensives (22.6% vs 6.3%, P = 0.006), and renal (6.5% vs 0%, P = 0.010) patients as well as a significantly longer initial ICU stay (6 vs 4 d, respectively, P < 0.001). Logistic regression analysis revealed that significant independent risk factors for ICU readmission included recipient age (OR = 1.048, 95%CI = 1.005-1.094, P = 0.030) and length of initial hospital stay (OR = 0.836, 95%CI = 0.789-0.885, P < 0.001).
The identification of high-risk patients (older age and shorter initial hospital stay) before ICU discharge may help provide optimal care and tailor follow-up to reduce the rate of ICU readmission.
Core Tip: Patients undergoing living donor liver transplantation may suffer complications that require intensive care unit readmission. We retrospectively evaluated 299 patients who underwent living donor liver transplantation. We identified the incidence, causes, and outcomes of intensive care unit readmission after living donor liver transplantation. Older recipient age and longer length of initial hospital stay were recognized as significant independent risk factors for intensive care unit readmission. The identification of high-risk patients before discharge may help provide optimal care and tailor follow-up to reduce the rate of intensive care unit readmission.
- Citation: Salah M, Montasser IF, El Gendy HA, Korraa AA, Elewa GM, Dabbous H, Mahfouz HR, Abdelrahman M, Goda MH, Bahaa El-Din MM, El-Meteini M, Labib HA. Intensive care unit readmission in adult Egyptian patients undergoing living donor liver transplant: A single-centre retrospective cohort study. World J Hepatol 2022; 14(6): 1150-1161
- URL: https://www.wjgnet.com/1948-5182/full/v14/i6/1150.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i6.1150
Liver transplantation is the only definitive treatment for end-stage liver disease[1]. As a major abdominal surgery, postoperative complications may occur and might require readmission, which may be serious and life threatening. In general, patients who require intensive care unit (ICU) readmission show higher morbidity, mortality, and prolonged hospital stays than those who do not require readmission[2-5].
Complications following living donor liver transplantation (LDLT) requiring ICU readmission may be serious and life threatening. Identification of the causes of ICU readmission is pivotal to establish effective strategies to reduce the rate of readmission, improve the quality of care and patient outcomes, and reduce health expenditures by medical institutions[6].
Most available reports are on hospital readmission after deceased donor liver transplantation (DDLT). To our knowledge, there are limited published data about hospital readmission of LDLT patients. We hypothesized that ICU readmission after LDLT is due to different reasons. Consequently, this study was conducted to identify the incidence, causes, and outcomes of ICU readmission after LDLT.
This retrospective cohort study was conducted by reviewing the hospital files of adult patients who underwent LDLT at Ain Shams University Hospital, Cairo, Egypt, during the period from January 1, 2008, to December 31, 2018.
This study was approved by the Ethics Committee of the Faculty of Medicine, Ain Shams University, Egypt (approval number: IRB/0006379). The confidentiality of the patients’ data was maintained by assigning a code number to each patient.
We included adult Egyptian patients (18 years old or above) of either sex who underwent LDLT at our institution during the period from January 1, 2008, to December 31, 2018.
The following patients were excluded from the study: We excluded patients who were less than 18 years old, who died before discharge after LDLT, who underwent retransplantation before discharge from the ICU after the first liver transplant, and who were pregnant patients.
The sample size was calculated using Epi InfoTM software (Centers for Disease Control and Prevention, version 7.2.3.0), setting the type-1 error (α) at 0.05, an acceptable margin of error of 5%, and a 95% confidence interval. The results from a previous study[5] showed that the incidence of hospital readmission among cases undergoing liver transplantation was 17.1%. Calculation according to these values produced a minimal sample size of 218 cases.
The hospital files of patients who met the eligibility criteria were thoroughly revised to extract relevant data. The collected data included patient demographics, donor characteristics, preoperative and intraoperative variables, postoperative stay, complications, causes for ICU readmission, and outcomes after ICU readmission.
The studied primary outcome was the incidence of ICU readmission. Readmission was defined as ICU readmission within ≤ 3 mo of initial ICU discharge. Patients were divided into two groups: those who were readmitted to the ICU (the readmission group) and those who were not (the control group). The secondary outcomes included the causes of first hospital readmission after discharge as well as the incidence of ICU readmission for more than one time and two-year survival.
Risk factors for ICU readmission were assessed by examining the contribution of collected patient and donor variables to the probability of ICU readmission.
Statistical analysis was performed using the Statistical Package for Social Sciences (IBM SPSS Statistics) for Windows, version 26 (IBM Corp., Armonk, NY, United States). For quantitative data, the Shapiro-Wilk test for normality was performed. For data that followed a normal distribution, values were expressed as the mean ± SD. Comparisons between two groups were carried out using an independent samples T test. For data that did not follow a normal distribution, the median and interquartile range (IQR; expressed as the 25th-75th percentiles) were calculated, and the Mann–Whitney test was used to compare the two groups. For qualitative data, the variables were summarized as frequencies. Pearson’s chi square tests for independence, Fisher’s exact test or Fisher-Freeman-Halton exact test were used to examine the association between two categorical variables as appropriate. Binomial logistic regression was conducted to identify independent risk factors for ICU readmission, including all variables with a P value < 0.1 in univariant analysis. Kaplan–Meier curves and log rank tests were performed to estimate two-year survival. A P value < 0.05 was adopted to interpret the significance of statistical tests.
The statistical review of this study was performed by a biomedical statistician.
The present study included 299 patients who underwent liver transplantation and were followed up for a median duration of 40 mo (ranging from less than one month to 136 mo) after surgery. Thirty-one (10.4%) patients were readmitted into the ICU within ≤ 3 mo of initial ICU discharge, among whom 7 (2.3% of total cases) had more than one ICU readmission. Hospital readmission was recorded in 10 (3.3%), among whom 5 (1.6% of total cases) were readmitted due to biliary complications and sepsis. Table 1 depicts the causes for ICU readmission.
| N | % | |
| Sepsis | 5 | 1.6 |
| Pulmonary complications | 3 | 0.9 |
| Cardiovascular complications | 3 | 0.9 |
| HA thrombosis | 3 | 0.9 |
| 7Th day syndrome | 1 | 0.3 |
| Acute cellular rejection | 1 | 0.3 |
| Acute Pancreatitis | 1 | 0.3 |
| Cerebrovascular stroke | 3 | 0.9 |
| Graft failure | 1 | 0.3 |
| hemorrhagic shock | 1 | 0.3 |
| Liver infarction | 1 | 0.3 |
| Metabolic disorders | 1 | 0.3 |
| Portal vein thrombosis | 1 | 0.3 |
| Prograf neurotoxicity | 2 | 0.6 |
| PV STENOSIS | 1 | 0.3 |
| Re -transplant1 | 2 | 0.6 |
| Renal impairment | 1 | 0.3 |
The preoperative characteristics of the studied patients and donors are shown in Table 2. The mean age of the patients was 49.8 ± 8.6 years. Men outnumbered women (84.9% vs 15.1%, respectively). The mean BMI was 28.4 ± 4.3 kgm2. The median MELD score was 16 (ranging from 6 to 29). Approximately one-third of the patients had one or more comorbidities; the most frequent were diabetes mellitus (26.4%), hypertension (8%), and IHD (1.3%). The most frequent liver disease was HCV (76.6%), followed by HCC (39.1%), PVT (12.4%), and cryptogenic (10.7%). Encephalopathy was diagnosed in 31.8% of patients. Regarding the donors, the mean age was 29.8 ± 6.3 years (ranging from 18 to 48), with a higher percentage of men than women (68.6% vs 31.4%, respectively); their mean BMI was 23.7 ± 2.6 kgm2. The comparison between patients who were readmitted to the ICU and patients who were not readmitted showed that the former group was older in age (53.0 ± 5.1 vs 49.4 ± 8.8, P = 0.001) and had a significantly higher percentage of women (29% vs 13.4%, P = 0.032), diabetic patients (41.9% vs 24.6%, P = 0.039), hypertensive patients (22.6% vs 6.3%, P = 0.006), and renal patients (6.5% vs 0%, P = 0.010).
| Total (N = 299), % | No ICU readmission (N = 268), % | ICU readmission (N = 31), % | Test statistic | P value | |||||
| Age (years); mean ± SD (Range) | 49.8 ± 8.6; (19.0 - 67.0) | 49.4 ± 8.8; (19.0 - 67.0) | 53.0 ± 5.1; (42.0 - 64.0) | 3.381a | 0.0011 | ||||
| Gender | Female | 45 | 15.1 | 36 | 13.4 | 9 | 29.0 | FE | 0.0321 |
| Male | 254 | 84.9 | 232 | 86.6 | 22 | 71.0 | |||
| BMI (Kg/m2); mean ± SD (Range) | 28.4 ± 4.3; (18.5 - 52.9) | 28.2 ± 4.0; (18.5 - 42.0) | 29.4 ± 6.5; (20.6 - 52.9) | 0.936a | 0.356 | ||||
| MELD score; Median [IQR] (Range) | 16.0; [13.0 – 18.0] (6.0 - 29.0) | 16.0; [13.0 -18.0] (6.0 - 29.0) | 15.0; [12.0 – 20.0] (7.0 - 28.0) | 0.538b | 0.590 | ||||
| Positive medical history | 103 | 34.4 | 86 | 32.1 | 17 | 54.8 | FE | 1.000 | |
| DM | 79 | 26.4 | 66 | 24.6 | 13 | 41.9 | 4.282c | 0.0391 | |
| Hypertension | 24 | 8.0 | 17 | 6.3 | 7 | 22.6 | FE | 0.0061 | |
| Bronchial asthma | 3 | 1.0 | 2 | 0.7 | 1 | 3.2 | FE | 0.281 | |
| IHD | 4 | 1.3 | 4 | 1.5 | 0 | 0.0 | FE | 1.000 | |
| Renal | 2 | 0.7 | 0 | 0.0 | 2 | 6.5 | FE | 0.0101 | |
| Bilharziasis | 2 | 0.7 | 2 | 0.7 | 0 | 0.0 | FE | 1.000 | |
| Others | 9 | 3.0 | 8 | 3.0 | 1 | 3.2 | FE | 1.000 | |
| Diagnosis | AIH | 10 | 3.3 | 10 | 3.7 | 0 | 0.0 | FE | 0.606 |
| HCC | 117 | 39.1 | 107 | 39.9 | 10 | 32.3 | 0.686c | 0.408 | |
| PVT | 37 | 12.4 | 34 | 12.7 | 3 | 9.7 | FE | 0.780 | |
| Cryptogenic | 32 | 10.7 | 29 | 10.8 | 3 | 9.7 | FE | 1.000 | |
| ESLD | 10 | 3.3 | 8 | 3.0 | 2 | 6.5 | FE | 0.278 | |
| HCV | 229 | 76.6 | 204 | 76.1 | 25 | 80.6 | 0.317c | 0.573 | |
| HBV | 11 | 3.7 | 11 | 4.1 | 0 | 0.0 | FE | 0.612 | |
| BCS | 2 | 0.7 | 2 | 0.7 | 0 | 0.0 | FE | 1.000 | |
| PSC | 2 | 0.7 | 2 | 0.7 | 0 | 0.0 | FE | 1.000 | |
| Encephalopathy | 95 | 31.8 | 87 | 32.5 | 8 | 25.8 | 0.568c | 0.451 | |
| Creatinine clearance (mL/min); mean ± SD (Range) | 88.7 ± 26.5; (10.0 - 172.0) | 88.5 ± 25.8; (10.0 - 170.0) | 90.4 ± 32.7; (16.0 - 172.0) | 0.384a | 0.702 | ||||
| Serum creatinine (mg/dL); mean ± SD (Range) | 0.97 ± 0.31; (0.30 - 2.40) | 0.97 ± 0.32; (0.30 - 2.40) | 0.96 ± 0.24; (0.50 - 1.30) | 0.255a | 0.799 | ||||
| Serum Albumin gm/dL; mean ± SD (Range) | 3.0 ± 0.5; (1.8 - 4.8) | 3.0 ± 0.5; (1.8 - 4.8) | 2.8 ± 0.5; (1.8 - 3.8) | 1.428a | 0.154 | ||||
| Na mmol/L; mean ± SD (Range) | 135.1 ± 5.2; (117.0 - 147.0) | 135.1 ± 5.4; (117.0 - 147.0) | 135.0 ± 3.6; (128.0 - 145.0) | 0.137a | 0.891 | ||||
| Total bilirubin mg/dL; Median [IQR] (Range) | 1.3; [0.8 - 1.9] (0.2 - 27.0) | 1.3; [0.7 - 1.9] (0.2 - 27.0) | 1.4; [1.1 - 1.9] (0.6 - 5.6) | 1.270b | 0.204 | ||||
| Alkaline phosphatase IU/L; Median [IQR] (Range) | 143.0; [97.0 - 221.0] (6.2 - 2369.0) | 144.5; [97.0 - 231.5] (6.2 - 2369.0) | 131.0; [98.0 - 167.0] (45.0 - 1410.0) | 1.041b | 0.298 | ||||
| Donor age (years); mean ± SD (Range) | 29.8 ± 6.3; (16.0 - 48.0) | 30.0 ± 6.3; (16.0 - 48.0) | 28.0 ± 5.9; (18.0 - 39.0) | 1.731a | 0.084 | ||||
| Donor gender | Female | 94 | 31.4 | 83 | 31.0% | 11 | 35.5 | 0.263c | 0.608 |
| Male | 205 | 68.6 | 185 | 69.0% | 20 | 64.5 | |||
| Donor BMI (Kg/m2); mean ± SD (Range) | 23.7 ± 2.6; (17.7 - 32.0) | 23.8 ± 2.6; (17.7 - 32.0) | 23.0 ± 2.3; (18.3 - 29.0) | 1.545a | 0.124 | ||||
Table 3 summarizes the intraoperative and postoperative details of the studied patients. Synthetic grafts were used in 2.7% of patients. Vascular surgical complications were encountered in 15.7% of patients, mainly in the form of hepatic artery thrombosis (8%). No significant difference was detected between the two groups (P > 0.05).
| Total (N = 299), % | No ICU readmission (N = 268), % | ICU readmission (N = 31), % | Test statistic | P value | |||||
| Waiting Time (days); Median [IQR] (Range) | 86.0; [59.0 - 120.0] (20.0 - 546.0) | 86.5; [56.5 - 120.0] (20.0 - 462.0) | 74.0; [65.0 - 119.0] (29.0 - 546.0) | 0.034a | 0.973 | ||||
| Warm ischemia time (min); mean ± SD (Range) | 48.6 ± 19.4; (20.0 - 145.0) | 48.7 ± 19.0; (20.0 - 145.0) | 47.9 ± 22.7; (20.0 - 145.0) | 0.222b | 0.274 | ||||
| Graft weight/GRWR; mean ± SD (Range) | 1.06 ± 0.47; (0.01 - 6.30) | 1.08 ± 0.49; (0.01 - 6.30) | 0.98 ± 0.23; (0.01 - 1.30) | 1.095b | 0.825 | ||||
| Cold ischemia time (min); Median [IQR] (Range) | 45.0; [30.0 - 60.0] (10.0 - 180.0) | 45.0; [31.0 - 60.0] (10.0 - 180.0) | 45.0; [30.0 - 50.0] (20.0 - 125.0) | 0.864a | 0.387 | ||||
| Packed red blood cells (units); Median [IQR] (Range) | 4.0; [2.0 - 7.0] (1.0 - 28.0) | 4.0; [2.0 - 7.0] (1.0 - 28.0) | 3.0; [2.0 - 6.0] (1.0 - 17.0) | 0.957a | 0.339 | ||||
| PV Anastomosis | RPV/MPV | 255 | 85.3 | 230 | 85.8 | 25 | 80.6 | FE | 0.426 |
| RPV/CPV | 34 | 11.4 | 29 | 10.8 | 5 | 16.1 | FE | 0.372 | |
| RPV/RPV | 4 | 1.3 | 4 | 1.5 | 0 | 0.0 | FE | 1.000 | |
| LPV/LPV | 1 | 0.3 | 1 | 0.4 | 0 | 0.0 | |||
| LPV/MPV | 2 | 0.7 | 2 | 0.7 | 0 | 0.0 | |||
| RPH/CHV | 2 | 0.7 | 2 | 0.7 | 0 | 0.0 | |||
| RPV/CBV | 1 | 0.3 | 0 | 0.0 | 1 | 3.2 | |||
| RPV/CHV | 1 | 0.3 | 1 | 0.4 | 0 | 0.0 | |||
| HA Anastomosis | RHA/RHA | 280 | 93.6 | 252 | 94.0 | 28 | 90.3 | FE | 0.708 |
| RHA/LHA | 18 | 6.0 | 15 | 5.6 | 3 | 9.7 | FE | 0.606 | |
| RHA/SPA | 1 | 0.3 | 1 | 0.4 | 0 | 0.0 | |||
| HVs Anastomosis | RHV/RHV | 278 | 93.0 | 248 | 92.5 | 30 | 96.8 | FE | 0.708 |
| RHV/IVC | 10 | 3.3 | 10 | 3.7 | 0 | 0.0 | FE | 0.606 | |
| LMHV/LMHV | 9 | 3.0 | 8 | 3.0 | 1 | 3.2 | FE | 1.000 | |
| RHV/MHV | 2 | 0.7 | 2 | 0.7 | 0 | 0.0 | |||
| Synthetic graft | 8 | 2.7 | 7 | 2.6 | 1 | 3.2 | FE | 0.588 | |
| Surgical vascular complications | 47 | 15.7 | 39 | 14.6 | 8 | 25.8 | FE | 0.118 | |
| HA stenosis | 6 | 2.0 | 5 | 1.9 | 1 | 3.2 | |||
| HA thrombosis | 24 | 8.0 | 19 | 7.1 | 5 | 16.1 | |||
| HV stenosis | 3 | 1.0 | 3 | 1.1 | 0 | 0.0 | |||
| HVT | 2 | 0.6 | 2 | 0.8 | 0 | 0.0 | |||
| PV stenosis | 4 | 1.3 | 3 | 1.1 | 1 | 3.2 | |||
| PV thrombosis | 7 | 2.3 | 6 | 2.2 | 1 | 3.2 | |||
| Sub-diaphragmatic hematoma | 1 | 0.3 | 1 | 0.4 | 0 | 0.0 | |||
Table 4 shows the follow-up details of the patients. The median LOS of initial ICU admission was significantly longer in the readmission group (6 vs 4 d, respectively, P < 0.001). Rejection occurred in 12% of all patients. The mortality rate was 29.8%, with a significantly higher percentage in the readmission group (64.5% vs 25.7%, P < 0.001).
| Total (N = 299) | No ICU readmission (N = 268) | ICU readmission (N = 31) | Test statistic | P value | ||||
| Initial Hospital length of stay (days); Median [IQR] (Range) | 21.0; [18.0 - 26.0](1.0 - 150.0) | 22.0; [19.0 - 26.0] (5.0 - 120.0) | 3.0; [2.0 - 9.0] (1.0 - 150.0) | 8.003a | < 0.0011 | |||
| Length of stay in initial ICU (days); Median [IQR] (Range) | 4.0; [3.0 - 5.0] (2.0 - 45.0) | 4.0; [3.0 - 5.0] (2.0 - 45.0) | 6.0; [5.0 - 7.0] (4.0 - 9.0) | 6.676a | < 0.0011 | |||
| Rejection (N, %) | 36 | 12.0 | 34 | 12.7 | 2 | 6.5 | FE | 0.557 |
| Mortality(N, %) | 89 | 29.8 | 69 | 25.7 | 20 | 64.5 | 19.978b | < 0.0011 |
Logistic regression analysis was conducted to identify risk factors for ICU readmission after discharge (Table 5). Significant independent risk factors included recipient age and length of initial hospital stay after discharge from the ICU. The increase in recipient age by one year was associated with an increased likelihood of ICU readmission by 4.8% (OR = 1.048, 95%CI = 1.005-1.094, P = 0.030). A negative relationship existed between the length of initial hospital stay and the probability of ICU readmission, as an increased length of stay resulted in a decreased risk of readmission (OR = 0.836, 95%CI = 0.789-0.885, P < 0.001).
| Wald | P value | OR | 95%CI for OR | ||
| Lower | Upper | ||||
| Patients’ age (years) | 4.707 | 0.0301 | 1.048 | 1.005 | 1.094 |
| Gender (male compared to female) | 2.722 | 0.099 | 0.399 | 0.134 | 1.188 |
| DM | 1.257 | 0.262 | 1.828 | 0.637 | 5.244 |
| Hypertension | 0.462 | 0.497 | 1.641 | 0.394 | 6.842 |
| Donors’ age (years) | 1.700 | 0.192 | 0.954 | 0.888 | 1.024 |
| Length of initial ICU stay (days) | 1.255 | 0.263 | 1.055 | 0.960 | 1.159 |
| Length of initial hospital stay (days) | 37.306 | < 0.0011 | 0.836 | 0.789 | 0.885 |
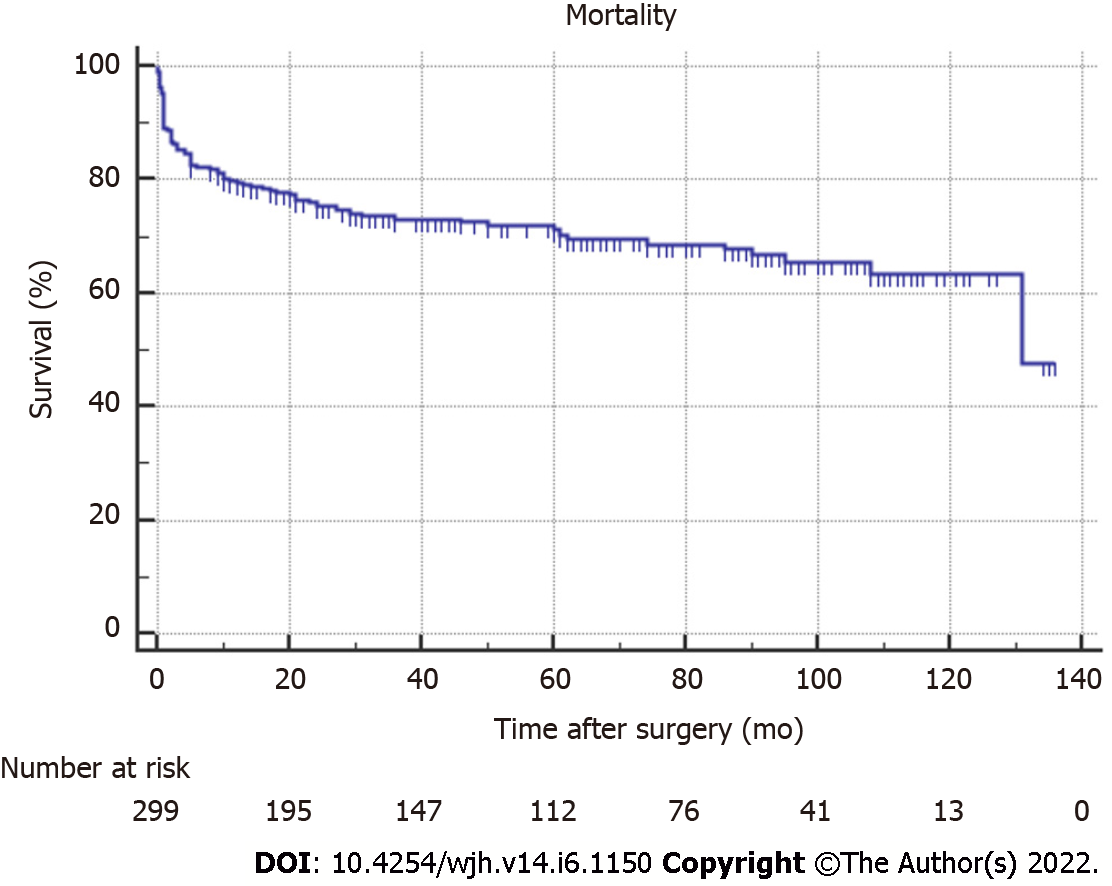
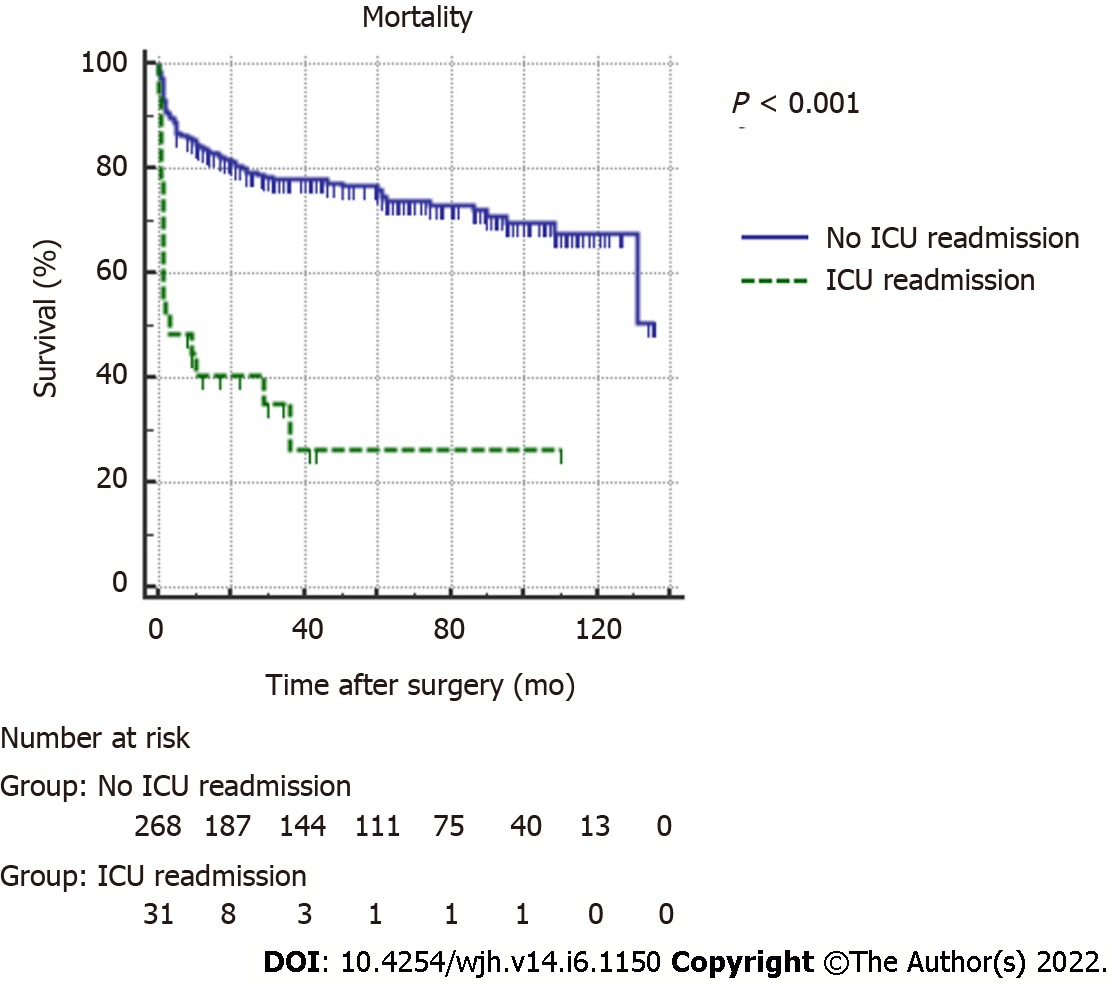
Figures 1 and 2 illustrate the survival curve for all studied patients and according to ICU readmission, respectively. The OS rates for all patients at 1 and 2 years were 79.5% ± 2.3% and 75.2% ± 2.5%, respectively. The overall survival (OS) rates for non-ICU readmitted patients were 83.9% ± 2.3% and 79.2% ± 2.5% at 1 and 2 years, respectively. For ICU readmitted patients, the OS rate was 40.6% ± 9.1% at 1 year and persisted until 2 years. The log rank test showed a significant difference between the survival curves of the two groups (P < 0.001).
Readmission after discharge from the hospital is considered among the important indicators of the quality of delivered health care services. Moreover, readmissions impose an additional considerable burden on health care expenditure and on hospital resources[7]. Recipients of liver transplantation are susceptible to the administration of multiple drug regimens, and they endure metabolic changes in addition to the complications that may arise from surgery[5]. All of these factors increase the risk of hospital and ICU readmission in this group of patients[8,9]. The current study aimed to identify the incidence, causes, and outcomes of ICU readmission after LDLT. Our cohort consisted of 299 patients who underwent LDLT and were followed up for a median duration of 40 mo.
In the present study, the incidence of ICU readmission within the first 3 mo after discharge was 10.4% and that of multiple ICU readmissions was 2.3% of the total cases. The incidence of hospital readmission after discharge was 3.3%. In agreement with this low rate of readmission, Chen et al[5] reported a 3-mo hospital readmission rate of 9.4% in 791 patients who underwent either LDLT or DDLT. On the other hand, much higher incidence rates of hospital readmission were reported by earlier studies[6,8-10].
Shankar et al[9] assessed risk factors for rehospitalization in 208 patients who underwent liver transplantation (among whom 8 patients only underwent LDLT) over a duration of 4 years. They reported a hospital readmission rate of 30.3% within 3 mo. Pereira et al[8] conducted an assessment of 766 patients undergoing DDLT over an 8-year period. They found a 30-d readmission rate of 45%. Patel et al[10] evaluated 325 patients with DDLT over a 10-year period, with an overall 90-d readmission rate of 46%. Yataco et al[6] studied hospital readmission in 445 patients who underwent either DDLT or LDLT, with a 90-d hospital readmission rate of 42%. All of these studies included patients who underwent either DDLT only or a mixed sample of DDLT and LDLT. Nagaraja et al[11] assessed 140 LDLT patients and found the rate of readmission within 3 mo after discharge to be lower than reported in DDLT or a mixed sample (27.1%).
The wide variation in the reported readmission rates among studies may be explained by the difference in preoperative patient characteristics, as only 16.7% of studies included patients undergoing LDLT and had MELD scores above 19. In addition, institutional policies for patient selection before transplant and the criteria for readmission differ among the centres, potentially impacting the reported rates of readmission.
The most common causes of ICU readmission among our patients included sepsis (5/31 patients), followed by pulmonary and cardiac causes (3/31 each). Previous studies reported sepsis as the most common cause for hospital readmission, followed by biliary complications[6,11]. Meanwhile, sepsis due to biliary complications were reported among the causes for hospital readmission (1.6% of total cases) in our cohort.
We proceeded in the current study to identify potential risk factors that increase the likelihood of ICU readmission within 3 mo after discharge. Several variables were assessed in the literature as potential predictors of rehospitalization after liver transplantation.
The recipient’s age was found on univariate and multivariate analyses in the current study to be significantly associated with an increased probability of ICU readmission. This association is supported by the results of Levy et al[12] and Patel et al[10]. However, several studies showed a lack of significant association with rehospitalization[5,6,8,9,11].
Regarding the recipient’s sex, univariate analysis showed that women were significantly more likely to be readmitted to the ICU, but this association was not significant in multivariate analysis. Patel et al[10] reported a lower risk for men and an increased risk for women. Other previous studies reported the lack of a significant effect of recipient sex on rehospitalization[5,6,8,9,11,12].
The presence of comorbidities was assessed in the present study. A higher percentage of ICU readmission was associated with diabetes, hypertension, and renal disease in univariate analysis, while multivariate analysis showed the lack of a significant effect on ICU readmission. The increased risk of rehospitalization with the presence of chronic illnesses was stated in the literature in patients undergoing surgery[13,14]. Our results are in line with previous studies assessing rehospitalization after liver transplantation, which did not show this significant association[5,8,11]. On the other hand, other preoperative morbid conditions, such as preoperative HCV infection[9] and PVT[8], were reported to increase the risk of hospital readmission, although such an association was not detected in our cohort.
While the current study results revealed a significantly longer initial ICU stay in ICU readmitted patients using univariate analysis, the association was not found to be significant on multivariate analysis. Similarly, Nagaraja et al[11] and Yataco et al[6] reported the lack of a significant difference between readmitted and non readmitted groups. In contrast, Levy et al[12] found that a higher percentage of non readmitted patients had an ICU stay less than 3 d than readmitted patients (67.8% vs 56.3%, P = 0.0231). Shankar et al[9] reported that a longer LOS in the ICU had a lower risk ratio.
Numerous other factors were identified by some researchers as predictors of rehospitalization but were nonsignificant in the current study, including the MELD score and postoperative complications.
We found that the initial hospital stay correlated negatively with the probability of ICU readmission (OR = 0.836, 95%CI = 0.789-0.885, P < 0.001), indicating an increased risk with shorter stays. The literature shows controversial reports concerning the relationship between the length of initial hospital stay and rehospitalization. A negative correlation was also observed by Kassin et al[13], Ladner et al[15], Pereira et al[8], and Chen et al[5]. Contradictory results were stated by Yataco et al[6], who found that an initial hospital stay longer than 7 d was significantly associated with hospital readmission. Prolonged hospital stay can potentially exert two contradictory effects on the probability of hospital readmission, which may depend largely on the range of stay. On the one hand, a longer stay can prevent discharge before full assessment, optimization of the patient, and adequate management of postoperative complications. Some postoperative complications, such as rejection, may not manifest within the first days after transplantation, and their detection after discharge leads to early hospital readmission. On the other hand, prolonged stay predisposes the patient to an increased risk of contracting nosocomial infection with a negative impact on the patient’s health and outcomes.
A higher MELD score has been associated with higher health care costs and increased utilization of hospital resources[16,17]. Nevertheless, the MELD score was not found to be significantly associated with ICU readmission in this study, a finding shared by several previous studies assessing risk factors for hospital readmission[5,6,8-11]. The calculation of the MELD score is based on a limited set of laboratory measurements that are not able to capture all aspects of the patient’s functional status.
We did not find a significant difference in the rate of postoperative complications between readmitted and nonreadmitted groups, a finding shared by Nagaraja et al[11]. However, Chen et al[5] found that the risk of readmission correlated positively with the number and severity of complications after liver transplantation. An increased risk in patients suffering postoperative complications was also observed by Pereira et al[8].
The mortality rate in our series was 29.8%. The OS rates for all patients at 1 and 2 years were 79.5% ± 2.3% and 75.2% ± 2.5%, respectively. Patients with ICU readmission had a significantly higher mortality rate than those without readmission (64.5% vs 25.7%, P < 0.001). The OS rates for ICU readmitted patients were significantly reduced compared to the non readmission group at one year (40.6% ± 9.1% vs 83.9% ± 2.3%) and two years (40.6% ± 9.1% vs 79.2% ± 2.5%) post transplantation. This association between readmission and mortality could be explained by the worsened health status of readmitted patients, which requires readmission and at the same time increases the risk of mortality. Moreover, ICU readmission may expose the patient to nosocomial infections, and the use of multiple medications may negatively affect renal function and result in further deterioration of the patient’s health status.
In accordance with these findings, Pereira et al[8] found decreased OS at one year after transp
The present study differs from previous studies by investigating ICU readmission and not all rehospitalizations, which may explain differences in results from those studies. We believe that ICU readmission imposes more negative effects on both patients and the resources of health care systems than rehospitalization into other hospital wards or units. Considering that the resources of the ICU are limited and the cost of care is higher than that encountered with hospital ward admission, the identification of specific causes and risk factors for ICU readmission is crucial. However, the present study bears some points of limitation. The retrospective nature of the study predisposes the collected data to inaccuracies. Moreover, patients may have been readmitted to other health care facilities, and such data may not be recorded in our institution’s files. Being a single-centre experience hinders the generalization of our results.
Older recipient age and shorter initial hospital stay were significantly associated with ICU readmission. The overall survival rate for ICU readmitted patients was significantly lower than that for non-ICU readmitted patients. The identification of high-risk patients with these factors before discharge may help provide optimal care and tailor follow-up to reduce the rate of ICU readmission.
Intensive care unit (ICU) admission and readmission following liver transplantation is important field in liver transplantation operation. Readmission causes and effect on prognosis in terms of morbidity and mortality are still needed to be further investigated
To identify causes and outcome in recipients post living donor liver transplantation (LDLT) who required ICU readmission after initial discharge from ICU and to compare them with patients who did not require readmission
A retrospective cohort study carried on recipients who had LDLT in single Egyptian center in the period betwenn 2008 and 2018. Patients were divided into two groups according to ICU readmission after initial hospital discharge. Risk factors for ICU readmission were identified in univariate and multivariate analyses.
Retrospective cohort study was conducted by reviewing the hospital files and records of adult patients who underwent LDLT at Ain Shams University Hospital, Cairo, Egypt, during the period from January 1, 2008, to December 31, 2018. Causes and outcome of ICU readmission were compared between both groups (Readmission group and non readmission group). Risk factors for ICU readmission were also assessed including donor and recipient factors. Binomial logistic regression was conducted to identify independent risk factors for ICU readmission, including all variables with a P value < 0.1 in univariant analysis.
Thirty-one (10.4%) patients were readmitted into the ICU within ≤ 3 mo of initial ICU discharge, among whom 7 (2.3% of total cases) had more than one ICU readmission. Biliary complication and sepsis was the most common cause of ICU readmission. Significant independent risk factors included recipient age and length of initial hospital stay after discharge from the ICU.
The study concluded that older recipient age and duration of hospital stay (word stay) before ICU readmission were significant risk factors for ICU readmission. The overall survival rate for ICU readmitted patients was significantly lower than that for non-ICU readmitted patients.
Further study are warranted to identity how to improve management of the risky patients and hence improve their survival.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cimen SG, Turkey; Deshwal H, United States; Kumar R, India A-Editor: Zhu JQ, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Farkas S, Hackl C, Schlitt HJ. Overview of the indications and contraindications for liver transplantation. Cold Spring HarbPerspect Med. 2014;4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Rosenberg AL, Hofer TP, Hayward RA, Strachan C, Watts CM. Who bounces back? Crit Care Med. 2001;29:511-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 175] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 3. | Rosenberg AL, Watts C. Patients readmitted to ICUs* : a systematic review of risk factors and outcomes. Chest. 2000;118:492-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 273] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 4. | Chan KS, Tan CK, Fang CS, Tsai CL, Hou CC, Cheng KC, Lee MC. Readmission to the intensive care unit: an indicator that reflects the potential risks of morbidity and mortality of surgical patients in the intensive care unit. Surg Today. 2009;39:295-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Chen P, Wang W, Yan L, Yang J, Wen T, Li B, Zhao J, Xu M. Risk factors for first-year hospital readmission after liver transplantation. Eur J GastroenterolHepatol. 2015;27:600-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Yataco M, Cowell A, David W, Keaveny AP, Taner CB, Patel T. Predictors and impacts of hospital readmissions following liver transplantation. Ann Hepatol. 2016;15:356-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418-1428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3684] [Cited by in RCA: 3913] [Article Influence: 244.6] [Reference Citation Analysis (0)] |
| 8. | Pereira AA, Bhattacharya R, Carithers R, Reyes J, Perkins J. Clinical factors predicting readmission after orthotopic liver transplantation. Liver Transpl. 2012;18:1037-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Shankar N, Marotta P, Wall W, Albasheer M, Hernandez-Alejandro R, Chandok N. Defining readmission risk factors for liver transplantation recipients. GastroenterolHepatol (N Y). 2011;7:585-590. [PubMed] |
| 10. | Patel MS, Mohebali J, Shah JA, Markmann JF, Vagefi PA. Readmission following liver transplantation: an unwanted occurrence but an opportunity to act. HPB (Oxford). 2016;18:936-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Nagaraja R, Mehta N, Kumaran V, Varma V, Kapoor S, Nundy S. Readmission after living donor liver transplantation: predictors, causes, and outcomes. Indian J Gastroenterol. 2014;33:369-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Levy MF, Greene L, Ramsay MA, Jennings LW, Ramsay KJ, Meng J, Hein HA, Goldstein RM, Husberg BS, Gonwa TA, Klintmalm GB. Readmission to the intensive care unit after liver transplantation. Crit Care Med. 2001;29:18-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K, Sadiraj V, Sweeney JF. Risk factors for 30-day hospital readmission among general surgery patients. J Am CollSurg. 2012;215:322-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 479] [Article Influence: 36.8] [Reference Citation Analysis (0)] |
| 14. | Silverstein MD, Qin H, Mercer SQ, Fong J, Haydar Z. Risk factors for 30-day hospital readmission in patients ≥65 years of age. Proc (BaylUniv Med Cent). 2008;21:363-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 159] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 15. | Ladner DP, Skaro AI, Abecassis MM. Are all readmissions the same? Liver Transpl. 2012;18:1007-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Buchanan P, Dzebisashvili N, Lentine KL, Axelrod DA, Schnitzler MA, Salvalaggio PR. Liver transplantation cost in the model for end-stage liver disease era: looking beyond the transplant admission. Liver Transpl. 2009;15:1270-1277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 17. | Washburn WK, Pollock BH, Nichols L, Speeg KV, Halff G. Impact of recipient MELD score on resource utilization. Am J Transplant. 2006;6:2449-2454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 3.4] [Reference Citation Analysis (0)] |