Published online Mar 27, 2022. doi: 10.4254/wjh.v14.i3.504
Peer-review started: March 29, 2021
First decision: June 15, 2021
Revised: July 9, 2021
Accepted: February 19, 2022
Article in press: February 19, 2022
Published online: March 27, 2022
Processing time: 360 Days and 4.8 Hours
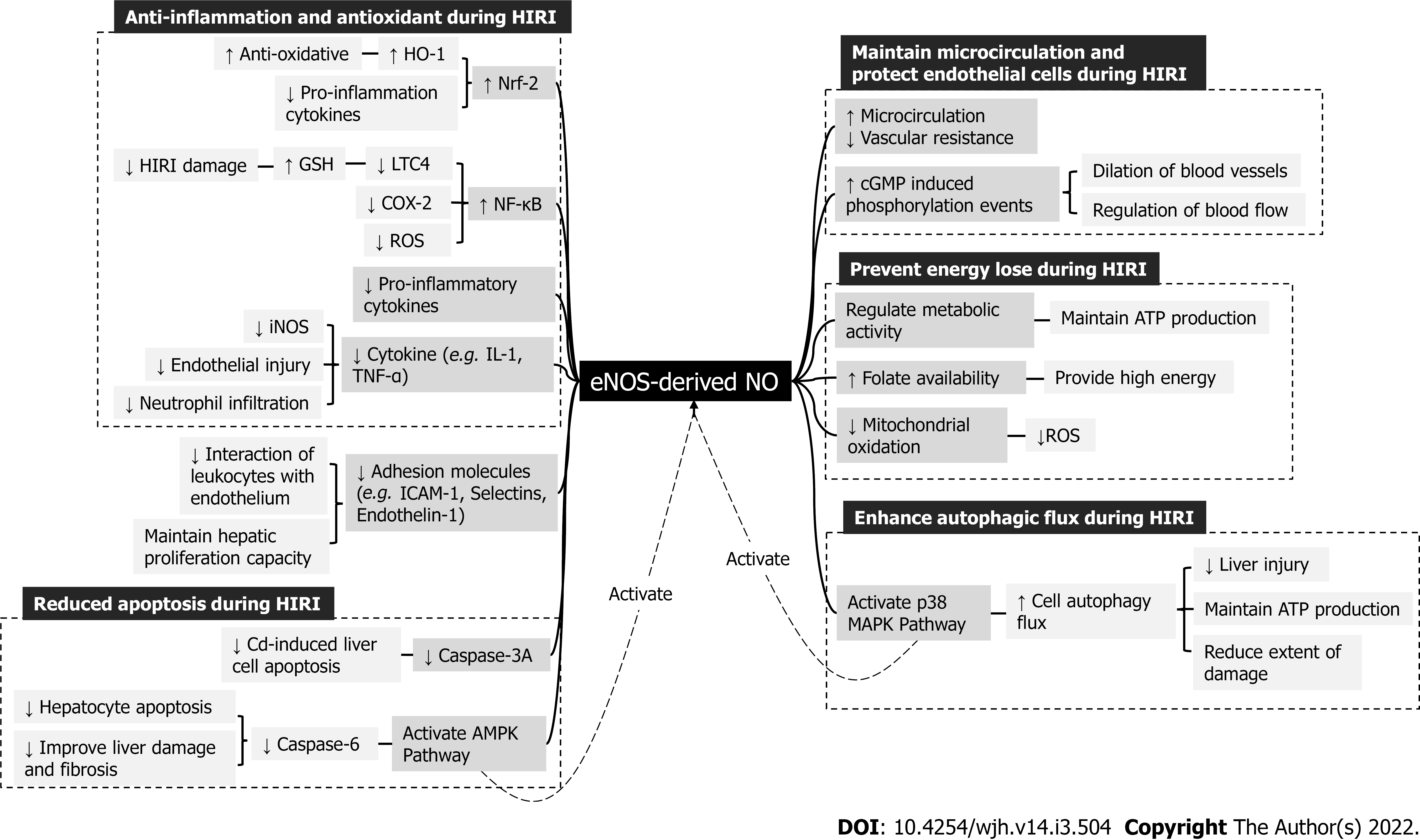
Hepatic ischemia-reperfusion injury (HIRI) is a major clinical cause of morbidity and mortality in liver surgery and transplantation. Many studies have found that nitric oxide (NO) plays an important role in the HIRI and its increase or decrease can affect the progression and outcome of HIRI. However, the role of NO in HIRI is controversial and complicated. NO derived by endothelial NO synthase (eNOS) shows a protective role in HIRI, while excessive NO derived by inducible NO synthase (iNOS) accelerates inflammation and increases oxidative stress, further aggravating HIRI. Nevertheless, the overexpression of eNOS may exacerbate HIRI and iNOS-derived NO in some cases reduces HIRI. Here we review the new progress in the understanding of the roles of NO during HIRI: (1) NO possesses different roles in HIRI by increasing NO bioavailability, down-regulating leukotriene C4 synthase, inhibiting the activation of the nuclear factorκB (NFκB) pathway, enhancing cell autophagy, and reducing inflammatory cytokines and reactive oxygen species (ROS). And NO has both protective and deleterious effects by regulating apoptotic factors; (2) eNOS promotes NO production and suppresses its own overexpression, exerting a hepatoprotective effect reversely. Its activation is regulated by the PI3K/Akt and KLF2/AMPK pathways; and (3) iNOS derived NO mainly has deteriorating effects on HIRI, while it may have a protective function under some conditions. Their expression should reach a balance to reduce the adverse side and make NO protective in the treatment of HIRI. Thus, it can be inferred that NO modulating drugs may be a new direction in the treatment of HIRI or may be used as an adjunct to mitigate HIRI for the purpose of protecting the liver.
Core Tip: This review focuses on the new progress in the understanding of the role of nitric oxide (NO) in hepatic ischemia-reperfusion injury (HIRI). NO protects HIRI by increasing NO bioavailability and cellular autophagy, down-regulating leukotriene C4 synthase, inhibiting the nuclear factor κB (NF-κB) pathway, and reducing inflammatory cytokines and reactive oxygen species. While by regulating apoptotic factors, it has dual effects. eNOS exerts hepatoprotective effects by promoting NO production through the involvement of the phosphoinositide 3-kinase/Akt pathway and Kruppel-like factor 2/adenosine monophosphate-activated protein kinase pathways. The function of eNOS overexpression remains controversial. iNOS-derived NO mainly deteriorates HIRI, but it may reduce damage under certain conditions. The balance of eNOS and iNOS is important for the HIRI protection.
- Citation: Zhang YP, Liu XR, Yang MW, Yang SL, Hong FF. New progress in understanding roles of nitric oxide during hepatic ischemia-reperfusion injury. World J Hepatol 2022; 14(3): 504-515
- URL: https://www.wjgnet.com/1948-5182/full/v14/i3/504.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i3.504
Hepatic ischemia-reperfusion injury (HIRI) is a major complication often seen in liver surgery and organ transplantation. It manifests as cellular damage during the ischemic phase and worsens during reperfusion. Depending on the different conditions of ischemia, HIRI can be divided into warm ischemia-reperfusion (WIR) injury and cold ischemia-reperfusion injury (IRI), which have similar pathophysiology but different clinical injury sites[1].
With a high incidence of cases, liver cancer has increased by 114.0% and ended up with 1007800 cases in 2016[2]. Many liver cancer patients are supposed to be treated by liver transplantation or hepatectomy, where HIRI occurs during the operation [3]. Although HIRI is receiving increasing attention to improve the success rate of surgery and improve prognosis, very few of them are known.
The pathophysiological process of hepatic IRI involves the interaction of many different cell types and numerous signaling pathways such as anaerobic metabolism, acidosis, oxidative stress, and intracellular calcium overload. Among the interactions, the imbalance in the ratio of endothelin (ET) to nitric oxide (NO) is one of the mechanisms involved in HIRI. Normally, their function is to regulate blood flow to the hepatic sinusoids. In contrast, in the first few hours after reperfusion, as ET rises, plasma expression of NO decreases, leading to an increase in the ET/NO ratio and the possible appearance of HIRI[4,5].
Many pieces of evidence show that NO plays an important role in ischemia-reperfusion (I/R)[6,7]. However, as a vasodilator, the role of NO has been controversially discussed by scientists[8,9]. In past studies, NO was regarded as a negative factor because of its cytotoxic effect[10]. Nevertheless, a recent study indicated that NO can induce either a positive or negative effect during the early phase of HIRI and have a protective effect during late HIRI[11]. Therefore, it is important to further explore the protective mechanism of NO in HIRI.
NO is a small molecule free radical that can easily penetrate cell membranes. It is also an important effector and messenger molecule of biological information, which has undergone many extensive types of research in the past few years. There are two sources of NO in the human body—enzymatic production and non-enzymatic production. Non-enzymatic production mainly comes from chemical degradation and inorganic nitrogen transformation on the body surface or ingested. For enzymatic production, NO is oxidized from L-arginine by NO synthase (NOS)[12].
There are Ca2+-independent and Ca2+-dependent NOS in the human body. Ca2+-dependent NOS can be subdivided into neuronal (nNOS) and endothelial (eNOS). eNOS is an enzyme continuously expressed in vascular endothelial cells and exerts biological functions through producing NO. In contrast to eNOS, Ca2+-independent inducible NOS (iNOS) is activated by some exterior factors including viruses, bacteria, pro-inflammatory interferon, and cytokines[13]. iNOS produces a large amount of NO in hepatocytes, cholangiocytes, and Kupffer cells (KCs), helping macrophages to mount an immune response[14].
eNOS and iNOS are believed to take actions in HIRI. While depending on different isoforms of NOS, NO has a dual effect on hepatocellular functions during IR. eNOS-derived NO is hepatoprotective of ischemia following IRI by improving hepatic microcirculation and counteracting the deteriorate functions of reactive oxygen species (ROS) [4]. However, an augmented level of iNOS activation upon reperfusion will produce excessive NO, resulting in endothelial dysfunction and aggravating liver damage in HIRI[14]. It has been reported that iNOS-derived NO may have a positive or negative function in HIRI depending on the different conditions[15].
This review aims to find the role of NO during HIRI and look for candidate ways to alleviate liver damage (Table 1).
| Pretreatment | NO/ iNOS/ eNOS levels | Animals | Experimental cells | Mechanism | Liver cell necrosis and liver damage | Ref. |
| NMP, BMMSCs, and liver CDC | eNOS↑, iNOS↓ | SPF rats | Liver tissue | Macrophage activation, ICAM-1, VCAM-1, vWF↓ | ↓ | [5] |
| L-NAME and BDL | iNOS mRNA↓ | Male Wistar rats | Liver tissue | TGF-β, NOx, HA↓; AMDA↑ | [6] | |
| Simvastatin and WIR | NO↑ | Male Wistar rats | Primary LSEC | Nitrotyrosines, O2-↓; Nrf2, HO-1↑ | ↓ | [14] |
| Simvastatin and WIR | NO, eNOS↑ | Male Wistar rats | LSEC | KLF2, p-eNOS, cGMP↑; | ↓ | [16] |
| Obestatin and HIRI | eNOS↑, iNOS↓ | Adult Wistar albino male rats | Liver tissue samples | Reducing oxidative stress and inflammatory process | ↓ | [17] |
| HIRI | NO↑ | Male Sprague-Dawley rats | Liver | Decrease synthesis of LTC4S, NF-κB↓ | ↓ | [18,19] |
| V-PYRRO/NO and HIRI | NO↑ | Male Sprague-Dawley rats | Liver | Decrease synthesis of LTC4S, NF-κB↓ | ↓ | [20] |
| AMPK–caspase-6 axis and nonalcoholic steatohepatitis | - | LAKO mice | Hepatocyte | Caspases-6 activation | ↓ | [21] |
| Cd-Induced Apoptosis | NO↑ iNOS↑ | Hy-Line Brown laying hen | Liver | Mitochondrial apoptotic pathway | ↓ | [23] |
| Punicalagin and cyclophosphamide | NO, iNOS↓ | Sprague-Dawley male rats | Liver | Reduce cell apoptosis | ↓ | [25] |
| Emblica officinalisGaertn and NAP | NO↓ | Male Wistar rats | Liver | Apoptosis, autophagy, inflammation↓ | ↓ | [28] |
| Tormentic acid and LPS/ D-GalN | NO, iNOS↓ | Male C57BL/6 mice | Liver samples | TNF-α, NF-κB↓; imbalanced Bax/Bcl-2 ratio | ↓ | [30] |
| Selenocysteine-containing 7-mer peptide | NO↓ | Adult male Wistar rats | Liver tissue | Inhibit oxidant peroxynitrite, Bax↓; Bcl-2↑ | ↓ | [34] |
| IPC and HIRI | NO↑ | Male C57BL/6 mice | Liver tissue | p38 MAPK↑; autophagy↑ | ↓ | [35] |
| Simvastatin and hepatic transplantation | NO↑ | Male rats | Liver | Autophagy↑ | ↓ | [36] |
| IPC | NO↑ | Male Sprague-Dawley rats | Liver | Oxygen species liberation and proinflammatory cytokine↓; microcirculation↑ | ↓ | [37] |
| Oxytocin and HIRI | NO↑ | Adult male albino (Sprague Dawley strain) | Liver | NO bioavailability↑ | ↓ | [38] |
| TELL and HIRI | eNOS↑ | Male Wistar rats | Liver | Activate PI3K/Akt pathway, suppress TLR4, p-PI3K, p-Akt, Nrf2, p-NF-κB p65, p-MAPK p38, TNF-α, GSH, MyD88, HMGB-1, TBARS↑; NF-κB↓ | ↓ | [42] |
| Apelin preconditioning and HIRI | eNOS↑ | Male albino rats | Liver tissue | Activate PI3K/Akt pathway, suppress AT1R, counteract Ang II/AT1R system | ↓ | [43] |
| Simvastatin and WIR | eNOS↑ | Male inbred Sprague Dawley rats | Liver tissue | Activate KLF2 pathway, TM, p-eNOS↑, TGF-β, TNF-α, IL- 1β↓ | ↓ | [44] |
| HMP and liver DCD | NO, eNOS↑ | Adult male Sprague-dawley rat | Liver | KLF2↑; NF-κB p65, IL-1β, TNF-α↓ | ↓ | [45] |
| TMZ and WIR | eNOS↑ | Male Wistar rats | Liver tissue | p-MAPK↑; activate MAPK pathway | ↓ | [46] |
| IGL-1 and Fatty Liver Graft Cold Storage | eNOS↑ | Homozygous (obese) Zücker rats | Liver | Activate MAPK pathway, ATP↑ | ↓ | [48] |
| SEW2871 and WIR | eNOS↑ | Male C57BL/6 mice | SECs | VE-cadherin, p-Akt↑; IFN-γ, TNF-α, IL-6, VCAM-1↓ | ↓ | [49] |
| EPO and liver transplantation | eNOS↑ | Female landrace pigs | Liver tissue | Activate JAK2/PI3/AKT pathway, AMPK↑; βcR2-VEGFR-2 complex | ↓ | [51] |
| HIRI | - | Female domestic (Landrace) pigs | Liver tissue | IL-6, STAT-3 and E-selectin mRNA↑ | - | [52] |
| TDF and HIRI | eNOS, iNOS↓ | Female Wistar albino rats | Liver tissue | cGMP↑, activate mitochondrial K-ATP channels, mitochondrial | ↓ | [53] |
| PTX and HIRI | eNOS, iNOS↓ | cAMP↑ TNF-α, IL-1, IL-6, IL-12, TGF-β, IFN-γ, procollagen-I mRNA↓ | ↓ | |||
| L-NNA and HIRI | iNOS↑, eNOS, NO↓ | Male Wistar rats | Liver | TNF-α, NF-κB↑, Bcl-2↓ | ↑ | [54] |
| L-Arginine/CDN and HIRI | NO, eNOS↑, iNOS↓ | TNF-α, NF-κB↓, Bcl-2↑ | ↓ | |||
| iNOS knockout and WIR | iNOS↓ | C57BL/6 male rats | 293 T cells | PUMA↓ | ↑ | [55] |
| NAC and HIRI | eNOS↑, iNOS↓ | Male Wister albino rats | Liver | NOSTRIN, MDA, MPO activity↓ | ↓ | [56] |
| TQ and HIRI | eNOS↑, iNOS↓ | NOSTRIN, MDA, oxidative stress, nitrosative stress↓, GSH↑ | ↓ | |||
| LA and HIRI | iNOS mRNA↓ | Male Wistar rats | Liver | NF-κB p65, MIP-2 mRNA, GSH↓ | ↓ | [57] |
| V and HIRI | NO, iNOS mRNA↓ | Male Wistar rats | Lung and Liver tissue | Inhibit HIF-α/HGF/iNOS pathway | ↓ | [58] |
| Eupatilin and HIRI | iNOS↓ | Male C57BL/6 mice | Embryonic liver BNL CL.2 cell | TLR2/4, p-IκB-a↓, Bcl-2↑ | ↓ | [59] |
| N-SMase inhibitor and HIRI | iNOS | Male Wistar rats | Liver tissue | Protein nitration, nitrite/nitrate levels, HNE | [60] | |
| Ad-eNOS and small-for-size liver transplatation | NO, eNOS↑ | - | Human normal liver cell line L02 | TNF-α↓, inhibit macrophage activation | ↓ | [61] |
| Ad-eNOS and HIRI | eNOS↑ | Male inbred C57BL6 lean mice | Liver | ATP↓, bax, p53↑ | ↓ | [62] |
Recently, studies have showed that NO has a significant role during the HIRI, which can be a positive protective function or negative deleterious function. NO was proved to reduce HIRI through various mechanisms such as increasing NO bioavailability, down-regulating leukotrienes (LTs), inhibiting liver cell apoptosis, enhancing autophagic flux, maintaining liver microcirculation blood flow, stabilizing ATP levels, and reducing oxidative stress injury. Whereas, NO can also regulate some apoptotic signal pathways to accelerate the apoptosis of hepatic tissue.
Hide et al[16] found that NO bioavailability was reduced during reperfusion by detecting the levels of cyclic guanosine monophosphate, a second messenger of NO. They concluded that the decreased NO bioavailability can be explained by the reduction of eNOS activity leading to less synthesis of NO and increased NO clearance by reacting with ROS and forming peroxynitrite, which may later react with cell components such as proteins, lipids, and DNA, further damaging the cell. Therefore, increasing NO bioavailability can protect the liver from further damage during HIRI. It is reported that obestatin enhances NO bioavailability by up-regulating eNOS expression[17]. Also, simvastatin maintains NO bioavailability by preventing kruppel-like factor 2 (KLF2) down-regulation[16].
Many studies reveal that cysteinyl leukotrienes are directly associated with hepatic IRI. Leukotriene C4 synthase (LTC4S) is one of the enzymes that are responsible for LTC4 synthesis, showing a strong relationship with the NO[18,19]. In I/R rats, the gene expression level of LTC4S is much higher. However, this is reversed by V-PYRRO/NO, which acts as an NO donor. Hong et al[20] also found that another NO donor, sodium nitroprusside, could down-regulate the mRNA expression of LTC4S by inhibiting nuclear factor-kappa B (NF-κB) activation in an NF-κB α inhibitor-independent manner by detecting the protein levels of NF-κB p65 and p50 in the nuclear extracts using Western Blot.
NO has a significant role in regulating some apoptotic signal transduction pathways which can be potentially activated to induce or inhibit the hepatic cell apoptosis process caused by HIRI during the hepatic operation or other hepatic diseases. The signal pathways or apoptosis-related genes including caspases[21-25], Bcl-2 gene family[26-30], mitogen-activated protein kinase (MAPK)[31], and NF-kB[32]. Studies have shown that the caspase family is strongly related to hepatic cell apoptosis[33]. Zhao et al[21] found that steatosis-induced decline in adenosine monophosphate-activated protein kinase (AMPK)-catalyzed phosphorylation permits caspase-6 activation, leading to hepatocyte death. And Gao et al[22] indicated that caspase-3A is involved in cadmium (Cd)-induced cell apoptosis in common carp, which showed 71.8% sequence similarity and 59.3% sequence identity to human caspase-3. Zhang et al[23] found that Cd treatment increased the level of iNOS and NO. The overexpression of NO leads to chicken hepatic cell apoptosis by inducing the mitochondrial apoptotic pathway. In two other studies, mouse liver cell apoptosis can be inhibited by reducing NO content, down-regulating Bax protein expression, and increasing Bcl-2 protein expression[24,25]. Besides, an imbalanced Bax/Bcl-2 ratio is caused by decreasing levels of NO and iNOS and increasing Bcl-2 expression through the NF-kB pathway. And this imbalanced ratio may show a protective role in the damaged liver[30]. Jiang et al[34] also found that 7-mer peptide can increase the level of Bcl-2 and decrease the level of Bax expression to reduce apoptosis and protect against IRI.
NO has an important role in protecting against I/R-induced liver injury by enhancing autophagic flux. During severe environments such as IRI, the cell will undergo an autophagic process, which is an adaptive response to reduce the injury. Studies have found that the protective mechanism of NO during HIRI is associated with autophagic flux. Shin et al[35] demonstrated that NO could enhance light chain-3 lipidation and autophagosome-lysosome fusion during hepatic I/R. Also, eNOS-induced NO enhances autophagy via p38 MAPK activation during liver I/R. Simvastatin, which is used to protect the donor liver, can activate autophagy and increase NO release during hepatic transplantation. This also indicates the possible connection between NO and autophagy[36].
During reperfusion, the surge of inflammatory factors, cytokine liberation, neutrophil infiltration and ROS generation occurred, which led to hepatic injury. An increased level of NO can reduce cytokines such as tumor necrosis factor-α (TNF-α) and interleukin (IL)-1 which stimulate infiltration and endothelial injury. Also, continuous NO production can reduce ROS and proinflammatory cytokine generation as well as neutrophil infiltration[37]. Inversely, NO deficiency can induce TNF-α expression as a result of ROS surging. Ragy et al[38] proved this by adding Nomega-nitro-L-arginine methyl ester (L-NAME) in IRI model rats treated with oxytocin. In this group, not only did the parameter damage increase but also the inflammatory factor such as TNF-α level increased compared with the control group.
eNOS performs various biological functions by promoting the production of NO, which is important for maintaining vascular tone and cardiovascular hemostasis, and inhibiting platelet activation and aggregation. It has been confessed that eNOS shows a hepatoprotective effect in HIRI by improving the production of NO (Figure 1).
There are two main regulation pathways for eNOS activation, one dependent on intracellular concentration of Ca2+ and the other independent. The increasing intracellular Ca2+ level can enhance the affinity of calmodulin binding to eNOS and activate enzymes to produce NO[39]. For the Ca2+-independent regulation pathway, phosphorylation of the Ser1177 residue or dephosphorylation of the Thr495 residue activates it to produce NO[40].
At the early stage of HIRI, the ischemia will lead to a shortage of oxygen and nutrients, which can decrease ATP availability. Without energy, ATP-dependent ion channels or transporters cannot work. The incompetence of the Na+/K+ pump leads to depolarization of the cell membrane, resulting in the influx of Ca2+[41]. Besides, anaerobic glycolysis induces an increase in H+, which activates intracellular proteases to increase cellular permeability. Furthermore, Na+/Ca2+ exchange is activated due to a high concentration of H+, leading to a further influx of Ca2+. Consequently, eNOS is activated due to the increase of intracellular concentration to produce NO, carrying anti-HIRI activities at the initial stage.
Phosphoinositide 3-kinase/Akt pathway induced eNOS activation: The phosphoinositide 3-kinase (PI3K)/Akt signaling pathway is a cell survival pathway that regulates cell proliferation and apoptosis, as well as an endogenous negative feedback regulator that functions in anti-inflammation and anti-apoptosis effects in IR.
PI3K can activate Akt to act on the phosphorylation of eNOS. It has been proven that telluric acid has a hepatoprotective effect by elevating the expression of eNOS, which is accompanied with elevated expression of p-PI3K and p-Akt proteins. Besides, the activation of PI3K/Akt also inhibits NF-κB and activates nuclear erythroid-related factor-2, reducing pro-inflammation cytokine expression and inducing anti-oxidative effects[42]. Moreover, through the PI3K/Akt pathway, apelin preconditioning can increase the expression of eNOS and counteract the pathological effects of the angiotensin II/angiotensin II type 1 receptor system in HIRI[43]. Thus, the activation of the PI3K/Akt pathway leads to the phosphorylation of eNOS and continuous catalysation of NO production, which is essential to counteract HIRI.
KLF2 induced eNOS activation: There may exist other ways of influencing the eNOS activity during IR. It has been proven that WIR injury can decrease the expression of KLF2 in endothelial cells. Also, this reduction is accompanied by a decrease in phosphorylated eNOS (p-eNOS), one of the KLF2 targets. And the IR damage can be mitigated by pretreatment with simvastatin through a KLF2-dependent mechanism, upregulating the mRNA expression of KLF2 and eNOS as well as the protein expression of KLF2 and p-eNOS[16,44]. Hu et al[45] also demonstrated that hypothermic machine perfusion inhibited NF-κB signaling and activated eNOS/NO signaling through KLF2 expression, thereby alleviating the inflammatory response and oxidative stress injury. It has demonstrated that KLF2 activators can be candidate therapeutic agents for HIRI.
AMPK induced eNOS activation: AMPK plays a key role in the regulation of cellular energy homeostasis. The activation of this kinase is a response to the stimulus. Mahfoudh et al[46] reported that repeated administration of trimetazidine protected against WIR injury by decreasing liver damage and oxidative stress. The underlying mechanism involves the activation of the AMPK/eNOS signaling pathway. In addition, similar mechanisms have been identified in the protective effect of Institut Georges Lopez 1 solution on cold-stored fatty liver grafts. The effect is mainly exerted through the activation of the AMPK pathway, which targets eNOS to produce NO, offsetting aggravated microcirculatory changes, and improving vascular resistance and function during IR[47,48].
Other pathways: SEW2871, a selective sphingosine-1-phosphate receptor 1 (S1PR1) agonist, can restore the expression of eNOS and vascular endothelial (VE) cadherin in sinusoidal endothelial cells during HIRI in vivo and does not influence the expression of p-Akt. Thus, there may be a regulation pathway between S1PR1 and eNOS[49]. And the expression of VE-cadherin is important for vascular integrity, which is the basis for eNOS expression[49].
Moreover, ischemia preconditioning (IPC) can protect HIRI through p38 MAPK activation, which induces eNOS-derived NO expression to enhance cell autophagy in HIRI[35]. However, pretreatment with 3,7-dimethyl-1-propargylxanthine, an adenosine A2 receptor (A2AR) antagonist, can repeal the protective effect induced by IPC. Therefore, it can be inferred that there may be a relationship between the A2AR and eNOS[50].
The study of Kebschull et al[51] showed that low-dose erythropoietin (EPO) treatment significantly increased hepatic NO bioavailability by up-regulating eNOS expression. EPO-mediated eNOS phosphorylation is promoted by EPOR-mediated activation of the Janus kinase 2/PI3K/Akt pathway and common β receptor (βcR)-dependent activation of AMPK. In addition to this, activation of the βcR2-vascular endothelial growth factor receptor-2 complex is also involved in the regulation, but its downstream signaling is currently unclear.
As mentioned above, iNOS-derived NO may have different functions in HIRI[15]. Although in most cases iNOS is considered to be harmful to the HIRI, it does not affect or even protects the HIRI in some conditions. In a study of models with liver ischemia and partial liver resection, iNOS mRNA expression was not found to be significantly altered compared to the sham group. While during 6 to 8 h after hepatectomy, iNOS expression and NO production were promoted by cytokines, thereby improving liver microcirculation and preventing cell apoptosis[52]. The protective effect of iNOS has only been demonstrated in a few specific experiments and lacks widespread validation. Due to differences in experimental subjects, measurement criteria, and experimental time constraints, iNOS-derived NO exhibits a more complex and unclear role than eNOS.
Hide et al[14] found a surge of NO in WIR in aged livers, which was mainly induced by iNOS production. The surge of NO derived from iNOS can increase the expression of reactive nitrogen species (RNS) and inflammatory cytokines, resulting in cytotoxic damage in hepatocytes. Besides, the damage from iNOS is also confirmed in other studies. As intrahepatic macrophages, KCs are activated in early IRI, producing excessive amounts of iNOS-derived NO and leading to massive production of pro-inflammatory factors, cytokines, and ROS, which are key links to impaired microcirculation in the liver and deteriorate HIRI[5,53].
At the late phase of HIRI, the function of iNOS will be at a prominent stage. Excess NO derived from iNOS has cytotoxic effects that induce inflammation and excessive oxidation, and performs many deleterious functions in HIRI. Increased iNOS expression is associated with increased TNF-α and NF-κB, which leads to increased expression of pro-inflammatory genes, inflammatory mediators, and regulatory enzymes[54]. They are both important to trigger inflammation reactions and may have deleterious effects on IRI. Besides, in studying the role of iNOS/NO in the interferon regulatory factor-1 (IRF1) signaling pathway of primary human hepatocytes, Du et al[55] found the existence of a positive-feedback loop between iNOS and IRF1. The IRF1 and p53 can upregulate the p53 up-regulated modulator of apoptosis (PUMA), which is a modulator of apoptosis, resulting in hepatocyte death and further damage to hepatic IRI.
The extent and intensity of eNOS and iNOS in HIRI are both higher than those in the normal state, while excess NO will produce peroxynitrite to aggravate IR damage. These can be reduced by using high doses of tadalafil and pentoxifylline to mitigate the deterioration of nitrosative stress and endothelial cell injury[53].
Iwasaki et al[6] demonstrated that L-NAME, an NOS inhibitor, attenuated liver damage in IRI of cholestatic livers by inhibiting the NO production. Comparing the expression of iNOS and eNOS with L-NAME treatment, they found that this kind of protection was mainly mediated by the inhibitory effects of iNOS. It also prevented the increase of asymmetric dimethylarginine, which is an exogenous inhibitor of eNOS, to protect against IRI at the early stage.
Bone marrow mesenchymal stem cell (BMMSC) transplantation can regulate NOS synthesis by increasing eNOS expression as well as inhibiting iNOS expression and excessive NO production to protect HIRI and reduce hepatocyte apoptosis. Its regulations are closely related to the inhibition of NOS-induced macrophage activation, the suppression of large amounts of iNOS and NO synthesized by macrophages, and the amelioration of endothelial damage. And the combined use of BMMSCs and normothermic machine perfusion can increase the balance of ET/NO ratio[5].
Besides, the eNOS traffic inducer (NOSTRIN) can significantly inhibit NO release by decreasing the enzymatic activity of eNOS. Pretreatment with N-acetylcysteine or thymoquinone can up-regulate eNOS along with NO production and down-regulate iNOS and NOSTRIN expression to attenuate HIRI injury, showing the protective effect of increasing eNOS and NO levels and inhibiting iNOS expression against IRI in rat liver[56].
After reperfusion, the expression of inflammatory factors such as macrophage inflammatory protein-2 and iNOS increase with the activation of NF-κB, leading to a series of inflammation reactions. Alpha-lipoic acid can reduce the formation of excess NO during reperfusion by decreasing the expression of iNOS mRNA and reduce cellular damage from NO-forming NOS superoxide and peroxide anions[57]. Beyond that, in a study of vildagliptin function in lung injury after hepatic IRI, significant inhibition of iNOS mRNA expression and NO was observed by the involvement of the hypoxia-inducible factor (HIF)-α/hepatocyte growth factor/iNOS pathway. The evaluated HIF-α can increase iNOS expression in various models. Therefore, targeting HIF-α expression can reduce tissue damage[58]. Furthermore, hepatic IR-induced iNOS protein expression can be diminished by eupatilin, which also suppresses the Toll-like receptor 2/NF-κB pathway to ameliorate inflammation response[59]. In addition, neural-sphingomyelinase (N-SMase) can produce ceramide, which is a mediator of iNOS expression. Inhibition of N-SMase leads to a decrease in iNOS levels, along with a decrease in protein nitrification and nitrite/nitrate levels in WIR[60].
Some studies have demonstrated the hepatoprotective effect of genetic eNOS overexpression in small-for-size liver transplantation and illustrated the importance of promoting eNOS expression for hepatoprotection[61]. However, there is insufficient evidence for a protective effect of eNOS overexpression, and evidence that eNOS overexpression is detrimental to HIRI[62]. The dual effect of eNOS in HIRI remains controversial.
The fact is that the expression of eNOS will be deteriorated by oxidative stress and endothelial damage during the progression of ischemia, while the function of iNOS will be stimulated by oxidative stress during reperfusion and aggravate the liver injury. The imbalance of eNOS and iNOS can also aggravate IRI.
NOS drugs as well as drugs for the regulation of NOS enzymes may be the way forward for liver protection. However, more in-depth studies are still needed. Not only do drugs need to be stable, but they also need to avoid the harm that NO and NOS can cause to reduce side effects. Besides, despite a number of experimental studies demonstrating the beneficial effects of NO-releasing compounds and some drugs that promote NO release in ameliorating hepatic IRI, the results of trials and evaluations in the clinical setting are still lacking. Perhaps more randomised controlled clinical trials should be strengthened in the future to obtain more therapeutic results.
In a nutshell, increasing or decreasing NO availability in the hepatic tissue may both be ways to prevent and treat HIRI and identifying ways to balance the expression of eNOS and iNOS is important to protect IR and can be a promising direction for clinical research.
In general, NO along with eNOS and iNOS can play complex roles in HIRI. NO can down-regulate LTC4S by inhibiting the NFκB pathway, inhibit apoptotic related genes such as Bax and Bcl-2, enhance autophagic flux, decrease inflammatory cytokines, and reduce ROS by inhibiting the mitochondrial respiratory chain. Furthermore, NO induced by different NOS results in a duality of action in HIRI. NO derived by eNOS prefers to protect endothelial cells and attenuate liver injury in HIRI. However, iNOS promotes the production of NO in response to stimuli, thus exacerbating liver damage. But their role is not set in stone. Overexpression of eNOS also worsens HIRI, whereas iNOS has also been reported to have a protective effect against HIRI. Actually, these views remain controversial, and the underlying mechanisms are urgently needed to be clarified.
Manuscript source: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pharmacology and Pharmacy
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ramadan N, Serafini S S-Editor: Chang KL L-Editor: Wang TQ P-Editor: Chang KL
| 1. | Ikeda T, Yanaga K, Kishikawa K, Kakizoe S, Shimada M, Sugimachi K. Ischemic injury in liver transplantation: difference in injury sites between warm and cold ischemia in rats. Hepatology. 1992;16:454-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 206] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 2. | Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, Jin L, Zhang T, Chen X. The trends in incidence of primary liver cancer caused by specific etiologies: Results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70:674-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 518] [Article Influence: 86.3] [Reference Citation Analysis (0)] |
| 3. | Phillips L, Toledo AH, Lopez-Neblina F, Anaya-Prado R, Toledo-Pereyra LH. Nitric oxide mechanism of protection in ischemia and reperfusion injury. J Invest Surg. 2009;22:46-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 137] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 4. | Rampes S, Ma D. Hepatic ischemia-reperfusion injury in liver transplant setting: mechanisms and protective strategies. J Biomed Res. 2019;33:221-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 5. | Yang L, Cao H, Sun D, Hou B, Lin L, Shen ZY, Song HL. Bone marrow mesenchymal stem cells combine with normothermic machine perfusion to improve rat donor liver quality-the important role of hepatic microcirculation in donation after circulatory death. Cell Tissue Res. 2020;381:239-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 6. | Iwasaki J, Afify M, Bleilevens C, Klinge U, Weiskirchen R, Steitz J, Vogt M, Yagi S, Nagai K, Uemoto S, Tolba RH. The Impact of a Nitric Oxide Synthase Inhibitor (L-NAME) on Ischemia⁻Reperfusion Injury of Cholestatic Livers by Pringle Maneuver and Liver Resection after Bile Duct Ligation in Rats. Int J Mol Sci. 2019;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Donnarumma E, Ali MJ, Rushing AM, Scarborough AL, Bradley JM, Organ CL, Islam KN, Polhemus DJ, Evangelista S, Cirino G, Jenkins JS, Patel RA, Lefer DJ, Goodchild TT. Zofenopril Protects Against Myocardial Ischemia-Reperfusion Injury by Increasing Nitric Oxide and Hydrogen Sulfide Bioavailability. J Am Heart Assoc. 2016;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 60] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 8. | Kim JS, Ohshima S, Pediaditakis P, Lemasters JJ. Nitric oxide protects rat hepatocytes against reperfusion injury mediated by the mitochondrial permeability transition. Hepatology. 2004;39:1533-1543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 81] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Hara Y, Teramoto K, Kumashiro Y, Sato E, Nakamura N, Takatsu S, Kawamura T, Arii S. Beneficial effect of tetrahydrobiopterin on the survival of rats exposed to hepatic ischemia-reperfusion injury. Transplant Proc. 2005;37:442-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Hibbs JB Jr, Taintor RR, Vavrin Z, Rachlin EM. Nitric oxide: a cytotoxic activated macrophage effector molecule. Biochem Biophys Res Commun. 1988;157:87-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1461] [Cited by in RCA: 1400] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 11. | Zhang YQ, Ding N, Zeng YF, Xiang YY, Yang MW, Hong FF, Yang SL. New progress in roles of nitric oxide during hepatic ischemia reperfusion injury. World J Gastroenterol. 2017;23:2505-2510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Crane BR, Arvai AS, Ghosh DK, Wu C, Getzoff ED, Stuehr DJ, Tainer JA. Structure of nitric oxide synthase oxygenase dimer with pterin and substrate. Science. 1998;279:2121-2126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 551] [Cited by in RCA: 515] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 13. | Förstermann U, Sessa WC. Nitric oxide synthases: regulation and function. Eur Heart J. 2012;33:829-837, 837a. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2678] [Cited by in RCA: 2901] [Article Influence: 223.2] [Reference Citation Analysis (0)] |
| 14. | Hide D, Warren A, Fernández-Iglesias A, Maeso-Díaz R, Peralta C, Le Couteur DG, Bosch J, Cogger VC, Gracia-Sancho J. Ischemia/Reperfusion Injury in the Aged Liver: The Importance of the Sinusoidal Endothelium in Developing Therapeutic Strategies for the Elderly. J Gerontol A Biol Sci Med Sci. 2020;75:268-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Abu-Amara M, Yang SY, Seifalian A, Davidson B, Fuller B. The nitric oxide pathway--evidence and mechanisms for protection against liver ischaemia reperfusion injury. Liver Int. 2012;32:531-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 16. | Hide D, Ortega-Ribera M, Garcia-Pagan JC, Peralta C, Bosch J, Gracia-Sancho J. Effects of warm ischemia and reperfusion on the liver microcirculatory phenotype of rats: underlying mechanisms and pharmacological therapy. Sci Rep. 2016;6:22107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | El-Gohary OA. Obestatin improves hepatic injury induced by ischemia/reperfusion in rats: Role of nitric oxide. Gen Physiol Biophys. 2017;36:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Cavalieri B, Perrelli MG, Aragno M, Ramadori P, Poli G, Cutrìn JC. Ischaemic preconditioning modulates the activity of Kupffer cells during in vivo reperfusion injury of rat liver. Cell Biochem Funct. 2003;21:299-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Matuschak GM, Henry KA, Johanns CA, Lechner AJ. Liver-lung interactions following Escherichia coli bacteremic sepsis and secondary hepatic ischemia/reperfusion injury. Am J Respir Crit Care Med. 2001;163:1002-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Hong FF, Wang YF, Liu H, Yang MW, Yang SL. V-PYRRO/NO downregulates mRNA expression levels of leukotriene C4 synthase during hepatic ischemia reperfusion injury in rats via inhibition of the nuclear factor-κB activation pathway. Biomed Rep. 2016;4:112-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Zhao P, Sun X, Chaggan C, Liao Z, In Wong K, He F, Singh S, Loomba R, Karin M, Witztum JL, Saltiel AR. An AMPK-caspase-6 axis controls liver damage in nonalcoholic steatohepatitis. Science. 2020;367:652-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 231] [Article Influence: 46.2] [Reference Citation Analysis (0)] |
| 22. | Gao D, Xu Z, Qiao P, Liu S, Zhang L, He P, Zhang X, Wang Y, Min W. Cadmium induces liver cell apoptosis through caspase-3A activation in purse red common carp (Cyprinus carpio). PLoS One. 2013;8:e83423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 23. | Zhang R, Yi R, Bi Y, Xing L, Bao J, Li J. The Effect of Selenium on the Cd-Induced Apoptosis via NO-Mediated Mitochondrial Apoptosis Pathway in Chicken Liver. Biol Trace Elem Res. 2017;178:310-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 24. | Abdel Moneim AE. Indigofera oblongifolia Prevents Lead Acetate-Induced Hepatotoxicity, Oxidative Stress, Fibrosis and Apoptosis in Rats. PLoS One. 2016;11:e0158965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 111] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 25. | Fouad AA, Qutub HO, Al-Melhim WN. Punicalagin alleviates hepatotoxicity in rats challenged with cyclophosphamide. Environ Toxicol Pharmacol. 2016;45:158-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 26. | Zhao J, Liu T, Ma L, Yan M, Zhao Y, Gu Z, Huang Y. Protective effect of acteoside on immunological liver injury induced by Bacillus Calmette-Guerin plus lipopolysaccharide. Planta Med. 2009;75:1463-1469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Yang T, Wu J, Wang C, Liu Q, Ma X, Peng J, Kaku T, Liu K. Protective effect of JBP485 on concanavalin A-induced liver injury in mice. J Pharm Pharmacol. 2009;61:767-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 28. | Chen KH, Lin BR, Chien CT, Ho CH. Emblica officinalis Gaertn. attentuates N-nitrosodiethylamine-induced apoptosis, autophagy, and inflammation in rat livers. J Med Food. 2011;14:746-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Tsuchihashi S, Kaldas F, Chida N, Sudo Y, Tamura K, Zhai Y, Qiao B, Busuttil RW, Kupiec-Weglinski JW. FK330, a novel inducible nitric oxide synthase inhibitor, prevents ischemia and reperfusion injury in rat liver transplantation. Am J Transplant. 2006;6:2013-2022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Lin X, Zhang S, Huang R, Tan S, Liang S, Wu X, Zhuo L, Huang Q. Protective effect of tormentic acid from Potentilla chinensis against lipopolysaccharide/D-galactosamine induced fulminant hepatic failure in mice. Int Immunopharmacol. 2014;19:365-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 31. | Zhao Y, Zhou P, Liu B, Bambakidis T, Mazitschek R, Alam HB, Li Y. Protective effect of suberoylanilide hydroxamic acid against lipopolysaccharide-induced liver damage in rodents. J Surg Res. 2015;194:544-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Yang BY, Zhang XY, Guan SW, Hua ZC. Protective Effect of Procyanidin B2 against CCl4-Induced Acute Liver Injury in Mice. Molecules. 2015;20:12250-12265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 33. | Sherif IO, Al-Shaalan NH. Vildagliptin Attenuates Hepatic Ischemia/Reperfusion Injury via the TLR4/NF-κB Signaling Pathway. Oxid Med Cell Longev. 2018;2018:3509091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 65] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 34. | Jiang Q, Pan Y, Cheng Y, Li H. Protection of rat liver against hepatic ischemia-reperfusion injury by a novel selenocysteine-containing 7-mer peptide. Mol Med Rep. 2016;14:2007-2015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Shin JK, Kang JW, Lee SM. Enhanced nitric oxide-mediated autophagy contributes to the hepatoprotective effects of ischemic preconditioning during ischemia and reperfusion. Nitric Oxide. 2016;58:10-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 36. | Gracia-Sancho J, García-Calderó H, Hide D, Marrone G, Guixé-Muntet S, Peralta C, García-Pagán JC, Abraldes JG, Bosch J. Simvastatin maintains function and viability of steatotic rat livers procured for transplantation. J Hepatol. 2013;58:1140-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 37. | Rodríguez-Reynoso S, Leal-Cortés C, Portilla-de Buen E, López-De la Torre SP. Ischemic Preconditioning Preserves Liver Energy Charge and Function on Hepatic Ischemia/Reperfusion Injury in Rats. Arch Med Res. 2018;49:373-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 38. | Ragy MM, Aziz NM. Prevention of renal ischemia/perfusion-induced renal and hepatic injury in adult male Albino rats by oxytocin: role of nitric oxide. J Basic Clin Physiol Pharmacol. 2017;28:615-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 39. | Michel JB, Feron O, Sacks D, Michel T. Reciprocal regulation of endothelial nitric-oxide synthase by Ca2+-calmodulin and caveolin. J Biol Chem. 1997;272:15583-15586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 441] [Cited by in RCA: 435] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 40. | Fleming I, Busse R. Molecular mechanisms involved in the regulation of the endothelial nitric oxide synthase. Am J Physiol Regul Integr Comp Physiol. 2003;284:R1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 584] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 41. | Nakazato PCG, Victorino JP, Fina CF, Mendes KDS, Gomes MCJ, Evora PRB, D'Albuquerque LAC, Castro-E-Silva O. Liver ischemia and reperfusion injury. Pathophysiology and new horizons in preconditioning and therapy. Acta Cir Bras. 2018;33:723-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 42. | Rabie MA, Zaki HF, Sayed HM. Telluric acid ameliorates hepatic ischemia reperfusion-induced injury in rats: Involvement of TLR4, Nrf2, and PI3K/Akt signaling pathways. Biochem Pharmacol. 2019;168:404-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 43. | Sabry MM, Ramadan NM, Al Dreny BA, Rashed LA, Abo El Enein A. Protective effect of apelin preconditioning in a rat model of hepatic ischemia reperfusion injury; possible interaction between the apelin/APJ system, Ang II/AT1R system and eNOS. United European Gastroenterol J. 2019;7:689-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 44. | Liu Z, Lai CH, Zhang X, Luo J, Huang X, Qi X, Wang W, Zhong Z, Xiaoli F, Li L, Xiong Y, Senninger N, Wang Y, Ye Q, Ye S. Simvastatin ameliorates total liver ischemia/reperfusion injury via KLF2-mediated mechanism in rats. Clin Res Hepatol Gastroenterol. 2019;43:171-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 45. | Hu X, Wang W, Zeng C, He W, Zhong Z, Liu Z, Wang Y, Ye Q. Appropriate timing for hypothermic machine perfusion to preserve livers donated after circulatory death. Mol Med Rep. 2020;22:2003-2011. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 46. | Mahfoudh Boussaid A, Selmi R, Bejaoui M, Hadj Ayed K, Zaouali MA, Ben Abdennebi H. Effectiveness of a single vs repeated administration of trimetazidine in the protection against warm ischemia/reperfusion injury of rat liver. Turk J Med Sci. 2016;46:1258-1264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 47. | Panisello Rosello A, Teixeira da Silva R, Castro C, G Bardallo R, Calvo M, Folch-Puy E, Carbonell T, Palmeira C, Roselló Catafau J, Adam R. Polyethylene Glycol 35 as a Perfusate Additive for Mitochondrial and Glycocalyx Protection in HOPE Liver Preservation. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 48. | Panisello-Roselló A, Verde E, Amine Zaouali M, Flores M, Alva N, Lopez A, Folch-Puy E, Carbonell T, Hotter G, Adam R, Roselló-Catafau J. The Relevance of the UPS in Fatty Liver Graft Preservation: A New Approach for IGL-1 and HTK Solutions. Int J Mol Sci. 2017;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 49. | Ito T, Kuriyama N, Kato H, Matsuda A, Mizuno S, Usui M, Sakurai H, Isaji S. Sinusoidal protection by sphingosine-1-phosphate receptor 1 agonist in liver ischemia-reperfusion injury. J Surg Res. 2018;222:139-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 50. | Robertson FP, Fuller BJ, Davidson BR. An Evaluation of Ischaemic Preconditioning as a Method of Reducing Ischaemia Reperfusion Injury in Liver Surgery and Transplantation. J Clin Med. 2017;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 51. | Kebschull L, Theilmann LFC, Mohr A, Uennigmann W, Stoeppeler S, Heitplatz B, Spiegel HU, Bahde R, Palmes DM, Becker F. EPOR2/βcR2-independendent effects of low-dose epoetin-α in porcine liver transplantation. Biosci Rep. 2017;37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 52. | Athanasopoulos P, Mastoraki A, Papalois A, Nastos C, Kondi-Pafiti A, Kostopanagiotou G, Smyrniotis V, Arkadopoulos N. Expression of Inflammatory and Regenerative Genes in a Model of Liver Ischemia/Reperfusion and Partial Hepatectomy. J Invest Surg. 2016;29:67-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 53. | Bektas S, Karakaya K, Can M, Bahadir B, Guven B, Erdogan N, Ozdamar SO. The effects of tadalafil and pentoxifylline on apoptosis and nitric oxide synthase in liver ischemia/reperfusion injury. Kaohsiung J Med Sci. 2016;32:339-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 54. | Atef Y, El-Fayoumi HM, Abdel-Mottaleb Y, Mahmoud MF. Effect of cardamonin on hepatic ischemia reperfusion induced in rats: Role of nitric oxide. Eur J Pharmacol. 2017;815:446-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 55. | Du Q, Luo J, Yang MQ, Liu Q, Heres C, Yan YH, Stolz D, Geller DA. iNOS/NO is required for IRF1 activation in response to liver ischemia-reperfusion in mice. Mol Med. 2020;26:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 56. | Ren Y, Wang LH, Deng FS, Li JS, Jiang L. Protective effect and mechanism of alpha-lipoic acid on partial hepatic ischemia-reperfusion injury in adult male rats. Physiol Res. 2019;68:739-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 57. | Sherif IO, Al-Shaalan NH. Alleviation of remote lung injury following liver ischemia/reperfusion: Possible protective role of vildagliptin. Int Immunopharmacol. 2021;91:107305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 58. | Lee HM, Jang HJ, Kim SS, Kim HJ, Lee SY, Oh MY, Kwan HC, Jang DS, Eom DW. Protective Effect of Eupatilin Pretreatment Against Hepatic Ischemia-Reperfusion Injury in Mice. Transplant Proc. 2016;48:1226-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 59. | Unal B, Ozcan F, Tuzcu H, Kırac E, Elpek GO, Aslan M. Inhibition of neutral sphingomyelinase decreases elevated levels of nitrative and oxidative stress markers in liver ischemia-reperfusion injury. Redox Rep. 2017;22:147-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 60. | Abd-Elbaset M, Arafa EA, El Sherbiny GA, Abdel-Bakky MS, Elgendy AN. Thymoquinone mitigate ischemia-reperfusion-induced liver injury in rats: a pivotal role of nitric oxide signaling pathway. Naunyn Schmiedebergs Arch Pharmacol. 2017;390:69-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 61. | Zhang B, Liu QH, Zhou CJ, Hu MZ, Qian HX. Protective effect of eNOS overexpression against ischemia/reperfusion injury in small-for-size liver transplantation. Exp Ther Med. 2016;12:3181-3188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 62. | Palanisamy AP, Cheng G, Sutter AG, Liu J, Lewin DN, Chao J, Chavin K. Adenovirus-mediated eNOS expression augments liver injury after ischemia/reperfusion in mice. PLoS One. 2014;9:e93304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |