Published online May 27, 2022. doi: 10.4254/wjh.v14.i5.911
Peer-review started: February 25, 2021
First decision: May 13, 2021
Revised: May 26, 2021
Accepted: April 20, 2022
Article in press: April 20, 2022
Published online: May 27, 2022
Processing time: 452 Days and 13 Hours
Hepatocellular carcinoma (HCC) is one of the few cancers for which locoregional treatments (LRTs) are included in international guidelines and are considered as a valid alternative to conventional surgery. According to Barcelona Clinic Liver Cancer classification, percutaneous treatments such as percutaneous ethanol injection, radiofrequency ablation and microwave ablation are the therapy of choice among curative treatments in patients categorized as very early and early stage, while transcatheter arterial chemoembolization is considered the better option for intermediate stage HCC. A precise assessment of treatment efficacy and surveillance is essential to optimize survival rate, whereas residual tumor requires additional treatment. Imaging modalities play a key role in this task. Currently, contrast-enhanced computed tomography/magnetic resonance imaging are considered the standard imaging modalities for this purpose. Contrast enhanced ultrasound (CEUS), using second generation contrast agents, plays an increasingly important role in detecting residual disease after LRTs. CEUS is a straightforward to perform, repeatable and cost-effective imaging modality for patients with renal failure or iodine allergies. Due to the ability to focus on single regions, CEUS can also provide high temporal resolution. Moreover, several studies have reported the same or better diagnostic accuracy as contrast-enhanced computed tomography for assessing tumor vascularity 1 mo after LRTs, and recently three-dimensional (3D)-CEUS has been reported as a promising technique to improve the evaluation of tumor response to therapy. Furthermore, CEUS could be used early after procedures in monitoring HCC treatments, but nowadays this indication is still debated, and data from literature are conflicting, especially after transcatheter arterial chemoembolization procedure.
Core Tip: Contrast enhanced ultrasound (CEUS) is playing an increasingly important role to evaluate locoregional treatments efficacy in hepatocellular carcinoma. In this paper, on the basis of personal experience and the relevant literature, we will review and discuss the CEUS technique. We will also highlight the importance of CEUS in evaluating the efficacy and post-procedural surveillance and their efficacy compared to the gold standard contrast-enhanced computed tomography and contrast-enhanced magnetic resonance imaging.
- Citation: Inzerillo A, Meloni MF, Taibbi A, Bartolotta TV. Loco-regional treatment of hepatocellular carcinoma: Role of contrast-enhanced ultrasonography. World J Hepatol 2022; 14(5): 911-922
- URL: https://www.wjgnet.com/1948-5182/full/v14/i5/911.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i5.911
Hepatocellular carcinoma (HCC) represents the sixth most common neoplasm and the third cause of cancer death in the world[1,2]. HCC occurs more often in males than females (2.4:1), but the worldwide incidence is heterogeneous because of the variable prevalence of the risk factors, with a higher incidence in Eastern and Southern Asia and Middle and Western Africa[3].
Chronic liver disease and cirrhosis remain the most important risk factors for the development of HCC regardless of etiology. Hepatitis B and C, alcohol and nonalcoholic fatty liver disease and autoimmune or genetic conditions are independent risk factors for the development of cirrhosis[4].
Development of HCC is a complex multistep process that involves inflammatory liver damage, hepatocyte necrosis and regeneration and fibrotic deposition, leading to increasing liver function impairment. The accumulation of genomic alterations in addition to epigenetic changes runs in parallel with the progression to low-grade dysplastic nodules, high-grade dysplastic nodules, early HCC and advanced HCC[5].
HCC is one of the few cancers for which locoregional treatments (LRTs) are included in international guidelines and have emerged as a valid alternative to conventional surgery[6]. The choice of treatment in patients with HCC is therefore guided not only by tumor staging (defined by number and sizes of nodules, presence of vascular invasion, extrahepatic spread), as in the vast majority of cancers, but also by careful assessment of liver function and general health status[7].
Although several staging systems have been proposed to provide a clinical classification of HCC, the current guidelines of the European Association for the Study of the Liver, European Organization for Research and Treatment of Cancer and American Association for the Study of Liver Disease endorse the Barcelona Clinic Liver Cancer (BCLC) classification[8]. This classification defines the standard of care for each tumor stage. Percutaneous treatments and in particular percutaneous ethanol injection and thermal ablation are included among curative treatments in patients categorized as very early (BCLC stage 0) and early stage (BCLC stage A) when surgical resection or liver transplantation is not feasible or not available. On the other hand, transcatheter arterial chemoembolization (TACE) is considered the best option for intermediate stage (BCLC stage B)[9].
Finally, much hope has been placed in the recognition of novel targets and prognosis predictors through molecular profiling. The combinations of immunotherapy with LRTs are under investigation, representing a promising treatment strategy in advanced HCC[10]. In several preclinical studies this combination has demonstrated increased antitumor immune response due to LRTs effect to increment tumor immunogenicity by inducing inflammation and by releasing tumor-associated antigens[11]. Furthermore, observational and small non-randomized studies have demonstrated the safety of TACE in combination with sorafenib, with manageable toxicities, in patients with intermediate stage HCC and good liver function. However, the combination did not provide meaningful clinical benefit compared with doxorubicin-eluting beads (DEB-TACE) alone[12].
Unfortunately, HCC is known to be a multicentric tumor, often with a poor prognosis. Despite great efforts in terms of primary prevention, surveillance and multidisciplinary approach, incidence and mortality continue to rise. An accurate assessment of therapeutic response is of crucial importance, considering that complete treatment response significantly increases the likelihood of patient survival, whereas residual tumor requires additional treatment[13].
Today, contrast enhanced ultrasound (CEUS) plays an increasingly important role in the management of HCC due to its numerous advantages in comparison with contrast-enhanced computed tomography (CECT) and contrast-enhanced magnetic resonance imaging (CEMRI)[14]
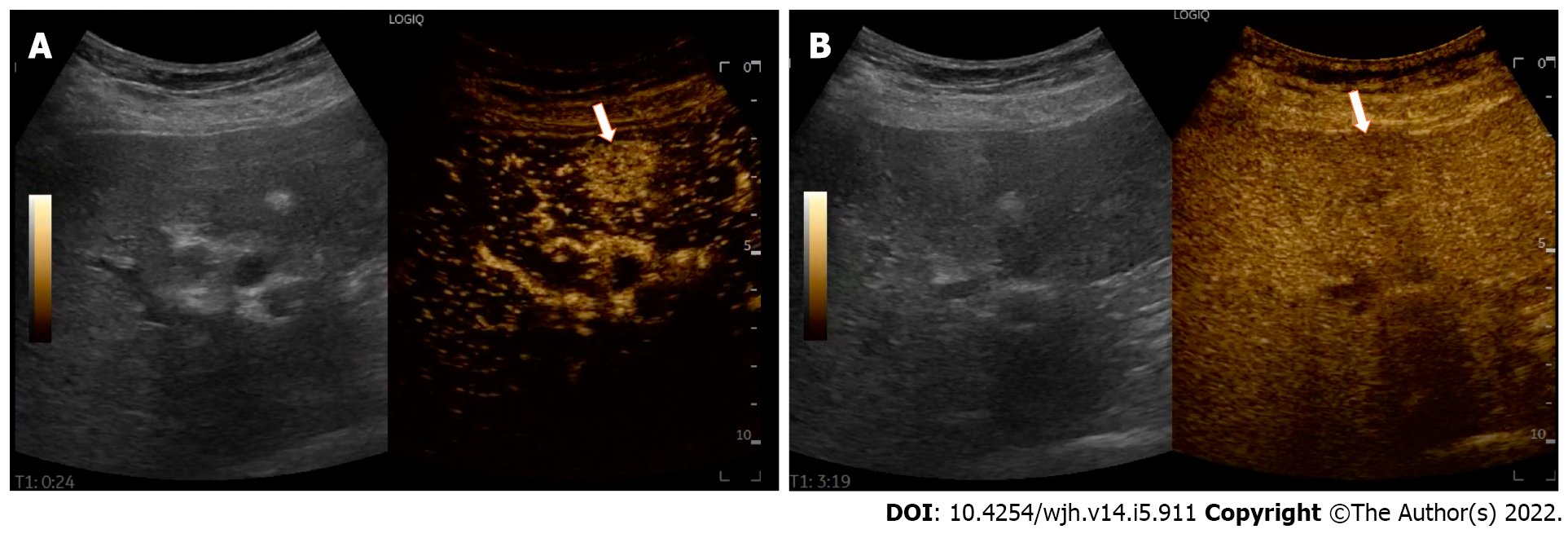
CEUS is a repeatable, cost-effective imaging modality that enables real-time dynamic assessment of liver lesions throughout the vascular phase[15]. Furthermore, CEUS has a much higher temporal resolution compared to other imaging modalities, without the associated radiation burden of CECT or the cost and the long examination time of CEMRI[16]. Compared with the latter, CEUS allows the reading, recording and tracking of every second of the study, without loss of information[17]. CEUS can perfectly depict the contrast-enhancement pattern of HCC[18]. In the arterial-phase, HCC is typically hypervascular and shows a mild and late washout, usually never before 60 s after the completion of contrast injection (Figure 1).
CEUS can be performed during the same interventional procedure session seamlessly. The excellent tolerance and high safety profiles of ultrasound contrast agents (USCAs) make them suitable for patients with renal failure, renal obstruction or allergic to iodine and can be administered more than once during the same examination. The high safety of USCAs was demonstrated by a meta-analysis of 23188 patients examined with CEUS for liver lesions, where the rate of serious adverse events was 0.0086%[19].
For these reasons, many international guidelines currently recommend CEUS as a fundamental imaging modality for the management of HCC, including surveillance, diagnosis, CEUS-guided treatment and treatment response evaluation[20,21].
CEUS exam is performed by intravenously injecting microbubble-based contrast agents. The most widely used of these agents consists of particles with a radius ranging from 1 to 10 μm in diameter, and it is composed of a fluorinated low-solubility gas core encapsulated by a flexible phospholipid shell. Of note, microbubbles, in contrast to the most commonly used contrast agents for computed tomography (CT) and magnetic resonance imaging (MRI), are purely intravascular blood-pool agents. Due to their relatively large size, when injected intravenously they pass through the pulmonary filter and remain in the intravascular space, without an interstitial extravascular phase[17]. The USCAs currently used in diagnostic ultrasound (US) of the liver are: (1) SonoVue (sulfur hexafluoride), Bracco SpA, Milan, Italy, introduced in 2001. Licensed in Europe, China, Hong Kong, Singapore, India, Korea, New Zealand and Brazil; (2) Sonazoid (perfluorobutane), Daiichi-Sankyo, GE Tokyo, Japan, introduced in 2007. Licensed in Japan and South Korea; and (3) Definity/Luminity (octafluoropropane), Lantheus Medical, Billerica, MA, United States, introduced in 2001. Licensed in Canada and Australia[22].
These newer second generation USCAs strongly increase the backscatter of US, and the low solubility of the gas improves their stability and provides good resonance behavior at low-mechanical index (< 0.2). This allows a continuous real time scanning over several minutes to visualize all vascular phases. These features have led to a better sensitivity and the accuracy in the detection of micro- and macro-vasculature of liver tumors[23].
Of note, the only USCA presenting a post-vascular, liver-specific phase is Sonazoid, which is deemed to be taken up by the Kupffer cells of the liver[24].
A baseline US examination is always performed before starting CEUS, including a color/power Doppler and pulsed Doppler analysis to choose the best acoustic window and to identify the target lesion. It is also important to select the best scanning plane either in the axial or long-axis plane and carefully evaluate the cooperation of the patient (i.e. positioning, breath holding), as the lesion has to be visualized during all phases of the CEUS examination. Once set, the US scan parameters, such as time gain compensation and focal zone, they should not be changed during the study. In order to minimize microbubbles disruption, the US scanner is switched to a low mechanical index contrast specific imaging module.
A standard CEUS protocol consists of the injection of 2.4 mL bolus of second generation USCAs followed by a flush of 5/10 mL of normal saline by using an intravenous access 20 G or greater than 20 G cannula. Some investigators use 1.2 mL, but the exact dose may depend on multiple factors, such as the software of the ultrasound equipment used, the size and depth of the lesion and others.
Activation of the timer coincides with the injection of the saline flush. Digital cineloops are acquired both during baseline and post contrast US scanning in 30-60 s intervals for up to 3-5 min to assess for all arterial, portal-venous phase (PVP) and late phase (LP). A post vascular or Kupffer phase for Sonazoid is registered 10 min after injection[22,23,25].
A precise assessment of treatment efficacy and risk of local recurrence is essential to achieve a satisfactory survival rate, whereas residual tumor requires additional treatment[18,20,21,25].
According to modified Response Evaluation Criteria in Solid Tumors, a CECT or CEMRI procedure is deemed successful when there is no enhancing portion within the treated lesion or an irregular peripheral enhancement along the ablative margin during the arterial phase. Moreover, to achieve a complete tumor necrosis, the region ablated beyond the borders of the tumour, ideally, should measure 5 mm in its smallest width[26].
Although today CECT and CEMRI are considered the reference standard in imaging modalities for evaluating treatment after LRTs, CEUS is considered an effective alternative in patients who have kidney failure or iodine allergy[20].
In the last decade many studies supported the importance and validity of CEUS in this peculiar clinical setting[27-29]. Hai et al[30] examined 43 publications to evaluate the overall sensitivity and specificity of CEUS in detection of residual tumor after locoregional therapy, estimated, respectively, to 85% and 94% with a diagnostic accuracy of 93.5%[30].
Percutaneous ablative procedures have been increasingly used for HCC treatment as minimally invasive procedures securing a good local control of tumor[31]. Radiofrequency ablation (RFA) is currently accepted as the best therapeutic choice for patients with very early and early-stage HCC when liver transplant or surgical resection is not a suitable option, providing excellent local control and acceptable morbidity and mortality rates[8,32-34]. Other forms of ablation are cryoablation, microwave ablation (MWA) and irreversible electroporation[35,36]. The latter is the most recent trend in ablation treatment of HCC, especially in patients with contraindications to other commonly used ablative techniques[37,38].
RFA induces thermal injury to tumoral tissue by creating resistive ionic heating (50–100 °C) through an electrode needle delivering high frequency alternating-current. The electrode needle is introduced into the lesion under US guidance[39]. MWA is a relatively new promising ablation procedure for the treatment of HCC. MWA systems uses an alternating electromagnetic field at 915 MHz or 2.45 GHz that has the ability to propagate through a tissue. Heat is generated when the alternating field interacts with tissue water and ions, generating greater ablation zones than RFA in perfused organs[29].
To date there are many studies in scientific literature that show the excellent accuracy of CEUS in detecting residual viable tumor. CECT and CEMRI are the most commonly used modalities for assessing the therapeutic response, however these imaging techniques are normally acquired 1 mo after and not immediately close to percutaneous ablative procedures[27].
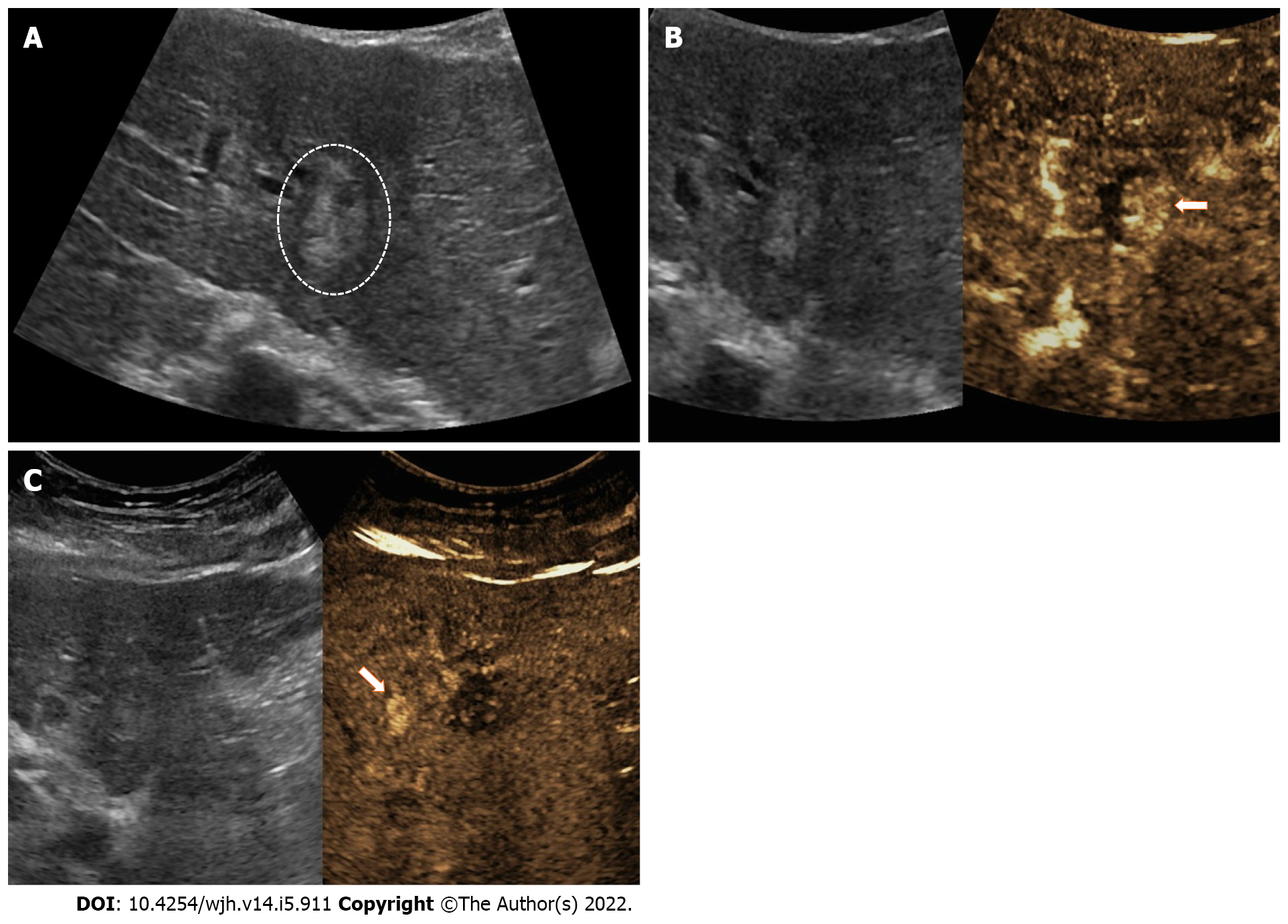
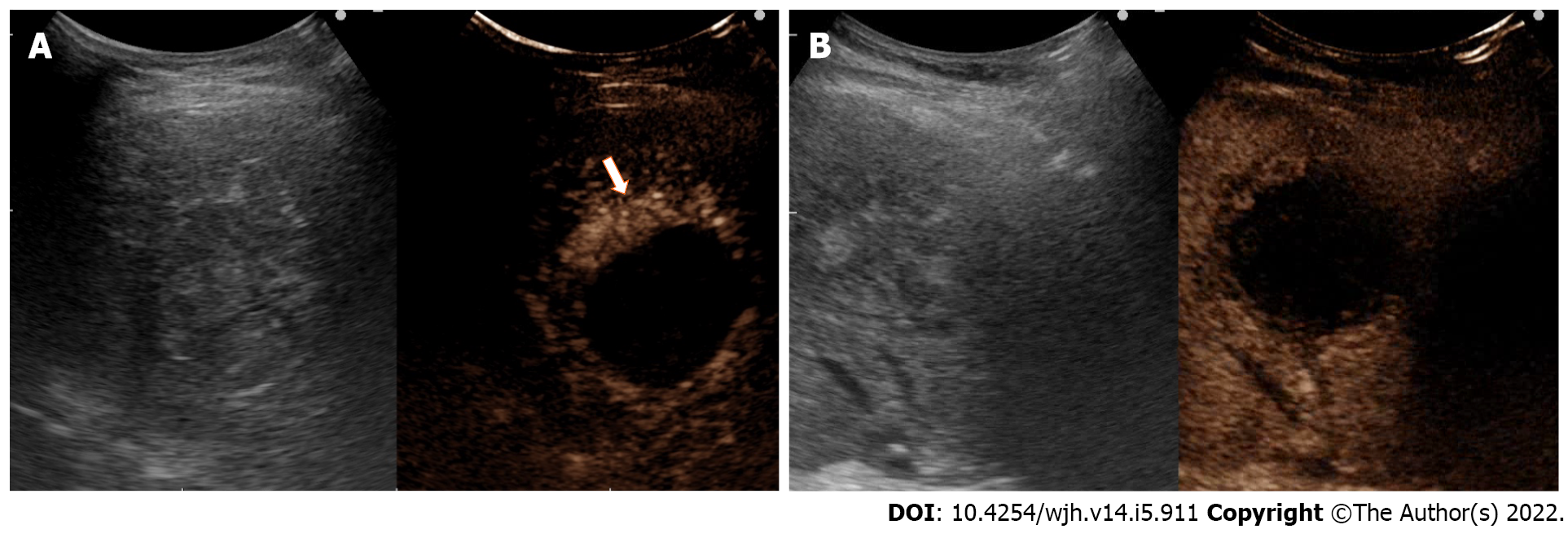
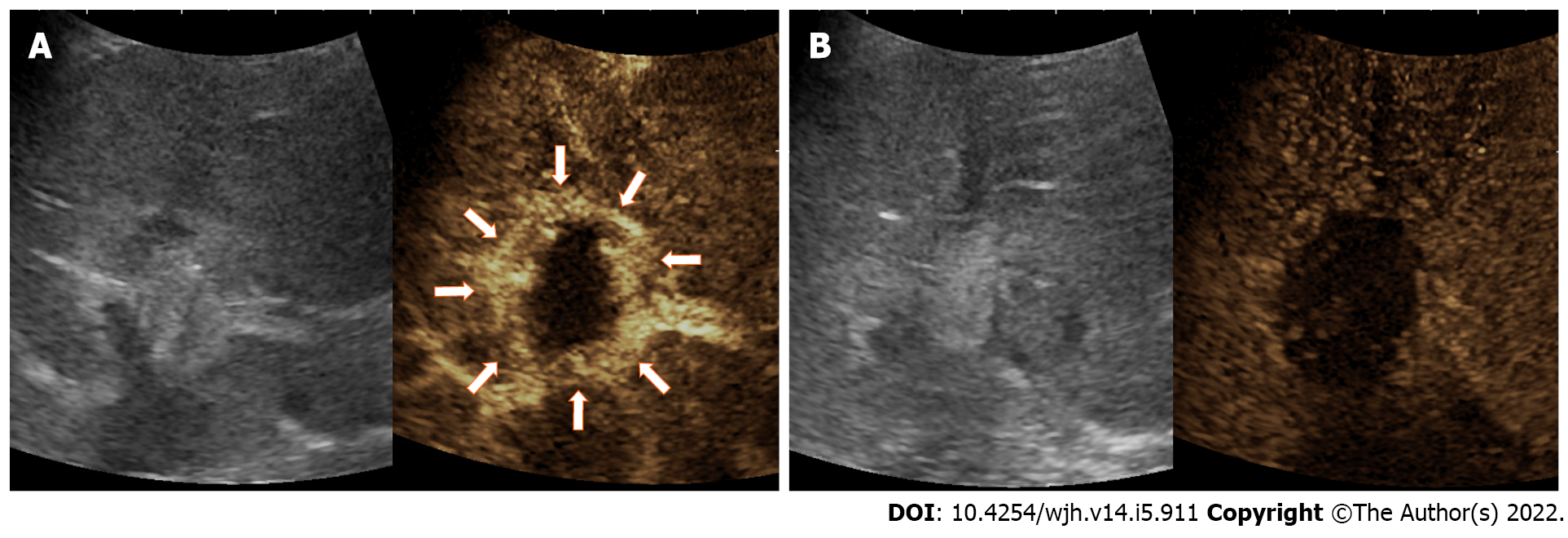
CEUS assessment of LRTs can distinguish a complete response, a partial response and an equivocal treatment response. The lack of any nodular arterially enhancement portion within or at the edge of the ablated HCC is considered a complete response. In contrast, the detection of a residual viable tumor is considered a partial response[26,40]. Partial response may further divided in (1) an ingrowth-pattern when arterial phase hyperenhancement is detected within the edge of a treated nodule (Figure 2); and (2) outgrow-pattern when arterial phase hyperenhancement is detected immediately adjacent to the margin of the treated nodule (Figure 3).
Of note, there are some factors to be aware of when performing immediate postprocedural CEUS. First, as with CECT or CEMRI after RFA, the presence of a peripheral rim of enhancement can reflect a halo of inflammatory hyperemia surrounding the treated zone due to thermal damage. This finding disappears over time and can be distinguished from residual tumor for its characteristic to be a thin (4 mm to 8 mm) regular and peritumoral contrast enhancement and for the absence of wash-out in the PVP and LP (Figure 4). Furthermore, misinterpretation of this perilesional hyperemic halo as residual viable tumor can be avoided by comparing post-ablation images with pre-ablation scans. Hence, it is highly recommended to perform a pre-treatment CEUS study[22,26,41]. Second, during CEUS, the hyperechoic foci in the arterial phase detecting as viable tumor may not have clear washout in portal venous and LP as well as HCC. This underlines the importance of careful evaluation of the arterial phase[26]. Third, after thermal ablative therapies, an ill-defined gas cloud and a hyperechoic artifact are usually seen in the treatment bed. This occurs for the outgassing of water vapor produced by the deposition of high intensity energy. In most cases, it is enough to wait 10-15 min for this artifact to resolve[31].
To date, the latest advancement in fusion technology has permitted to match CT and MRI imaging, with real time US or real time CEUS used for ablation guidance[42,43]. According to recent studies, the fusion technology is better compared to conventional tumor ablation only under US or CEUS guidance, showing respectively an effectiveness rate up to 98.8%–100% compared to 67.7%–93.5%[42,44-46]. This approach exceeds the limit of conventional ablation, taking advantage of the high sensitivity of CT and MRI imaging, in which small HCCs are more detectable, with the coregistered real time US or CEUS for ablation guidance[42,47].
When CEUS is available, it is preferable to US. Indeed, CEUS has the advantage of showing the absence of any nodular arterially enhancement portion within or at the margin of the treated lesion in successfully ablated tumor or remaining enhancing residual tumor in uncompleted ablation[23,48]. Hence, the additional use of CEUS may improve lesion conspicuity, allowing a better rate of satisfying treatment[49]. The result is a more confidence during procedure guidance, especially for those tumors poorly visible with US or CEUS: Lesions located in depth or in the liver dome, small size lesions and hypovascular lesions in a severe cirrhotic liver[43,50].
In conclusion, CEUS/fusion imaging guidance has raised the clinical efficacy of ablation technique, particularly in poor conspicuous HCC, aiding in the visualization and ablation of initial and residual enhancing tissue.
TACE is considerate the best option for intermediate stage liver cancer according to BCLC classification[8,11,12,51].
In conventional TACE protocols, chemotherapeutic drug emulsion containing iodized oil (Lipiodol, Guerbet, France) is delivered through the tumor feeding artery, followed by embolization[7]. CECT is one of the most commonly used modalities, also recommended by modified Response Evaluation Criteria in Solid Tumors criteria, to evaluate a successfully treated site, as indicated by the lack of arterial phase hyperenhancement[52]. However, many studies have shown that CECT may be inconsistent in detecting residual viable tumoral tissue, especially in the early assessment[53-56].
The estimation of tumor necrosis can be troublesome because the residual viable enhancing tumor may be obscured by the artifacts created by the dense accumulation of the ethiodized oil in TACE, not allowing an accurate interpretation of response. Additionally, radiation hazard and renal iodine contrast toxicity often limit repeated applications of CECT in patients with HCC[57]. In a study encompassing 178 patients, Bargellini et al[54] concluded that CECT may overestimate tumor response to TACE with a relatively low specificity (62%) in detecting complete necrosis[54]. Salvaggio et al[55] found that CECT is less sensitive to assess residual contrast enhancement than CEUS[55]. Liu et al[56] concluded that CEUS shows a better diagnostic performance than CECT and, as consequence, CEUS may be more sensitive and accurate to detect residual tumor after TACE, especially when the tumor is completely filled with lipiodol[56].
CEMRI is considered the most accurate imaging modality for the diagnosis and post-procedural assessment of HCC[58,59]. In comparison with CECT, the better contrast resolution of CEMRI allows a high sensitivity in the assessment of enhanced tissue of viable tumor[60-62]. In addition, the multiphasic contrast enhanced sequences are less affected by the intratumoral retention of iodized oil[61,62]. However, high cost, limited availability and breath holding related artifacts may constitute constraints to a widespread application of MRI. In 2015, in a pilot study by Cho et al[58], CECT and CEUS showed sensitivities of 75% and 100%, respectively, when compared with MRI in identifying the presence of residual tumor at 4 wk[58]. In the same study, CEUS also showed a great advantage in the early detection of tumor recurrence or in incomplete treatments[58].
CEUS has been advocated as having equivalent or superior efficacy for assessing HCC response to TACE than CECT, especially for the tumor completely filled with lipiodol[63].
The utility of CEUS in this modality has been debated in literature[23,64]. Some studies found a low sensitivity of CEUS performed immediately after procedure owing to false negative results[65,66]. Moschouris et al[67] suggested that very early assessment may not be suitable in the case of TACE with doxorubicin capable beads because the level of necrosis could be underestimated[67]. These latter were in part associated to technical difficulties secondary to procedure-related artifacts such as gas or uncooperative patients still under conscious sedation or general anesthesia or in pain. Gas-related artifacts may be avoided by waiting at least 5–10 min to 20–40 min after procedure. However, these drawbacks are offset by low cost, ready availability, absence of radiation exposure and the unique CEUS ability of detecting still viable tumor during the RFA session allowing re-treatment in the same procedural setting.
The best advantage of CEUS in monitoring HCC treatments is the possibility to detect tumor vascularization immediately after ablation, permitting retreatment in the same session if needed. A study has shown that CEUS performed within 1 h after RFA had a good agreement with CECT or CEMRI performed 1 mo later[68]. In the same study, CEUS demonstrated a specificity of 94% but a sensitivity of only 40% in the detection of residual disease[68]. Furthermore, Lekht et al[69] showed that performing immediate postprocedural CEUS significantly decreased the incidence of residual tumor seen at follow-up imaging[69]. Moreover, in a study by Mauri et al[70] with 93 patients, residual disease was seen at CT or MRI 24 h after the procedure in 5.4% of patients who underwent immediate postprocedural CEUS, whereas residual disease was seen in 36.5% of the patients who did not undergo postprocedural CEUS[70]. These findings demonstrate the significant role of immediate postprocedural CEUS in optimizing patient management[27,41].
Alternatively, it is possible to perform CEUS at 24-48 h after LRTs[71]. This latter strategy has the disadvantage of not allowing retreatment during the same treatment. However, immediate postprocedural CEUS could be not accessible in all clinical settings, and the aforementioned technical problems could overcome[23].
Nevertheless, the usefulness of CEUS at 24-48 h is still a debated topic, considering that some studies confirm low sensitivity owing to peripheral hyperemia[65,66]. However, a recent study involving 94 patients showed sensitivity and specificity of CEUS performed at 48 h after LRTs (percutaneous ethanol injection, RFA, TACE, combined treatments), respectively, of 79.1% and 96.7% compared to CECT at 1 mo as reference standard[56]. The same authors thinks that tumor position may have affected the results in all false negative cases, confirming that CEUS may not be always practicable due to the inherent inconveniences associated with ultrasound in general. Moreover, peripheral reactive hyperemia may still be a confounding factor even 48 h after the procedure[56].
In our opinion, both CEUS for the immediate postprocedural assessment and CEUS performed at 24-48 h after LRTs could be considered the first choice exam to evaluate quickly the technical success of the ablation without having to wait 4 wk to evaluate response using CECT.
CEUS performed 1 mo after therapy was demonstrated to be valid to identify residual disease after both percutaneous and intra-arterial treatments. Vilana et al[66] reported a sensitivity of 91% and a specificity of 97% after LRTs[66]. Another study demonstrated sensitivity and specificity of CEUS of 87% and 98.4%, respectively, in the evaluation of efficacy 1-mo after ablation treatment of hepatocarcinoma, showing an optimal diagnostic agreement with CT (94.6%)[72]. Hence, several reports have concluded that the sensitivity, specificity and diagnostic accuracy of CEUS in the detection of residual tumor performing at 1-mo is at least equal to that of CECT and CEMRI examinations[66,72-74]. Bansal et al[41] proposed their own protocol with CEMRI performed 1 mo after the treatment, and subsequent imaging performed at 3-mo intervals and the patient alternating between CEUS and MRI for the first 2 years[41].
In our experience, 1-mo CEUS with second generation contrast agents can be considered a good alternative imaging modality to CECT for evaluating the efficacy of HCC therapy, with sensitivity of 92.9% and specificity of 98.8%, when compared to MDCT. However, it must be considered that deep lesions in the liver and irregular reactive peripheral hyperemia could still represent a diagnostic problem even at 1-mo CEUS[23,75].
Three dimensional-CEUS consents the division of structures into tomographic slices in three orthogonal planes, giving additional information unachievable with 2D-CEUS[76]. The bidimensional nature of CEUS makes it impossible to visualize the entire ablated volume but only single planes. Moreover, the vasculature of HCCs may be heterogeneous over the 2D imaging planes, and this represents a limitation of the evaluation of treatment.
The development of real time 3D and four-dimensional US techniques may increase the diagnostic accuracy in detection of hypervascular contrast enhancement, presenting several slices continuously and allowing a superior representation of the whole tumor throughout the vascular phases after the injection of contrast agent[23,77]. During conventional 2D-CEUS there may not be enough time to evaluate in the whole lesion the rapid duration of hyperenhancement during the arterial phase. Covertly 3D-CEUS, permitting acquisition of the volume data of region of interest in a few seconds, could make it easier to evaluate the enhancement of the whole target area.
Furthermore, the volume data are able to be retrieved and thoroughly reviewed from various directions or slice by slice with a sub millimeter thickness. Therefore, 3D-CEUS may pick up some residual tumor tissue that is missed by 2D-CEUS[78,79]. Xu et al[78] used static 3D-CEUS to evaluate the treatment response of liver cancer (n = 107) after local therapies and found that 3D-CEUS improved diagnostic confidence relative to 2D-CEUS[78]. Luo et al[80] compared 3D-CEUS performed 1 d after RFA for the assessment of residual disease using 1-mo 3D-CEUS as reference standard. They have shown a good agreement and a sensitivity, specificity and accuracy of 1-d 3D-CEUS for detecting adequate ablation of 97%, 100% and 97%, respectively[80]. In our preliminary study, 2D- and 3D-CEUS have provided a comparable diagnostic performance in the assessment of therapeutic response of HCC treated with LRTs[77].
We think 3D-CEUS is an increasingly used technique. Current studies showed that 3D-CEUS is a promising technique to improve the evaluation of tumor response to therapy, providing supplementary information unachievable with 2D-CEUS.
CEUS has the identical limitations as conventional B-mode ultrasound imaging. Suboptimal ultrasound technique can lead to ineffective surveillance on CEUS. Hence, general limitations in the use of CEUS in the liver are in patients who have a large body habitus, bad acoustic window, intervening bowel gas and poor physical condition. Moreover, tiny lesions deeply located in the liver parenchyma, especially at depth more than 12 cm, are difficult to interpret because of limited ultrasound wave penetration of a fatty liver[19]. Furthermore, CEUS is not comparable to CECT in case of intra-arterial treatments that include more than one lesion, since each tumor has to be evaluated separately to detect changes in arterial enhancement, even if reinjection of USCA is carried out[13,56].
In summary, CEUS enables in real-time assessment of the therapeutic effect of LRTs in HCC and provides an easy, repeatable and cost-effective way for detecting residual disease. Although CEUS is subject to the same limitation as B-Mode US and is inferior to CECT/ CEMRI in some aspects, CEUS can be considered the first-line exam for the early assessment of treatment efficacy during the interventional procedure to determine the necessity of immediate additional treatment.
CEUS could also be considered the first-line exam in monitoring the efficacy of TACE. Moreover, CEUS can be considered a reliable alternative imaging modality to CECT/CEMRI at 1 mo follow-up and could be used in conjunction with CECT/CEMRI in follow-up.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghoneim S, United States; Shamaa MM, Egypt S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. |
World Health organization.
International Agency for Research on Cancer, Global Cancer Observatory Cancer Today–IARC, Lyon, France, 2018 available |
| 2. | Kulik L, El-Serag HB. Epidemiology and Management of Hepatocellular Carcinoma. Gastroenterology. 2019;156:477-491.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 754] [Cited by in RCA: 1219] [Article Influence: 203.2] [Reference Citation Analysis (1)] |
| 3. | El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2881] [Cited by in RCA: 3088] [Article Influence: 220.6] [Reference Citation Analysis (0)] |
| 4. | Balogh J, Victor D 3rd, Asham EH, Burroughs SG, Boktour M, Saharia A, Li X, Ghobrial RM, Monsour HP Jr. Hepatocellular carcinoma: a review. J Hepatocell Carcinoma. 2016;3:41-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 755] [Cited by in RCA: 807] [Article Influence: 89.7] [Reference Citation Analysis (0)] |
| 5. | El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557-2576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3846] [Cited by in RCA: 4267] [Article Influence: 237.1] [Reference Citation Analysis (2)] |
| 6. | Crocetti L, Bargellini I, Cioni R. Loco-regional treatment of HCC: current status. Clin Radiol. 2017;72:626-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 7. | Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2800] [Cited by in RCA: 4110] [Article Influence: 587.1] [Reference Citation Analysis (6)] |
| 8. | European Association for the Study of the Liver. ; European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5593] [Cited by in RCA: 6064] [Article Influence: 866.3] [Reference Citation Analysis (3)] |
| 9. | Llovet JM, Brú C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19:329-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2645] [Cited by in RCA: 2876] [Article Influence: 110.6] [Reference Citation Analysis (1)] |
| 10. | Prieto J, Melero I, Sangro B. Immunological landscape and immunotherapy of hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2015;12:681-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 338] [Cited by in RCA: 451] [Article Influence: 45.1] [Reference Citation Analysis (0)] |
| 11. | Singh P, Toom S, Avula A, Kumar V, Rahma OE. The Immune Modulation Effect of Locoregional Therapies and Its Potential Synergy with Immunotherapy in Hepatocellular Carcinoma. J Hepatocell Carcinoma. 2020;7:11-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 75] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 12. | Lencioni R, Llovet JM, Han G, Tak WY, Yang J, Guglielmi A, Paik SW, Reig M, Kim DY, Chau GY, Luca A, Del Arbol LR, Leberre MA, Niu W, Nicholson K, Meinhardt G, Bruix J. Sorafenib or placebo plus TACE with doxorubicin-eluting beads for intermediate stage HCC: The SPACE trial. J Hepatol. 2016;64:1090-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 544] [Article Influence: 60.4] [Reference Citation Analysis (0)] |
| 13. | Minami Y, Nishida N, Kudo M. Therapeutic response assessment of RFA for HCC: contrast-enhanced US, CT and MRI. World J Gastroenterol. 2014;20:4160-4166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 53] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Zheng SG, Xu HX, Liu LN. Management of hepatocellular carcinoma: The role of contrast-enhanced ultrasound. World J Radiol. 2014;6:7-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 45] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Ferraioli G, Meloni MF. Contrast-enhanced ultrasonography of the liver using SonoVue. Ultrasonography. 2018;37:25-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 16. | Burrowes DP, Medellin A, Harris AC, Milot L, Wilson SR. Contrast-enhanced US Approach to the Diagnosis of Focal Liver Masses. Radiographics. 2017;37:1388-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Bartolotta TV, Vernuccio F, Taibbi A, Lagalla R. Contrast-Enhanced Ultrasound in Focal Liver Lesions: Where Do We Stand? Semin Ultrasound CT MR. 2016;37:573-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Bartolotta TV, Terranova MC, Gagliardo C, Taibbi A. CEUS LI-RADS: a pictorial review. Insights Imaging. 2020;11:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 19. | Piscaglia F, Bolondi L; Italian Society for Ultrasound in Medicine and Biology (SIUMB) Study Group on Ultrasound Contrast Agents. The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol. 2006;32:1369-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 533] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 20. | Dietrich CF, Nolsøe CP, Barr RG, Berzigotti A, Burns PN, Cantisani V, Chammas MC, Chaubal N, Choi BI, Clevert DA, Cui X, Dong Y, D'Onofrio M, Fowlkes JB, Gilja OH, Huang P, Ignee A, Jenssen C, Kono Y, Kudo M, Lassau N, Lee WJ, Lee JY, Liang P, Lim A, Lyshchik A, Meloni MF, Correas JM, Minami Y, Moriyasu F, Nicolau C, Piscaglia F, Saftoiu A, Sidhu PS, Sporea I, Torzilli G, Xie X, Zheng R. Guidelines and Good Clinical Practice Recommendations for Contrast-Enhanced Ultrasound (CEUS) in the Liver-Update 2020 WFUMB in Cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultrasound Med Biol. 2020;46:2579-2604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 287] [Article Influence: 57.4] [Reference Citation Analysis (0)] |
| 21. | Cassinotto C, Aubé C, Dohan A. Diagnosis of hepatocellular carcinoma: An update on international guidelines. Diagn Interv Imaging. 2017;98:379-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsøe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC, Chaubal NG, Chen MH, Clevert DA, Correas JM, Ding H, Forsberg F, Fowlkes JB, Gibson RN, Goldberg BB, Lassau N, Leen EL, Mattrey RF, Moriyasu F, Solbiati L, Weskott HP, Xu HX. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver--update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med. 2013;34:11-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 224] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 23. | Chung YE, Kim KW. Contrast-enhanced ultrasonography: advance and current status in abdominal imaging. Ultrasonography. 2015;34:3-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 121] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 24. | Salvatore V, Borghi A, Piscaglia F. Contrast-enhanced ultrasound for liver imaging: recent advances. Curr Pharm Des. 2012;18:2236-2252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Dietrich CF, Averkiou M, Nielsen MB, Barr RG, Burns PN, Calliada F, Cantisani V, Choi B, Chammas MC, Clevert DA, Claudon M, Correas JM, Cui XW, Cosgrove D, D'Onofrio M, Dong Y, Eisenbrey J, Fontanilla T, Gilja OH, Ignee A, Jenssen C, Kono Y, Kudo M, Lassau N, Lyshchik A, Franca Meloni M, Moriyasu F, Nolsøe C, Piscaglia F, Radzina M, Saftoiu A, Sidhu PS, Sporea I, Schreiber-Dietrich D, Sirlin CB, Stanczak M, Weskott HP, Wilson SR, Willmann JK, Kim TK, Jang HJ, Vezeridis A, Westerway S. How to perform Contrast-Enhanced Ultrasound (CEUS). Ultrasound Int Open. 2018;4:E2-E15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 246] [Cited by in RCA: 222] [Article Influence: 31.7] [Reference Citation Analysis (33)] |
| 26. | Bartolotta TV, Taibbi A, Midiri M, De Maria M. Hepatocellular cancer response to radiofrequency tumor ablation: contrast-enhanced ultrasound. Abdom Imaging. 2008;33:501-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 27. | Lu MD, Yu XL, Li AH, Jiang TA, Chen MH, Zhao BZ, Zhou XD, Wang JR. Comparison of contrast enhanced ultrasound and contrast enhanced CT or MRI in monitoring percutaneous thermal ablation procedure in patients with hepatocellular carcinoma: a multi-center study in China. Ultrasound Med Biol. 2007;33:1736-1749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 28. | Catalano O, Izzo F, Vallone P, Sandomenico F, Albino V, Nunziata A, Fusco R, Petrillo A. Integrating contrast-enhanced sonography in the follow-up algorithm of hepatocellular carcinoma treated with radiofrequency ablation: single cancer center experience. Acta Radiol. 2015;56:133-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Cui R, Yu J, Kuang M, Duan F, Liang P. Microwave ablation vs other interventions for hepatocellular carcinoma: A systematic review and meta-analysis. J Cancer Res Ther. 2020;16:379-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Hai Y, Savsani E, Chong W, Eisenbrey J, Lyshchik A. Meta-analysis and systematic review of contrast-enhanced ultrasound in evaluating the treatment response after locoregional therapy of hepatocellular carcinoma. Abdom Radiol (NY). 2021;46:5162-5179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 31. | Crocetti L, de Baére T, Pereira PL, Tarantino FP. CIRSE Standards of Practice on Thermal Ablation of Liver Tumours. Cardiovasc Intervent Radiol. 2020;43:951-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 88] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 32. | Lencioni R, Della Pina C, Bartolozzi C. Percutaneous image-guided radiofrequency ablation in the therapeutic management of hepatocellular carcinoma. Abdom Imaging. 2005;30:401-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 33. | Choi D, Lim HK, Rhim H, Kim YS, Lee WJ, Paik SW, Koh KC, Lee JH, Choi MS, Yoo BC. Percutaneous radiofrequency ablation for early-stage hepatocellular carcinoma as a first-line treatment: long-term results and prognostic factors in a large single-institution series. Eur Radiol. 2007;17:684-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 245] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 34. | Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Ierace T, Solbiati L, Gazelle GS. Hepatocellular carcinoma: radio-frequency ablation of medium and large lesions. Radiology. 2000;214:761-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 806] [Cited by in RCA: 741] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 35. | Nault JC, Sutter O, Nahon P, Ganne-Carrié N, Séror O. Percutaneous treatment of hepatocellular carcinoma: State of the art and innovations. J Hepatol. 2018;68:783-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 283] [Article Influence: 40.4] [Reference Citation Analysis (0)] |
| 36. | Sutter O, Calvo J, N'Kontchou G, Nault JC, Ourabia R, Nahon P, Ganne-Carrié N, Bourcier V, Zentar N, Bouhafs F, Sellier N, Diallo A, Seror O. Safety and Efficacy of Irreversible Electroporation for the Treatment of Hepatocellular Carcinoma Not Amenable to Thermal Ablation Techniques: A Retrospective Single-Center Case Series. Radiology. 2017;284:877-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 111] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 37. | Bhutiani N, Philips P, Scoggins CR, McMasters KM, Potts MH, Martin RC. Evaluation of tolerability and efficacy of irreversible electroporation (IRE) in treatment of Child-Pugh B (7/8) hepatocellular carcinoma (HCC). HPB (Oxford). 2016;18:593-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 38. | Park MJ, Kim YS, Rhim H, Lim HK, Lee MW, Choi D. A comparison of US-guided percutaneous radiofrequency ablation of medium-sized hepatocellular carcinoma with a cluster electrode or a single electrode with a multiple overlapping ablation technique. J Vasc Interv Radiol. 2011;22:771-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 39. | Wu M, Gao S, Song H, Zhang Z, Wang J, Liu R, Wang X, Cheng J, Luo J, Liu Q, Chen Y, Yan Z, Liu L. Percutaneous thermal ablation combined with simultaneous transarterial chemoembolization for hepatocellular carcinoma ≤5 cm. J Cancer Res Ther. 2019;15:766-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 40. | Ahmed M, Solbiati L, Brace CL, Breen DJ, Callstrom MR, Charboneau JW, Chen MH, Choi BI, de Baère T, Dodd GD 3rd, Dupuy DE, Gervais DA, Gianfelice D, Gillams AR, Lee FT Jr, Leen E, Lencioni R, Littrup PJ, Livraghi T, Lu DS, McGahan JP, Meloni MF, Nikolic B, Pereira PL, Liang P, Rhim H, Rose SC, Salem R, Sofocleous CT, Solomon SB, Soulen MC, Tanaka M, Vogl TJ, Wood BJ, Goldberg SN; International Working Group on Image-guided Tumor Ablation; Interventional Oncology Sans Frontières Expert Panel; Technology Assessment Committee of the Society of Interventional Radiology,; Standard of Practice Committee of the Cardiovascular and Interventional Radiological Society of Europe. Image-guided tumor ablation: standardization of terminology and reporting criteria--a 10-year update. Radiology. 2014;273:241-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 628] [Cited by in RCA: 897] [Article Influence: 81.5] [Reference Citation Analysis (0)] |
| 41. | Bansal S, Gui J, Merrill C, Wong JK, Burak KW, Wilson SR. Contrast-enhanced US in Local Ablative Therapy and Secondary Surveillance for Hepatocellular Carcinoma. Radiographics. 2019;39:1302-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 42. | Eisenbrey JR, Gabriel H, Savsani E, Lyshchik A. Contrast-enhanced ultrasound (CEUS) in HCC diagnosis and assessment of tumor response to locoregional therapies. Abdom Radiol (NY). 2021;46:3579-3595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 43. | Minami Y, Kudo M. Image Guidance in Ablation for Hepatocellular Carcinoma: Contrast-Enhanced Ultrasound and Fusion Imaging. Front Oncol. 2021;11:593636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 44. | Xu EJ, Lv SM, Li K, Long YL, Zeng QJ, Su ZZ, Zheng RQ. Immediate evaluation and guidance of liver cancer thermal ablation by three-dimensional ultrasound/contrast-enhanced ultrasound fusion imaging. Int J Hyperthermia. 2018;34:870-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 45. | Clevert DA, Paprottka PM, Helck A, Reiser M, Trumm CG. Image fusion in the management of thermal tumor ablation of the liver. Clin Hemorheol Microcirc. 2012;52:205-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 46. | Monsky W, Keravnou C, Averkiou M. Contrast-enhanced ultrasound to ultrasound fusion during microwave ablation: feasibility study in a perfused porcine liver model. J Ultrasound. 2019;22:323-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Mauri G, Cova L, De Beni S, Ierace T, Tondolo T, Cerri A, Goldberg SN, Solbiati L. Real-time US-CT/MRI image fusion for guidance of thermal ablation of liver tumors undetectable with US: results in 295 cases. Cardiovasc Intervent Radiol. 2015;38:143-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 165] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 48. | Li K, Su Z, Xu E, Huang Q, Zeng Q, Zheng R. Evaluation of the ablation margin of hepatocellular carcinoma using CEUS-CT/MR image fusion in a phantom model and in patients. BMC Cancer. 2017;17:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 49. | Bartolotta TV, Taibbi A, Randazzo A, Gagliardo C. New frontiers in liver ultrasound: From mono to multi parametricity. World J Gastrointest Oncol. 2021;13:1302-1316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (2)] |
| 50. | Lee MW, Kim YJ, Park HS, Yu NC, Jung SI, Ko SY, Jeon HJ. Targeted sonography for small hepatocellular carcinoma discovered by CT or MRI: factors affecting sonographic detection. AJR Am J Roentgenol. 2010;194:W396-W400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 51. | Llovet JM, Real MI, Montaña X, Planas R, Coll S, Aponte J, Ayuso C, Sala M, Muchart J, Solà R, Rodés J, Bruix J; Barcelona Liver Cancer Group. Arterial embolisation or chemoembolisation vs symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359:1734-1739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2502] [Cited by in RCA: 2611] [Article Influence: 113.5] [Reference Citation Analysis (0)] |
| 52. | Gregory J, Dioguardi Burgio M, Corrias G, Vilgrain V, Ronot M. Evaluation of liver tumour response by imaging. JHEP Rep. 2020;2:100100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 53. | Kim YS, Rhim H, Lim HK, Park CK, Lee WJ, Do YS, Cho JW. Completeness of treatment in hepatocellular carcinomas treated with image-guided tumor therapies: Evaluation of positive predictive value of contrast-enhanced CT with histopathologic correlation in the explanted liver specimen. J Comput Assist Tomogr. 2006;30:578-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 54. | Bargellini I, Bozzi E, Campani D, Carrai P, De Simone P, Pollina L, Cioni R, Filipponi F, Bartolozzi C. Modified RECIST to assess tumor response after transarterial chemoembolization of hepatocellular carcinoma: CT-pathologic correlation in 178 Liver explants. Eur J Radiol. 2013;82:e212-e218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 55. | Salvaggio G, Campisi A, Lo Greco V, Cannella I, Meloni MF, Caruso G. Evaluation of posttreatment response of hepatocellular carcinoma: comparison of ultrasonography with second-generation ultrasound contrast agent and multidetector CT. Abdom Imaging. 2010;35:447-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 56. | Liu M, Lin MX, Lu MD, Xu ZF, Zheng KG, Wang W, Kuang M, Zhuang WQ, Xie XY. Comparison of contrast-enhanced ultrasound and contrast-enhanced computed tomography in evaluating the treatment response to transcatheter arterial chemoembolization of hepatocellular carcinoma using modified RECIST. Eur Radiol. 2015;25:2502-2511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 57. | Malone CD, Fetzer DT, Monsky WL, Itani M, Mellnick VM, Velez PA, Middleton WD, Averkiou MA, Ramaswamy RS. Contrast-enhanced US for the Interventional Radiologist: Current and Emerging Applications. Radiographics. 2020;40:562-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 58. | Cho YZ, Park SY, Choi EH, Baik SK, Kwon SO, Kim YJ, Cha SH, Kim MY. The usefulness of contrast-enhanced ultrasonography in the early detection of hepatocellular carcinoma viability after transarterial chemoembolization: pilot study. Clin Mol Hepatol. 2015;21:165-174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 59. | Minami Y, Kudo M. Imaging Modalities for Assessment of Treatment Response to Nonsurgical Hepatocellular Carcinoma Therapy: Contrast-Enhanced US, CT, and MRI. Liver Cancer. 2015;4:106-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 60. | Shao L, Wang X, Yu Y, Xie J. Comparative analysis of the efficacy and accuracy of magnetic resonance imaging (MRI) and contrast-enhanced CT for residual and new lesions after transcatheter arterial chemoembolization (TACE) in patients with primary liver cancer. Transl Cancer Res. 2021;10:3739-3747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 61. | Kele PG, van der Jagt EJ. Diffusion weighted imaging in the liver. World J Gastroenterol. 2010;16:1567-1576. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 106] [Cited by in RCA: 110] [Article Influence: 7.3] [Reference Citation Analysis (2)] |
| 62. | Liu HF, Zou LQ, Lu XR, Sheng Y, Wang Q, Ding JL, Shi L, Liu SQ, Xing W. Diagnostic Efficacy of Contrast-Enhanced MRI in Detecting Residual or Recurrent Hepatocellular Carcinoma After Transarterial Chemoembolization: A Systematic Review and Meta-analysis. J Magn Reson Imaging. 2020;52:1019-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 63. | Minami Y, Kudo M, Kawasaki T, Kitano M, Chung H, Maekawa K, Shiozaki H. Transcatheter arterial chemoembolization of hepatocellular carcinoma: usefulness of coded phase-inversion harmonic sonography. AJR Am J Roentgenol. 2003;180:703-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 64. | Ainora ME, Iezzi R, Ponziani FR, Garcovich M, Di Stasio E, Riccardi L, Annicchiarico BE, Abbate V, De Gaetano AM, Siciliano M, Grieco A, Rapaccini GL, Gasbarrini A, Pompili M, Zocco MA. Contrast-Enhanced Ultrasound in the Short-Term Evaluation of Hepatocellular Carcinoma after Locoregional Treatment. Dig Dis. 2020;38:522-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 65. | Meloni MF, Andreano A, Zimbaro F, Lava M, Lazzaroni S, Sironi S. Contrast enhanced ultrasound: Roles in immediate post-procedural and 24-h evaluation of the effectiveness of thermal ablation of liver tumors. J Ultrasound. 2012;15:207-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 66. | Vilana R, Bianchi L, Varela M, Nicolau C, Sánchez M, Ayuso C, García M, Sala M, Llovet JM, Bruix J, Bru C; BCLC Group. Is microbubble-enhanced ultrasonography sufficient for assessment of response to percutaneous treatment in patients with early hepatocellular carcinoma? Eur Radiol. 2006;16:2454-2462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 87] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 67. | Moschouris H, Malagari K, Papadaki MG, Kornezos I, Matsaidonis D. Contrast-enhanced ultrasonography of hepatocellular carcinoma after chemoembolisation using drug-eluting beads: a pilot study focused on sustained tumor necrosis. Cardiovasc Intervent Radiol. 2010;33:1022-1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 68. | Dill-Macky MJ, Asch M, Burns P, Wilson S. Radiofrequency ablation of hepatocellular carcinoma: predicting success using contrast-enhanced sonography. AJR Am J Roentgenol. 2006;186:S287-S295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 69. | Lekht I, Gulati M, Nayyar M, Katz MD, Ter-Oganesyan R, Marx M, Cen SY, Grant E. Role of contrast-enhanced ultrasound (CEUS) in evaluation of thermal ablation zone. Abdom Radiol (NY). 2016;41:1511-1521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 70. | Mauri G, Porazzi E, Cova L, Restelli U, Tondolo T, Bonfanti M, Cerri A, Ierace T, Croce D, Solbiati L. Intraprocedural contrast-enhanced ultrasound (CEUS) in liver percutaneous radiofrequency ablation: clinical impact and health technology assessment. Insights Imaging. 2014;5:209-216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 103] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 71. | Faccia M, Garcovich M, Ainora ME, Riccardi L, Pompili M, Gasbarrini A, Zocco MA. Contrast-Enhanced Ultrasound for Monitoring Treatment Response in Different Stages of Hepatocellular Carcinoma. Cancers (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 72. | Pompili M, Riccardi L, Covino M, Barbaro B, Di Stasi C, Orefice R, Gasbarrini G, Rapaccini GL. Contrast-enhanced gray-scale harmonic ultrasound in the efficacy assessment of ablation treatments for hepatocellular carcinoma. Liver Int. 2005;25:954-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 73. | Kim HJ, Kim TK, Kim PN, Kim AY, Ko EY, Kim KW, Sung KB, Ha HK, Kim HC, Lee MG. Assessment of the therapeutic response of hepatocellular carcinoma treated with transcatheter arterial chemoembolization: comparison of contrast-enhanced sonography and 3-phase computed tomography. J Ultrasound Med. 2006;25:477-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 74. | Choi D, Lim HK, Lee WJ, Kim SH, Kim YH, Lim JH. Early assessment of the therapeutic response to radio frequency ablation for hepatocellular carcinoma: utility of gray scale harmonic ultrasonography with a microbubble contrast agent. J Ultrasound Med. 2003;22:1163-1172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 75. | Bartolotta TV, Midiri M, Galia M, Runza G, Bellia M, Lagalla R. Usefulness of sonovue-enhanced pulse-inversion ultrasonography to assess hepatocellular carcinoma response after percutaneous radiofrequency thermal ablation therapy. [cited 10 January 2021]. Available from: https://www.researchgate.net/publication/266125757_Usefulness_of_SonoVue-enhanced_Pulse-Inversion_Ultrasonography_to_Assess_Hepatocellular_Carcinoma_Response_after_Percutaneous_Radiofrequency_Thermal_Ablation_Therapy. |
| 76. | Bartolotta TV, Sidoti Pinto A, Cannella R, Porrello G, Taravella R, Randazzo A, Taibbi A. Focal liver lesions: interobserver and intraobserver agreement of three-dimensional contrast-enhanced ultrasound-assisted volume measurements. Ultrasonography. 2021;40:333-341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 77. | Bartolotta TV, Taibbi A, Matranga D, Midiri M, Lagalla R. 3D vs 2D contrast-enhanced sonography in the evaluation of therapeutic response of hepatocellular carcinoma after locoregional therapies: preliminary findings. Radiol Med. 2015;120:695-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 78. | Xu HX, Lu MD, Xie XH, Xie XY, Kuang M, Xu ZF, Liu GJ, Wang Z, Chen LD, Lin MX. Treatment response evaluation with three-dimensional contrast-enhanced ultrasound for liver cancer after local therapies. Eur J Radiol. 2010;76:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 79. | Xu HX, Lu MD, Xie XH, Xie XY, Xu ZF, Chen LD, Liu GJ, Liang JY, Lin MX, Wang Z, Huang B. Three-dimensional contrast-enhanced ultrasound of the liver: experience of 92 cases. Ultrasonics. 2009;49:377-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 80. | Luo W, Numata K, Morimoto M, Oshima T, Ueda M, Okada M, Takebayashi S, Zhou X, Tanaka K. Role of Sonazoid-enhanced three-dimensional ultrasonography in the evaluation of percutaneous radiofrequency ablation of hepatocellular carcinoma. Eur J Radiol. 2010;75:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |