Published online May 27, 2022. doi: 10.4254/wjh.v14.i5.992
Peer-review started: June 8, 2021
First decision: August 18, 2021
Revised: September 1, 2021
Accepted: April 24, 2022
Article in press: April 24, 2022
Published online: May 27, 2022
Processing time: 349 Days and 21 Hours
Studies have shown that covered self-expandable metallic stents (CSEMS) with a low axial forces after placement can cause early recurrent biliary obstruction (RBO) due to precipitating sludge formation.
To ascertain whether the angle of CSEMS after placement is a risk factor for RBO in unresectable distal malignant biliary obstruction (MBO).
Between January 2010 and March 2019, 261 consecutive patients underwent self-expandable metallic stent insertion by endoscopic retrograde cholangiopancreatography at our facility, and 87 patients were included in this study. We evaluated the risk factors for RBO, including the angle of CSEMS after placement as the primary outcome. We measured the obtuse angle of CSEMS after placement on an abdominal radiograph using the SYNAPSE PACS system. We also evaluated technical and functional success, adverse events, time to RBO (TRBO), non-RBO rate, survival time, cause of RBO, and reintervention procedure as secondary outcomes.
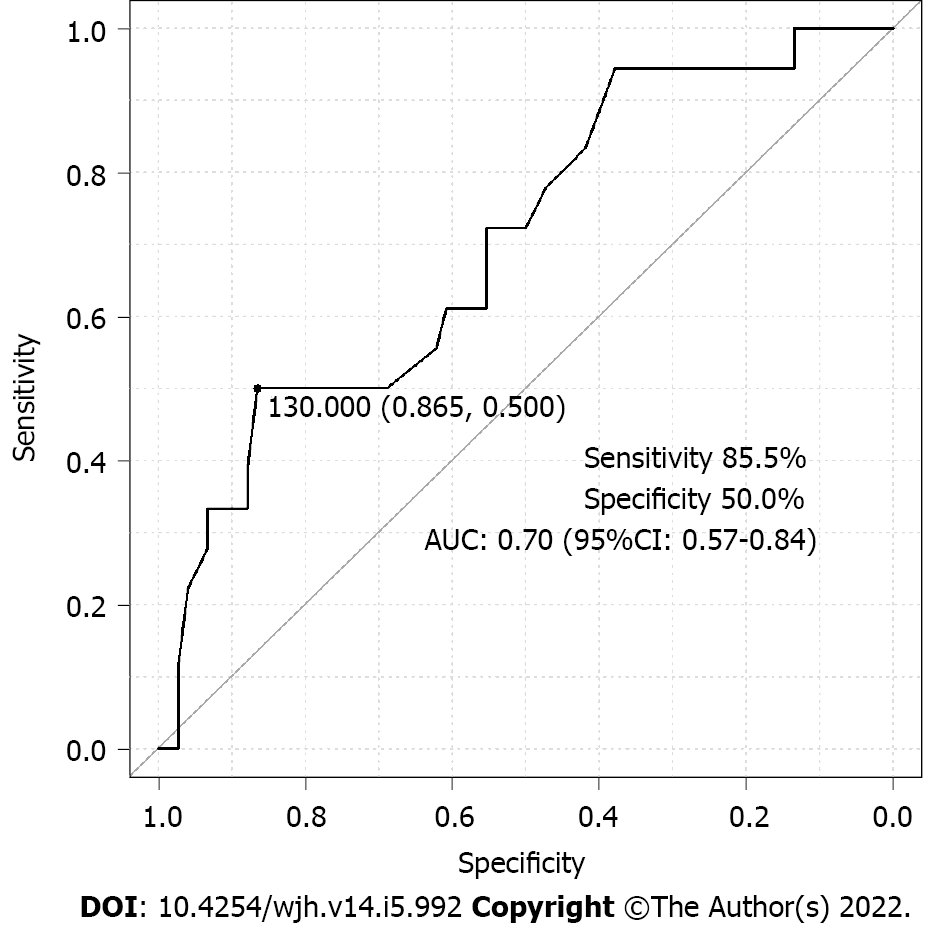
We divided the patients into two cohorts based on the presence or absence of RBO. The angle of CSEMS after placement (per 1° and per 10°) was evaluated using the multivariate Cox proportional hazard analysis, which was an independent risk factor for RBO in unresectable distal MBO [hazard ratio, 0.97 and 0.71; 95% confidence interval (CI): 0.94-0.99 and 0.54-0.92; P = 0.01 and 0.01, respectively]. For early diagnosis of RBO, the cut-off value of the angle of CSEMS after placement using the receiver operating characteristic curve was 130° [sensitivity, 50.0%; specificity 85.5%; area under the curve 0.70 (95%CI: 0.57-0.84)]. TRBO in the < 130° angle group was significantly shorter than that in the ≥ 130° angle group (P < 0.01).
This study suggests that the angle of the CSEMS after placement for unresectable distal MBO is a risk factor for RBO. These novel results provide pertinent information for future stent mana
Core Tip: We aimed to assess whether the angle of covered self-expandable metallic stents (CSEMS) after placement is a risk factor for recurrent biliary obstruction (RBO) in patients with unresectable distal malignant biliary obstruction. We included 87 patients in this study and divided them into two cohorts. We found that the angle of the CSEMS after placement was an independent risk factor for RBO. Furthermore, we demonstrated that the cut-off value of the angle of CSEMS after placement was 130° and that time to RBO in the < 130° group was significantly shorter than that in the ≥ 130° group.
- Citation: Tanoue K, Maruyama H, Ishikawa-Kakiya Y, Kinoshita Y, Hayashi K, Yamamura M, Ominami M, Nadatani Y, Fukunaga S, Otani K, Hosomi S, Tanaka F, Kamata N, Nagami Y, Taira K, Watanabe T, Fujiwara Y. Angle of covered self-expandable metallic stents after placement is a risk factor for recurrent biliary obstruction. World J Hepatol 2022; 14(5): 992-1005
- URL: https://www.wjgnet.com/1948-5182/full/v14/i5/992.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i5.992
Covered self-expandable metallic stents (SEMS) are widely used for managing unresectable distal malignant biliary obstruction (MBO)[1-4]. However, recurrent biliary obstruction (RBO), which constitutes a major problem in patients with MBO, prevents the continuation of treatment, and patients experience a poor quality of life. Covered self-expandable metallic stents (CSEMS) are expected to prolong patency in patients with unresectable distal MBO by preventing tumor ingrowth or epithelial hyperplasia[5,6]. Additionally, improving the conformability of SEMS in the bile duct reduces the risk of migration[6]. In a recent study, sludge formation and food impaction were identified as the major causes of RBO[7].
Recently, SEMS with low axial forces (AFs) have been used frequently to improve compatibility with the bile duct, with increasing concerns that they are likely to cause early RBO as a result of sludge formation and food impaction[8]. AF represents the stent-straightening force, and it has been shown that CSEMS with a high AF have a lower frequency of sludge formation and food impaction than those with a low AF[9].
Therefore, we hypothesized that the time to RBO (TRBO) in CSEMS with a low AF would be short. This study focused on the angle of the CSEMS after placement to investigate the risk factors for RBO due to CSEMS in unresectable distal MBO.
This retrospective cohort study was conducted at the Department of Gastroenterology, Osaka City University Graduate School of Medicine, Japan. Consecutive patients who underwent SEMS placement using endoscopic retrograde cholangiopancreatography (ERCP) between January 2010 and March 2019, with follow-up until September 2019, were enrolled. Next, patients who underwent CSEMS placement were included. The exclusion criteria were as follows: (1) Postoperative patients (Billroth II, Roux-en-Y reconstruction, etc.); (2) Patients with hilar biliary stricture; (3) Patients with placement of multiple SEMS; (4) Patients with benign distal biliary stricture; (5) Duplicated patients; (6) Patients with absence of abdominal radiograph; (7) Patients who had undergone percutaneous transhepatic biliary drainage, or biliary or duodenal metallic stenting; (8) Resectable distal MBO; (9) Patients with unknown treatment details; and (10) Early removal of SEMS due to cholecystitis and pancreatitis. Most cases could be pathologically evaluated, while other cases were diagnosed using radiographic imaging.
This study was conducted in compliance with the principles outlined in the Declaration of Helsinki. The study protocol was approved by the ethics committee of Osaka City University Graduate School of Medicine (No. 2020-022). All patients were given the opportunity to opt out of this study on our website’s homepage.
The primary outcome was risk factors for RBO in unresectable distal MBO, including assessment of the angle of the CSEMS after placement. The secondary outcomes included the evaluation of technical and functional success, adverse events, TRBO, non-RBO rate, survival time, cause of RBO, and reintervention procedure.
All procedures were performed using a side-viewing duodenoscope (JF240, JF260V, TJF240, TJF260V; Olympus Optical Co, Tokyo, Japan) under conscious sedation with intravenous midazolam (3–10 mg), supplemented with pentazocine (15 mg) as required. These sedative drugs were re-administered as required during the procedure. Prophylactic antibiotics such as ulinastatin and nafamostat mesylate were administered to almost all patients to prevent cholangitis and pancreatitis. After selective cannulation of the bile duct using a 0.035- or 0.025-inch guidewire (Hydra Jagwire; Boston Scientific Corporation, Marlborough, United States or VisiGlide 2; TERUMO CORPORATION, Tokyo, Japan), routine cholangiography using a cannula (ERCP catheter; MTW Endoskopie, Wesel, Germany) or sphincterotome (Single-Use Sphincterotome V; OLYMPUS MEDICAL SYSTEMS Corp., Tokyo, Japan) was performed. Sphincterotomy was performed at the discretion of the endoscopist using an electrosurgical generator (ICC 200; ERBE Elektromedizin GmbH, Tübingen, Germany). The endoscopist decided which device to use during the procedure. All patients were hospitalized for at least 72 h after the procedure. Serum amylase levels were measured 4 and 24 h after ERCP. Abdominal computed tomography (CT) was performed if required.
Biliary drainage was performed using partially covered and fully covered SEMS. The WallFlex Biliary RX Stent (Boston Scientific Corporation, Marlborough, MA, United States) was used as the braided-type partial CSEMS. The braided-type full CSEMS employed in this study comprised a WallFlex Biliary RX Stent (Boston Scientific Corporation, Marlborough, United States), HANAROSTENT Biliary Full Cover Lasso (M. I. Tech Co., Ltd., Seoul, Korea), BONA-SHIMSTENT Covered with Lasso or BONASTENT M-intraductal (Sewoon Medical Inc., Seoul, Korea), Niti-S biliary silicone covered stent (Taewoong Medical, Seoul, Korea), and EGIS Biliary Stent (S&G Biotech Inc., Yongin-si, Korea). The laser-cut type CSEMS used was the X-Suit NIR Covered Biliary Metallic Stent (Medinol Ltd, Jerusalem, Israel).
Review outpatient visits based on clinical symptoms, blood tests, abdominal radiographs, and/or CT scans were performed every 3 mo until September 2019. Data were retrospectively collected from the medical records at the latest follow-up. Patients who were lost to follow-up, underwent any further surgery, or died without RBO were treated as censored cases at the time of last follow-up, operation, or death, respectively.
RBO and TRBO: According to the TOKYO criteria[10], RBO was defined as a composite endpoint of either occlusion or migration of the CSEMS. TRBO was defined as the time from the placement of CSEMS to occurrence of RBO. Stent occlusion was defined as the presence of elevated liver enzyme levels compared with baseline values, accompanied by biliary dilation on imaging studies or endoscopic findings suggesting it. Stent migration was diagnosed when reintervention revealed a completely or partially migrated CSEMS as the cause of RBO.
Technical success and functional success: Based on the Tokyo criteria recommendations, technical success was defined as successful deployment of the CSEMS in the intended location with sufficient coverage of the stricture, and functional success was defined as a 50% decrease in or normalization of the bilirubin level within 14 d after placement of the CSEMS.
Distal MBO: In this study, distal MBO was defined as a malignant biliary stricture situated ≥ 2 cm from the communication of the bilateral hepatic ducts.
Adverse events: Adverse events were graded according to the American Society of Gastrointestinal Endoscopy lexicon guidelines[11].
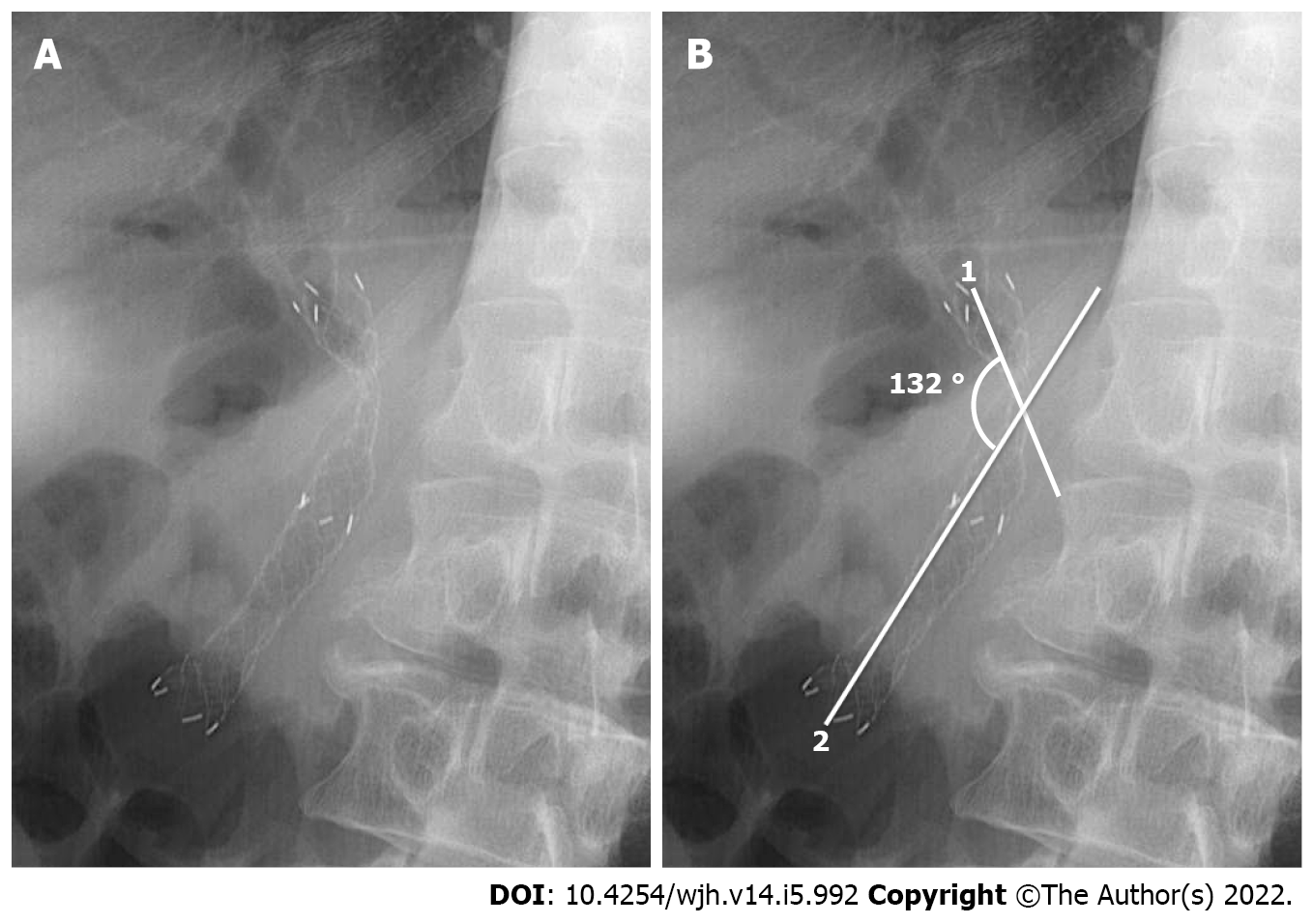
Measurement of the angle of CSEMS after placement: The angle of the CSEMS was retrospectively measured on abdominal radiographs obtained in the standing position using a medical imaging and information management system (SYNAPSE PACS SYSTEM; FUJIFILM Corporation, Tokyo, Japan). As previously reported[12], the angle of CSEMS was defined as the angle between the lines extending from the proximal and distal points to the narrowest point in the CSEMS (Figure 1). The obtuse angle of the CSEMS was evaluated after 2 or more days, and not immediately after placement because the CSEMS was not fully expanded and was unstable in position.
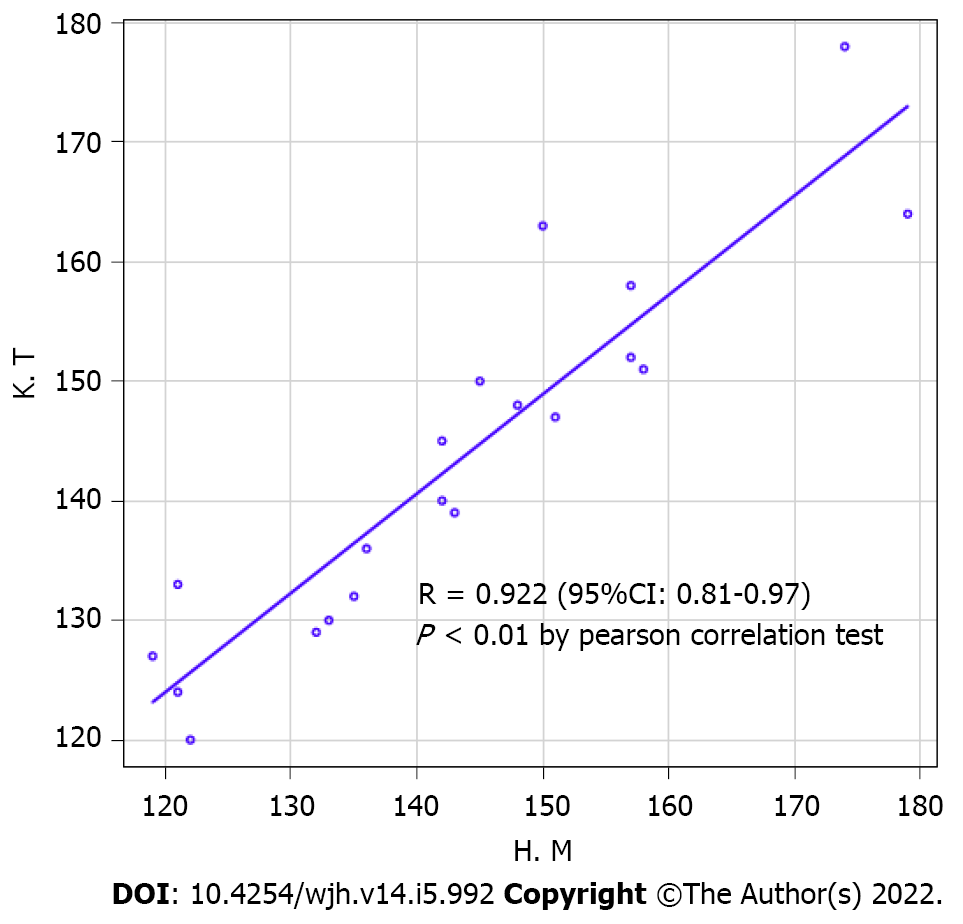
Medians and interquartile ranges (IQRs) are used for continuous variables, while percentages and counts are used for categorical variables. Categorical variables were evaluated using the chi-squared or Fisher’s exact test, and continuous variables were evaluated using the Mann-Whitney U test. Using the Cox proportional hazard model, the risk of RBO following CSEMS placement was estimated by calculating the hazard ratio (HR) and 95% confidence interval (CI). TRBO, non-RBO, and survival time were assessed using the Kaplan-Meier method. Using C-statistics, the model was evaluated for reliability using the Hosmer-Lemeshow test for goodness-of-fit and for validity using receiver operating characteristic (ROC) curves. The Pearson’s correlation test was used to evaluate the consistency of the angle of the CSEMS after placement by two people using a previously reported method[13]. Statistical analyses were performed using IBM SPSS software, version 23.0 for Windows (IBM Corporation, NY, United States) and R software version 2.4.3 (R Foundation for Statistical Computing, Vienna, Austria). All statistical tests were two-sided, and a P value < 0.05 was considered statistically significant.
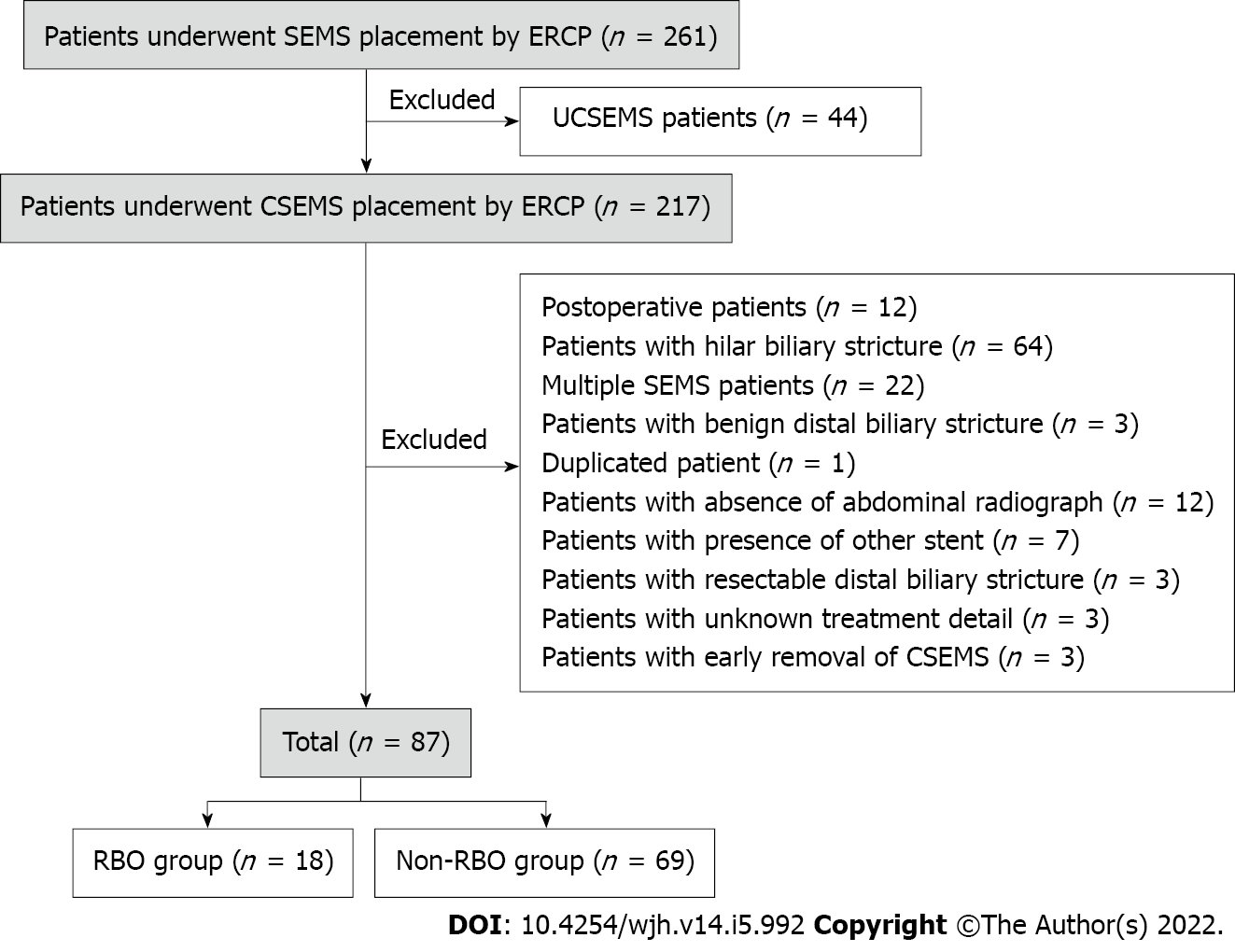
A total of 261 patients were enrolled in this study. Forty-four patients (62 sessions) who were treated with uncovered SEMS were excluded. Among the remaining 217 patients (246 sessions), 12 (13 sessions) had previously undergone surgery, 64 (79 sessions) underwent SEMS placement for hepatic hilar biliary stricture, 22 (24 sessions) underwent the placement of multiple SEMS, 3 (5 sessions) had benign biliary stricture, 1 (10 sessions) had duplication of data, 12 had absent abdominal radiographs, 7 had other stents, 3 had resectable distal MBO, and 3 were unknown, and in 3 patients, CSEMS were removed early due to adverse events. Finally, 87 eligible patients were included who underwent initial CSEMS placement for unresectable distal MBO (Figure 2).
The baseline characteristics of the patients and the treatments implemented are shown in Table 1. Pancreatic cancer was the predominant primary disease, resulting in distal MBO (66.7%), with the most common clinical stage being IV (86.2%). Forty-eight patients (55.2%) received chemotherapy and 11 patients (12.6%) received radiotherapy. Endoscopic sphincterotomy was performed in 60 (69.0 %) patients. The median of the angle of CSEMS after the placement was 146.0° (IQR: 134.5-156.5).
| Baseline characteristic | n = 87 | |
| Age (IQR, yr) | 63.5 (26.0-68.0) | |
| Sex, n (%) | Male | 55 (63.2) |
| Female | 32 (36.8) | |
| ASA-PS, n (%) | 1 | 24 (27.6) |
| 2 | 44 (50.6) | |
| 3 | 19 (21.8) | |
| Primary disease, n (%) | Pancreatic cancer | 58 (66.7) |
| Bile duct cancer | 9 (10.3) | |
| Gallbladder cancer | 2 (2.3) | |
| Ampullary cancer | 2 (2.3) | |
| Duodenal cancer | 2 (2.3) | |
| Other cancers | 14 (16.1) | |
| Clinical stage, n (%) | II | 3 (3.5) |
| III | 9 (10.3) | |
| IV | 75 (86.2) | |
| Chemotherapy, n (%) | Yes | 48 (55.2) |
| Radiotherapy, n (%) | Yes | 11 (12.6) |
| Total bilirubin level (IQR, mg/dL) | 3.8 (2.1-7.7) | |
| Length of stricture (IQR, mm) | 31.5 (21.8-39.3) | |
| Total procedure time (IQR, min) | 32.0 (24.5-48.5) | |
| EST, n (%) | Yes | 60 (69.0) |
| CSEMS type (1), n (%) | Partially | 38 (43.7) |
| Fully | 49 (56.3) | |
| CSEMS type (2), n (%) | Laser-cut | 6 (6.9) |
| Braided | 81(93.1) | |
| Length of CSEMS (cm), n (%) | 4 | 3 (3.5) |
| 5 | 1 (1.1) | |
| 6 | 44 (50.6) | |
| 7 | 10 (11.5) | |
| 8 | 29 (33.3) | |
| Diameter of CSEMS (mm), n (%) | 6 | 3 (3.5) |
| 8 | 3 (3.5) | |
| 10 | 81 (93.0) | |
| Angle of CSEMS (IQR, °) | 146.0 (134.5-156.5) | |
CSEMS were successfully deployed in 87 patients (100.0%), and functional success was observed in 72 patients (82.8%) (Table 2). The overall adverse event rate was 10.3%. The incidence rate of severe acute pancreatitis was 1.1%, and all patients with pancreatitis were managed conservatively. No adverse events associated with cholangitis (including non-occlusion cholangitis), cholecystitis, or other complications (bleeding, perforation, etc.) were observed.
| Classification | n (%) | |
| n = 87 | ||
| Technical success | 87 (100.0) | |
| Functional success | 72 (82.8) | |
| Adverse event | 9 (10.3) | |
| Pancreatitis | 9 (10.3) | |
| Severe | 1 (1.2) | |
| Moderate | 5 (5.7) | |
| Mild | 3 (3.4) | |
| Cholangitis | 0 (0.0) | |
| Cholecystitis | 0 (0.0) | |
| Other complications | 0 (0.0) | |
| n = 18 | ||
| RBO | 18 (100.0) | |
| Sludge formation or food impaction | 11 (61.1) | |
| Tumor overgrowth | 5 (27.8) | |
| Migration | 2 (11.1) | |
| Tumor ingrowth | 0 (0.0) | |
| Reintervention | 18 (100.0) | |
| Metallic stent | 9 (50.0) | |
| Sweep | 5 (27.8) | |
| Plastic stent | 3 (16.7) | |
| Not success | 1 (5.5) | |
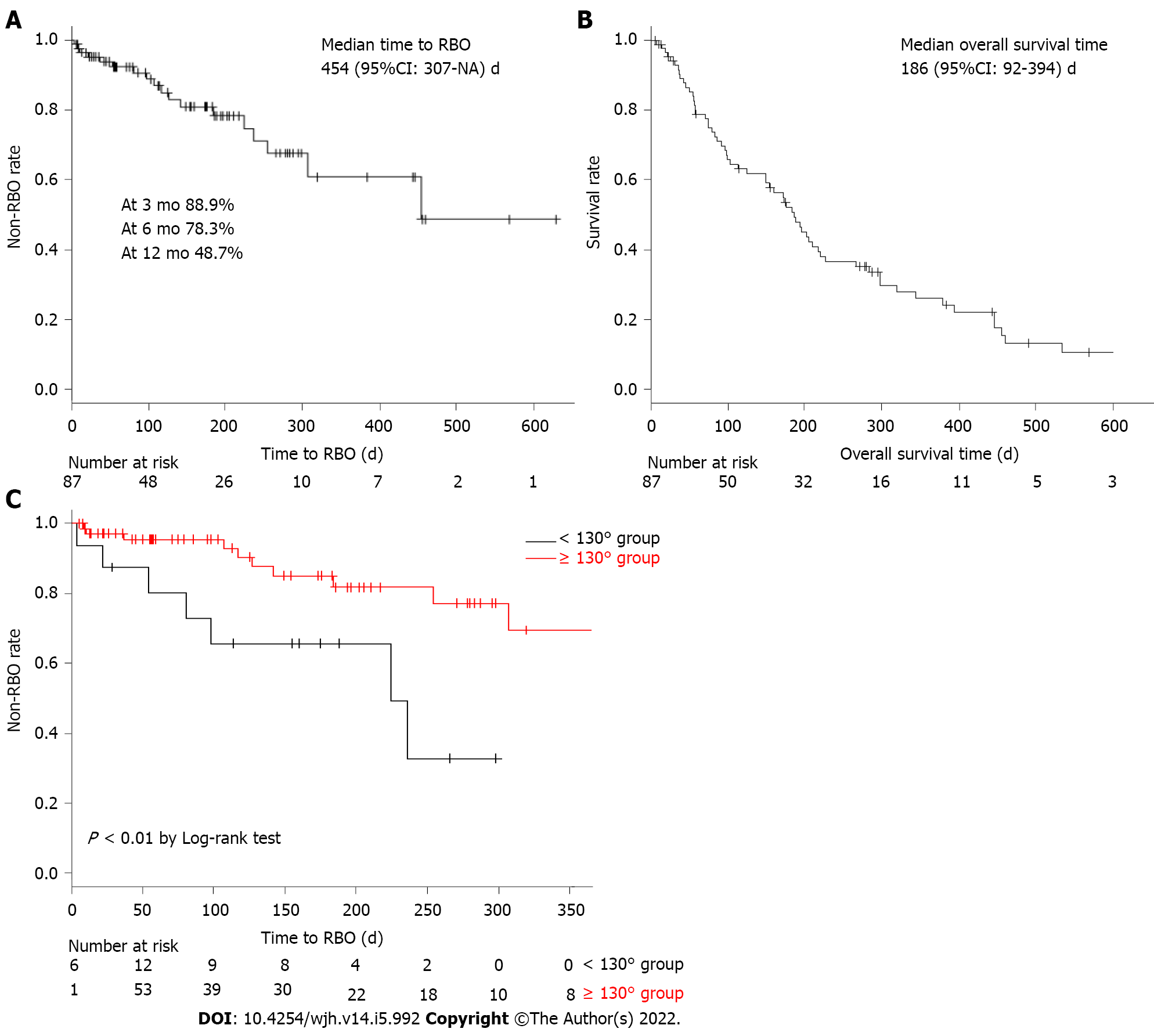
The median TRBO was found to be 454 [95%CI: 307-not available (NA)] d, during a median follow-up period of 117.0 (IQR: 47.5-220.5) d. The non-RBO rates at 3, 6, and 12 mo after CSEMS placement were 88.9%, 78.3%, and 48.7%, respectively (Figure 3A). The median overall survival time was 186 (95%CI: 92-394) d (Figure 3B). The number of patients with RBO after CSEMS placement was 18 (20.7%), and the most common cause of RBO was sludge formation and food impaction (11 cases, 61.1%) (Table 2). Except for tumor overgrowth, the incidence of RBO due to stent occlusion and migration was 72.2%. In 17 of 18 patients with CSEMS, reintervention for RBO was required and performed successfully. The procedures during reintervention included additional CSEMS replacement in nine patients, plastic stent placement in three, and no additional placement in five.
We divided the patients into two cohorts: 18 in the RBO group and 69 in the non-RBO group. The baseline characteristics were similar except for the angle of the CSEMS after placement, which differed significantly between the two groups (P = 0.01) (Table 3). The angle of CSEMS after placement (per 1° and per 10°) was a risk factor for RBO based on the univariate Cox proportional hazard analysis (HR, 0.96; 95%CI, 0.93-0.99; P < 0.01; HR: 0.67; 95%CI: 0.51-0.87; P < 0.01, respectively). In addition to the angle of the CSEMS after placement, we selected the American Society of Anesthesiologists Physical Status and chemotherapy that could potentially be a confounding factor using clinical knowledge[14]. In the multivariate Cox proportional hazard analysis, only the angle of CSEMS after placement (per 1° and per 10°) was significantly associated with shorter duration of RBO (HR: 0.97; 95%CI: 0.94-0.99; P = 0.01; HR: 0.71; 95%CI: 0.54-0.92; P = 0.01, respectively) (Table 4). The angle of CSEMS after placement was an independent risk factor for RBO in unresectable distal MBO.
| RBO group (n = 18) | Non-RBO group (n = 69) | P value | ||
| Age (IQR, yr) | 66.5 (61-77) | 69 (63.5-77) | 0.63 | |
| Sex, n (%) | Female | 5 (27.8) | 27 (39.1) | 0.42 |
| Male | 13 (72.2) | 42 (60.9) | ||
| ASA-PS, n (%) | 1 | 2 (11.1) | 22 (31.9) | 0.07 |
| 2 | 9 (50.0) | 35 (50.7) | ||
| 3 | 7 (38.9) | 12 (17.4) | ||
| Primary disease, n (%) | Other cancers | 8 (44.4) | 21 (30.4) | 0.28 |
| Pancreatic cancer | 10 (55.6) | 48 (69.6) | ||
| Clinical stage, n (%) | II | 1 (5.6) | 2 (2.9) | 0.08 |
| III | 4 (22.2) | 4 (5.8) | ||
| IV | 13 (72.2) | 63 (89.9) | ||
| Chemotherapy, n (%) | No | 8 (44.4) | 31 (44.9) | 1.00 |
| Yes | 10 (55.6) | 38 (55.1) | ||
| Radiotherapy, n (%) | No | 17 (94.4) | 59 (85.5) | 0.45 |
| Yes | 1 (5.6) | 10 (14.5) | ||
| Total bilirubin level (continuous, mg/dL) | 2.7 (1.1-6.7) | 4.4 (2.3-9.0) | 0.07 | |
| Length of stricture (IQR, mm) | 34.9 (25.9-47.2) | 30.9 (21.4-37.8) | 0.13 | |
| Total procedure time (IQR, min) | 35.5 (25-50.8) | 32.0 (24-47) | 0.65 | |
| EST, n (%) | No | 5 (27.8) | 22 (31.9) | 1.00 |
| Yes | 13 (72.2) | 47 (68.1) | ||
| CSEMS type (1), n (%) | Partially | 9 (50.0) | 29 (42.0) | 0.60 |
| Fully | 9 (50.0) | 40 (58.0) | ||
| CSEMS type (2), n (%) | Laser-cut | 1 (5.6) | 5 (7.2) | 1.00 |
| Braided | 17 (94.4) | 64 (92.8) | ||
| Length of CSEMS, n (%) | ≤ 6 cm | 8 (44.4) | 40 (58.0) | 0.55 |
| 7 cm | 3 (16.7) | 7 (10.2) | ||
| 8 cm | 7 (38.9) | 22 (31.9) | ||
| Diameter of CSEMS, n (%) | 6 mm | 0 (0.0) | 3 (4.4) | 0.58 |
| 8 mm | 1 (5.6) | 2 (2.9) | ||
| 10 mm | 17 (94.4) | 64 (92.8) | ||
| Angle of CSEMS (IQR, °) | 135.5 (114.8-149.3) | 149.0 (138.5-158) | 0.01 | |
| n | Case (%) | Univariate analysis | Multivariate analysis | ||||
| Unadjusted HR (95%CI) | P value | Adjusted HR (95%CI) | P value | ||||
| Age (continuous, yr) | 87 | 18 (20.7) | 1.00 (0.95-1.04) | 0.91 | |||
| Sex | Female | 32 | 5 (15.6) | 1.00 | |||
| Male | 55 | 13 (23.6) | 1.44 (0.51-4.05) | 0.49 | |||
| ASA-PS | 1 | 24 | 2 (8.3) | 1.00 | |||
| 2 | 44 | 9 (20.5) | 2.59 (0.56-12.00) | 0.23 | |||
| 3 | 19 | 7 (36.8) | 5.12 (1.06-24.81) | 0.04 | 1.76 (0.85-3.62) | 0.13 | |
| Primary disease | Others | 29 | 8 (27.6) | 1.00 | |||
| Pancreatic cancer | 58 | 10 (17.2) | 0.80 (0.31-2.05) | 0.64 | |||
| Clinical stage | II | 3 | 1 (33.3) | 1.00 | |||
| III | 8 | 4 (50.0) | 2.34 (0.26-21.22) | 0.45 | |||
| IV | 76 | 13 (17.1) | 0.79 (0.10-6.18) | 0.82 | |||
| Chemotherapy | No | 39 | 8 (20.5) | 1.00 | |||
| Yes | 48 | 10 (20.8) | 1.13 (0.44-2.88) | 0.80 | 1.02 (0.40-2.61) | 0.97 | |
| Radiotherapy | No | 76 | 17 (22.4) | 1.00 | |||
| Yes | 11 | 1 (9.1) | 0.43 (0.06-3.24) | 0.41 | |||
| Total bilirubin level (continuous, mg/dL) | 87 | 18 (20.7) | 1.01 (0.99-1.03) | 0.26 | |||
| Length of stricture (continuous, mm) | 87 | 18 (20.7) | 1.03 (1.00-1.07) | 0.10 | |||
| Total procedure time (continuous, min) | 87 | 18 (20.7) | 1.00 (0.98-1.03) | 0.75 | |||
| EST | No | 27 | 5 (18.5) | 1.00 | |||
| Yes | 60 | 13 (21.7) | 1.19 (0.42-3.35) | 0.75 | |||
| CSEMS type (1) | Partially | 38 | 9 (23.7) | 1.00 | |||
| Fully | 49 | 9 (18.4) | 0.85 (0.34-2.15) | 0.73 | |||
| CSEMS type (2) | Laser-cut | 6 | 1 (16.7) | 1.00 | |||
| Braided | 81 | 17 (21.0) | 1.27 (0.17-9.73) | 0.82 | |||
| Length of CSEMS | ≤ 6 cm | 48 | 8 (16.7) | 1.00 | |||
| 7 cm | 10 | 3 (30.0) | 2.33 (0.61-8.89) | 0.22 | |||
| 8 cm | 29 | 7 (24.1) | 1.63 (0.64-4.14) | 0.45 | |||
| Diameter of CSEMS | < 10 mm | 6 | 1 (16.7) | 1.00 | |||
| ≥ 10 mm | 81 | 17 (21.0) | 1.37 (0.18-10.47) | 0.76 | |||
| Angle of CSEMS (continuous, per 10°) | 87 | 18 (20.7) | 0.67 (0.51-0.87) | < 0.01 | 0.71 (0.54-0.92) | 0.01 | |
We evaluated the accuracy of the current study using the ROC curve. For early RBO diagnosis, the angle of 130° had a sensitivity of 50.0% and specificity of 85.5%, and the ROC analysis showed an area under the curve of 0.70 (95%CI: 0.57-0.84) (Figure 4). When comparing the groups based on the angle of CSEMS after placement, TRBO in the < 130° angle group was significantly shorter than that in the ≥ 130° angle group (P < 0.01) (Figure 3C).
Furthermore, we used the Pearson’s correlation test to evaluate the consistency of the obtuse angle of CSEMS after placement. A random number table was created for 87 patients. Of these, 20 patients were randomly sampled. The angle of the CSEMS after placement was evaluated by two board-certified fellows (K.T. and H.M.) of the Japan Gastroenterological Endoscopy Society. A significant positive correlation was observed for the angle of the CSEMS after placement (r = 0.92; 95%CI: 0.81-0.97; P < 0.01) (Figure 5).
We found that the angle of the CSEMS after placement was a risk factor for RBO in unresectable distal MBO. In addition, our study demonstrated that the cut-off value of the angle of CSEMS after placement for RBO was 130° and that TRBO in the group with an angle < 130° was significantly shorter than that in the group with an angle ≥ 130°. This is the first report to demonstrate a new and quantitative risk factor for RBO in CSEMS. We believe that our results are easy for everyone to replicate and provide important information for the management of CSEMS.
A CSEMS angle of < 130° is a risk factor for early RBO. This result suggests that CSEMS with a low AF cause sludge formation, food impaction, and stent migration, which is supported by the results of several previous studies[6,15,16]. First, the placement of a CSEMS with a large diameter across the papilla causes loss of sphincter dysfunction, resulting in duodenal-biliary reflux to the bile duct because of the pressure gradient caused by food or duodenal contents. These results suggest that disruption of the sphincter mechanism may be the most important etiological factor in the development of cholangitis after metallic stent placement for MBO[16]. In addition, previous reports have suggested that food debris is an etiologic factor for acute cholangitis and warned that occlusion might be caused by reflux of duodenal contents[17,18]. CSEMS with a low AF decrease the flow velocity and increase the resistance to bile juice. Therefore, a CSEMS angle of < 130° easily causes sludge formation and food impaction and induces early RBO. Additionally, increased outflow pressure of bile juice leads to an elevated risk of stent migration[19]. In our study, the incidence of RBO in the CSEMS angle < 130° group was inclined to be higher than that in the ≥ 130° group (43.8% vs 15.5%) (Table 5). Isayama et al[8] also demonstrated that a well-bent SEMS with a low AF after placement led to RBO as a result of sludge formation and food impaction[8], which supports our results. However, unlike this previous report, we proposed a versatile index and used abdominal radiography. We believe that the measurement of the CSEMS angle in our results is simple.
| < 130° group | ≥ 130° group | P value | |
| n = 16 | n = 71 | ||
| RBO, n (%) | 7 (43.5) | 11 (15.5) | 0.07 |
| n = 7 | n = 11 | ||
| Cause of RBO, n (%) | 7 (100.0) | 11 (100.0) | |
| Sludge formation or food impaction | 3 (42.9) | 8 (72.7) | |
| Tumor overgrowth | 3 (42.9) | 2 (18.2) | |
| Migration | 1 (14.2) | 1 (9.1) | |
| Tumor ingrowth | 0 (0.0) | 0 (0.0) | |
| Elevated liver enzymes, n (%) | 6 (85.7) | 5 (45.5) |
Our results may have an influence on the stent management after CSEMS placement. Until now, patients with unfavorable prognoses have not been considered for CSEMS replacement. However, it is widely accepted that CSEMS are exchanged when stent occlusion and migration occur. There are no definitive guidelines or literature concerning the management after CSEMS placement. However, this scenario has changed in recent years. With the advent of effective drugs and radiation therapy, patient prognosis has improved[20]. For this reason, stenting has shifted from being used for palliative care to maintaining the overall health status of patients undergoing antitumor therapy as part of multidisciplinary treatment. Therefore, long-term maintenance without stent dysfunction is recommended. However, recent studies have reported that the non-RBO rate at 6 mo was 63%-91% for full CSEMS[6,21,22], and that there was a need for replacement of CSEMS before the patients died.
In our study, among patients who had RBO due to CSEMS in the < 130° angle group, 86% had elevated liver enzyme levels according to the latest laboratory data before the occurrence of RBO compared with previous laboratory data, and all patients were asymptomatic (Table 5). Thus, a potentially high risk of RBO might be considered if the CSEMS angle is < 130° and liver enzyme levels are elevated. Hence, we suggest the replacement of CSEMS even in asymptomatic patients if the liver enzyme levels are elevated and the CSEMS angle is < 130° while managing such patients. We believe that this information has great significance in the management of patients undergoing CSEMS placement in clinical practice. Additionally, by deploying a new CSEMS with a high AF as needed, it is possible to expect long-term maintenance without stent dysfunction.
Our study has the following limitations. First, this was a retrospective cohort study conducted at a single center. We acknowledge that patient assignment to different interventions was subjected to selection bias. There were differences in the length, diameter, and type of CSEMS used in our study, which can influence RBO. However, in multivariate analyses, these factors did not significantly influence RBO. In our results, the angle after placement was a risk factor for RBO regardless of the selected CSEMS characteristics. A larger prospective multicenter study should be conducted to evaluate the obtuse angle of the CSEMS after placement in unresectable distal MBO. Second, we evaluated the angle of the CSEMS after placement using two-dimensional data. Although three-dimensional data, i.e., CT or magnetic resonance imaging, are desirable, we could not evaluate the angle after placement on a unified modality or quantify it using three-dimensional data. However, no previous reports have assessed RBO based on the angle of the CSEMS. Therefore, we consider our method using two-dimensional data to be simple and highly versatile. Third, the actual results of the censored cases were unknown because follow-up data were collected only from medical records.
The angle of the CSEMS after placement is a risk factor for RBO, and the TRBO of the CSEMS with a low AF is shorter than that of other CSEMS. These novel results provide pertinent information for future stent management.
Covered self-expandable metallic stents (CSEMS) cause recurrent biliary obstruction (RBO), which prevents the continuation of treatment and causes the quality of life in patients with unresectable distal malignant biliary obstruction (MBO) to be poor. To date, sludge formation and food impaction have remained to be major causes of RBO. Recently, CSEMS with a low axial force (AF) to improve compatibility with the bile duct have been used frequently, with increasing concerns that they are likely to cause early RBO as a result of sludge formation and food impaction.
We hypothesized that the time to RBO (TRBO) of CSEMS with a low AF was short. We considered that proving this hypothesis has great significance in the management of patients with CSEMS placement in the clinical practice.
We aimed to evaluate whether the angle of CSEMS after placement is a risk factor for RBO in patients with unresectable distal MBO.
Finally, we included 87 patients in this study. We divided the patients into two cohorts, RBO group and non-RBO group, and evaluated the risk factors for RBO including the angle of CSEMS after the placement. Using the SYNAPSE PACS system, we measured the obtuse angle of CSEMS after placement on an abdominal radiograph.
We found that the angle of CSEMS after placement was an independent risk factor for RBO. Further, we demonstrated that the cut-off value for the angle of CSEMS after placement was 130°, and that time to RBO in the < 130° group was significantly shorter than that in the ≥ 130° group. In our study, among patients who caused RBO of CSEMS in the < 130° angle group, 86% had elevated liver enzymes in the latest laboratory data before the occurrence of RBO, compared with previous laboratory data, and all patients were asymptomatic.
The findings suggest that the angle of CSEMS after placement for unresectable distal MBO is a risk factor for RBO, and TRBO of CSEMS with a low AF is shorter than that of other CSEMS. Hence, while managing such patients, we suggest the replacement of CSEMS even in asymptomatic patients if the liver enzymes are elevated and the CSEMS angle is < 130°. Additionally, by deploying a new CSEMS with a high AF as needed, it could be possible to expect long-term maintenance without stent dysfunction.
These results are novel and provide pertinent information for future stent management. However, further prospective studies with larger cohorts are needed to validate our findings.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Amornyotin S, Thailand; Jin ZD, China S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Fan JR
| 1. | Isayama H, Yasuda I, Ryozawa S, Maguchi H, Igarashi Y, Matsuyama Y, Katanuma A, Hasebe O, Irisawa A, Itoi T, Mukai H, Arisaka Y, Okushima K, Uno K, Kida M, Tamada K. Results of a Japanese multicenter, randomized trial of endoscopic stenting for non-resectable pancreatic head cancer (JM-test): Covered Wallstent vs DoubleLayer stent. Dig Endosc. 2011;23:310-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 97] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 2. | Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K. Randomised trial of self-expanding metal stents vs polyethylene stents for distal malignant biliary obstruction. Lancet. 1992;340:1488-1492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 753] [Cited by in RCA: 697] [Article Influence: 21.1] [Reference Citation Analysis (1)] |
| 3. | Katsinelos P, Paikos D, Kountouras J, Chatzimavroudis G, Paroutoglou G, Moschos I, Gatopoulou A, Beltsis A, Zavos C, Papaziogas B. Tannenbaum and metal stents in the palliative treatment of malignant distal bile duct obstruction: a comparative study of patency and cost effectiveness. Surg Endosc. 2006;20:1587-1593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 64] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Moses PL, Alnaamani KM, Barkun AN, Gordon SR, Mitty RD, Branch MS, Kowalski TE, Martel M, Adam V. Randomized trial in malignant biliary obstruction: plastic vs partially covered metal stents. World J Gastroenterol. 2013;19:8638-8646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Isayama H, Komatsu Y, Tsujino T, Sasahira N, Hirano K, Toda N, Nakai Y, Yamamoto N, Tada M, Yoshida H, Shiratori Y, Kawabe T, Omata M. A prospective randomised study of "covered" vs "uncovered" diamond stents for the management of distal malignant biliary obstruction. Gut. 2004;53:729-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 459] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 6. | Kitano M, Yamashita Y, Tanaka K, Konishi H, Yazumi S, Nakai Y, Nishiyama O, Uehara H, Mitoro A, Sanuki T, Takaoka M, Koshitani T, Arisaka Y, Shiba M, Hoki N, Sato H, Sasaki Y, Sato M, Hasegawa K, Kawabata H, Okabe Y, Mukai H. Covered self-expandable metal stents with an anti-migration system improve patency duration without increased complications compared with uncovered stents for distal biliary obstruction caused by pancreatic carcinoma: a randomized multicenter trial. Am J Gastroenterol. 2013;108:1713-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 171] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 7. | Tringali A, Hassan C, Rota M, Rossi M, Mutignani M, Aabakken L. Correction: Covered vs. uncovered self-expandable metal stents for malignant distal biliary strictures: a systematic review and meta-analysis. Endoscopy. 2018;50:C5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Isayama H, Kawakubo K, Nakai Y, Inoue K, Gon C, Matsubara S, Kogure H, Ito Y, Tsujino T, Mizuno S, Hamada T, Uchino R, Miyabayashi K, Yamamoto K, Sasaki T, Yamamoto N, Hirano K, Sasahira N, Tada M, Koike K. A novel, fully covered laser-cut nitinol stent with antimigration properties for nonresectable distal malignant biliary obstruction: a multicenter feasibility study. Gut Liver. 2013;7:725-730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Isayama H, Nakai Y, Kawakubo K, Kogure H, Togawa O, Hamada T, Ito Y, Sasaki T, Yamamoto N, Sasahira N, Hirano K, Tsujino T, Tada M, Koike K. Covered metallic stenting for malignant distal biliary obstruction: clinical results according to stent type. J Hepatobiliary Pancreat Sci. 2011;18:673-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Isayama H, Hamada T, Yasuda I, Itoi T, Ryozawa S, Nakai Y, Kogure H, Koike K. TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc. 2015;27:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 243] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 11. | Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1238] [Cited by in RCA: 1852] [Article Influence: 123.5] [Reference Citation Analysis (1)] |
| 12. | Kim KY, Han J, Kim HG, Kim BS, Jung JT, Kwon JG, Kim EY, Lee CH. Late Complications and Stone Recurrence Rates after Bile Duct Stone Removal by Endoscopic Sphincterotomy and Large Balloon Dilation are Similar to Those after Endoscopic Sphincterotomy Alone. Clin Endosc. 2013;46:637-642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Jeurnink SM, Steyerberg E, Kuipers E, Siersema P. The burden of endoscopic retrograde cholangiopancreatography (ERCP) performed with the patient under conscious sedation. Surg Endosc. 2012;26:2213-2219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Nakai Y, Isayama H, Mukai T, Itoi T, Maetani I, Kawakami H, Yasuda I, Maguchi H, Ryozawa S, Hanada K, Hasebe O, Ito K, Kawamoto H, Mochizuki H, Igarashi Y, Irisawa A, Sasaki T, Togawa O, Hara T, Kamada H, Toda N, Hamada T, Kogure H. Impact of anticancer treatment on recurrent obstruction in covered metallic stents for malignant biliary obstruction. J Gastroenterol. 2013;48:1293-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Bang BW, Jeong S, Lee DH, Lee JI, Lee SC, Kang SG. The biodurability of covering materials for metallic stents in a bile flow phantom. Dig Dis Sci. 2012;57:1056-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Okamoto T, Fujioka S, Yanagisawa S, Yanaga K, Kakutani H, Tajiri H, Urashima M. Placement of a metallic stent across the main duodenal papilla may predispose to cholangitis. Gastrointest Endosc. 2006;63:792-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 66] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Huibregtse K, Cheng J, Coene PP, Fockens P, Tytgat GN. Endoscopic placement of expandable metal stents for biliary strictures--a preliminary report on experience with 33 patients. Endoscopy. 1989;21:280-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 122] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Gordon RL, Ring EJ, LaBerge JM, Doherty MM. Malignant biliary obstruction: treatment with expandable metallic stents--follow-up of 50 consecutive patients. Radiology. 1992;182:697-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 97] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Hamada T, Isayama H, Nakai Y, Iwashita T, Ito Y, Mukai T, Yagioka H, Saito T, Togawa O, Ryozawa S, Hirano K, Mizuno S, Yamamoto N, Kogure H, Yasuda I, Koike K. Antireflux covered metal stent for nonresectable distal malignant biliary obstruction: Multicenter randomized controlled trial. Dig Endosc. 2019;31:566-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 20. | Nabi Z, Reddy DN. Endoscopic Palliation for Biliary and Pancreatic Malignancies: Recent Advances. Clin Endosc. 2019;52:226-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 21. | Kahaleh M, Talreja JP, Loren DE, Kowalski TE, Poneros JM, Degaetani M, Raijman I, Sejpal DV, Patel S, Rosenkranz L, McNamara KN, Brijbassie A, Wang AY, Gaidhane M, Sethi A, Stevens PD. Evaluation of a fully covered self-expanding metal stent with flared ends in malignant biliary obstruction: a multicenter study. J Clin Gastroenterol. 2013;47:e96-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Petersen BT, Kahaleh M, Kozarek RA, Loren D, Gupta K, Kowalski T, Freeman M, Chen YK, Branch MS, Edmundowicz S, Gluck M, Binmoeller K, Baron TH, Shah RJ, Kinney T, Ross W, Jowell P, Carr-Locke D. A multicenter, prospective study of a new fully covered expandable metal biliary stent for the palliative treatment of malignant bile duct obstruction. Gastroenterol Res Pract. 2013;2013:642428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |