Published online Feb 27, 2022. doi: 10.4254/wjh.v14.i2.400
Peer-review started: June 29, 2021
First decision: July 27, 2021
Revised: August 8, 2021
Accepted: February 10, 2022
Article in press: February 10, 2022
Published online: February 27, 2022
Processing time: 238 Days and 7.6 Hours
Takotsubo cardiomyopathy (TCM), or stress-induced cardiomyopathy, is associated with adverse prognosis. Limited data suggest that TCM occurring in orthotopic liver transplant (OLT) recipients is associated with elevated peri-operative risk.
To characterize the predictors of TCM in OLT recipients, using a large, multi-center pooled electronic health database.
A multi-institutional database (Explorys Inc, Cleveland, OH, USA), an aggregate of de-identified electronic health record data from 26 United States healthcare systems was surveyed. A cohort of patients with a Systematized Nomenclature of Medicine-Clinical Terms of “liver transplant” between 09/2015 and 09/2020 was identified. Subsequently, individuals who developed a new diagnosis of TCM following OLT were identified. Furthermore, the risk associations with TCM among this patient population were characterized using linear regression.
Between 09/2015 and 09/2020, of 37718540 patients in the database, 38740 (0.10%) had a history of OLT (60.6% had an age between 18-65 years, 58.1% female). A new diagnosis of TCM was identified in 0.3% of OLT recipients (45.5% had an age between 18-65 years, 72.7% female), compared to 0.04% in non-OLT patients [odds ratio (OR): 7.98, 95% confidence intervals: 6.62-9.63, (P < 0.0001)]. OLT recipients who developed TCM, compared to those who did not, were more likely to be greater than 65 years of age, Caucasian, and female (P < 0.05). There was also a significant association with cardiac arrhythmias, especially ventricular arrhythmias (P < 0.0001).
TCM was significantly more likely to occur in LT recipients vs non-recipients. Older age, Caucasian ethnicity, female gender, and presence of arrhythmias were significantly associated with TCM in LT recipients.
Core Tip: In a large cohort study using de-identified pooled electronic health record data, liver transplant recipients were more likely to develop Takotsubo cardiomyopathy compared to non-recipients. Older age, Caucasian ethnicity, female gender, and presence of arrhythmias were significantly associated with Takotsubo cardiomyopathy in liver transplant recipients.
- Citation: Zmaili M, Alzubi J, Alkhayyat M, Cohen J, Alkharabsheh S, Rana M, Alvarez PA, Mansoor E, Xu B. Takotsubo cardiomyopathy in orthotopic liver transplant recipients: A cohort study using multi-center pooled electronic health record data. World J Hepatol 2022; 14(2): 400-410
- URL: https://www.wjgnet.com/1948-5182/full/v14/i2/400.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i2.400
Takotsubo cardiomyopathy (TCM) is a stress-induced, reversible cardiomyopathy that occurs in the absence of significant coronary artery disease[1]. The awareness of TCM, which was first reported in Japan in 1990, has increased rapidly and several nomenclatures for this condition have been proposed including stress-induced cardiomyopathy, apical ballooning syndrome, left ventricular ballooning, and broken heart syndrome[2,3]. TCM is believed to be related to the presence of an underlying pathological stress, whether physical or emotional[1]. Despite the enormous attention that this condition has gained in recent years, TCM is still considered to be underdiagnosed, with an underestimated risk and incompletely understood pathogenesis[4].
It is hypothesized that emotional or physical stress may trigger a surge in catecholamine secretion, which in turn can lead to microvascular spasms and myocardial stunning via interaction with beta-adrenergic receptors, resulting in left ventricular systolic dysfunction[5]. Patients undergoing major surgery often have increased concentrations of catecholamines, caused by the physical and emotional stress of the perioperative period, which can contribute to the development of TCM[6]. Although TCM is self-limited and resolves completely without an adverse event in the majority of affected patients, it may result in significant morbidity and mortality in critically ill patients, such as liver transplant recipients, with estimated mortality rate of 10%-27%[7].
Small observational studies and case series have reported the occurrence of TCM in liver transplant recipients, but large cohort studies evaluating this association are lacking in the literature[6]. In addition to the stress imposed by the perioperative period, liver transplant candidates are particularly vulnerable to developing TCM due to the impaired stress response in the inflammatory milieu of hepatic cirrhosis[8,9]. Therefore, we aimed to study TCM in liver transplant recipients, providing information about the demographic characteristics of these patients, and delineating this unique patient population’s risk factors for TCM.
We conducted a retrospective, cohort study using a multicenter analytics and research platform developed by IBM Watson Health (Explorys Inc, Cleveland, OH, USA)[10]. At present, Explorys captures more than 70 million unique patients across all 50 states, and thus provides a broad regional and climatic distribution of source population. Diagnoses, findings, and procedures are arranged into the Systematized Nomenclature of Medicine - Clinical Terms (SNOMED-CT) hierarchy while prescription drug orders are mapped into SNOMED and RxNorm[11,12]. Patients with all types of insurance as well as those who self-pay are represented. Ethical review and informed consent were waived, since there are no identifiers associated with any of the patient data. The Explorys rounds cell counts to the nearest 10 and treats all cell counts between zero and 10 as equivalent in order to protect the identities of patients. The Explorys database has been used in multiple publications in gastroenterology, cardiology, oncology, neurology, and surgery[13,14].
Using the Explorys search tool, we identified all active patients in Explorys between 09/2015 and 09/2020 and selected those who underwent liver transplantation. Subsequently, a cohort of patients with a SNOMET-CT diagnosis of “takotsubo cardiomyopathy” was identified. Cases were compared to those who underwent liver transplantation without a history of TCM. Using SNOMED-CT codes, we identified possible associated medical conditions as well as disease outcomes.
Demographics and associated diseases were characterized by descriptive statistics. The overall period prevalence was calculated by dividing the total number of individuals with TCM by the total number of individuals in Explorys who underwent liver transplantation (2015-2020). The odds ratio (OR) for univariate analysis, its standard error and 95% confidence intervals (CI) were calculated according to Altman, 1991, using the MedCalc Statistical Software for Windows, version 19.4 (MedCalc Software, Ostend, Belgium) with a case-control design[15]. For all analyses, a 2-sided P value of <0.05 was considered statistically significant.
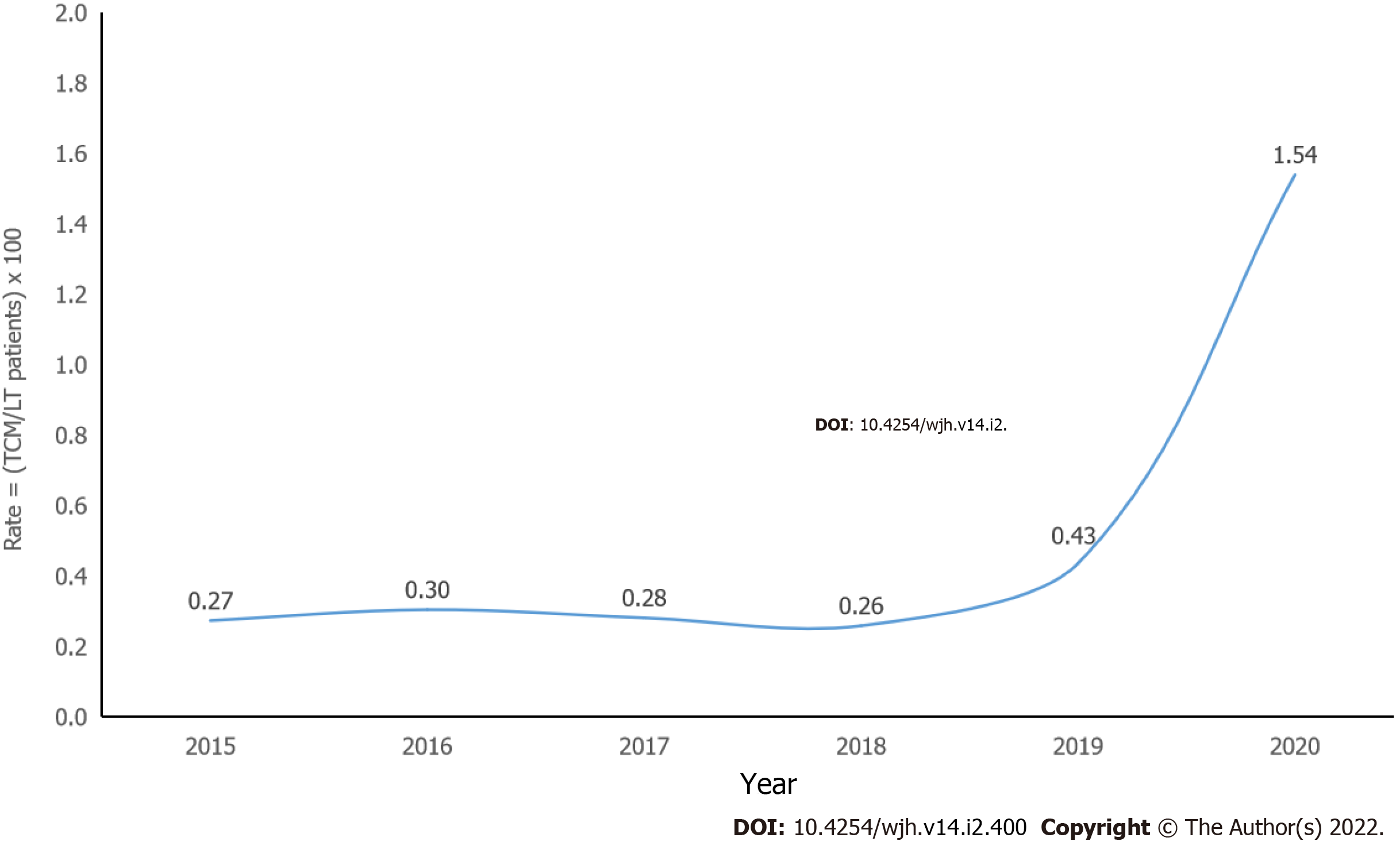
There were a total of 37718540 individuals in the database (2015-2020) with 38,740 (0.1%) who underwent liver transplantation. Baseline characteristics of patients with liver transplant and control groups are demonstrated in Table 1. The majority of patient who underwent OLT were adults (18-65 years old), female (58.1%), and Caucasian (77.8%). Among those who underwent liver transplantation, there were 110 patients with a diagnosis of TCM with a period prevalence rate of 0.3%. Rates of TCM among OLT patients and timing of diagnosis are shown in Figures 1 and 2, respectively.
| Liver transplant | No liver transplant | |||
| n = 38740 | % | n = 37679800 | % | |
| Takotsubo cardiomyopathy | 110 | 0.3 | 13430 | 0.0 |
| Age > 65 | 14780 | 38.2 | 8349380 | 22.2 |
| Age 18-65 | 23470 | 60.6 | 22449470 | 59.6 |
| Age < 18 | 500 | 1.3 | 6659540 | 17.7 |
| Male | 16230 | 41.9 | 16676780 | 44.3 |
| Female | 22510 | 58.1 | 20665100 | 54.8 |
| Caucasian | 30150 | 77.8 | 22446830 | 59.6 |
| African American | 6060 | 15.6 | 4315410 | 11.5 |
| Obesity | 840 | 2.2 | 5018440 | 13.3 |
| Cardiomyopathy | 1770 | 4.6 | 762420 | 2.0 |
| Hypertension | 390 | 1.0 | 3465120 | 9.2 |
| Diabetes Mellitus | 710 | 1.8 | 5484800 | 14.6 |
| Hyperlipidemia | 1220 | 3.1 | 10758820 | 28.6 |
| Atherosclerosis | 770 | 2.0 | 3848890 | 10.2 |
| Coronary artery disease | 730 | 1.9 | 3395870 | 9.0 |
| Myocardial infarction | 430 | 1.1 | 1528310 | 4.1 |
| Ischemic heart disease | 620 | 1.6 | 2285770 | 6.1 |
| Chronic kidney disease | 530 | 1.4 | 2052700 | 5.4 |
| Alcohol abuse | 80 | 0.2 | 1013590 | 2.7 |
| Smoking | 290 | 0.7 | 6369120 | 16.9 |
| Sepsis | 690 | 1.8 | 2101780 | 5.6 |
| Atrial fibrillation | 1030 | 2.7 | 2659760 | 7.1 |
| Supraventricular arrhythmia | 200 | 0.5 | 75580 | 0.2 |
| Ventricular arrhythmia | 590 | 1.5 | 415060 | 1.1 |
Interval epidemiology and underlying associations of Takotsubo cardiomyopathy in OLT.
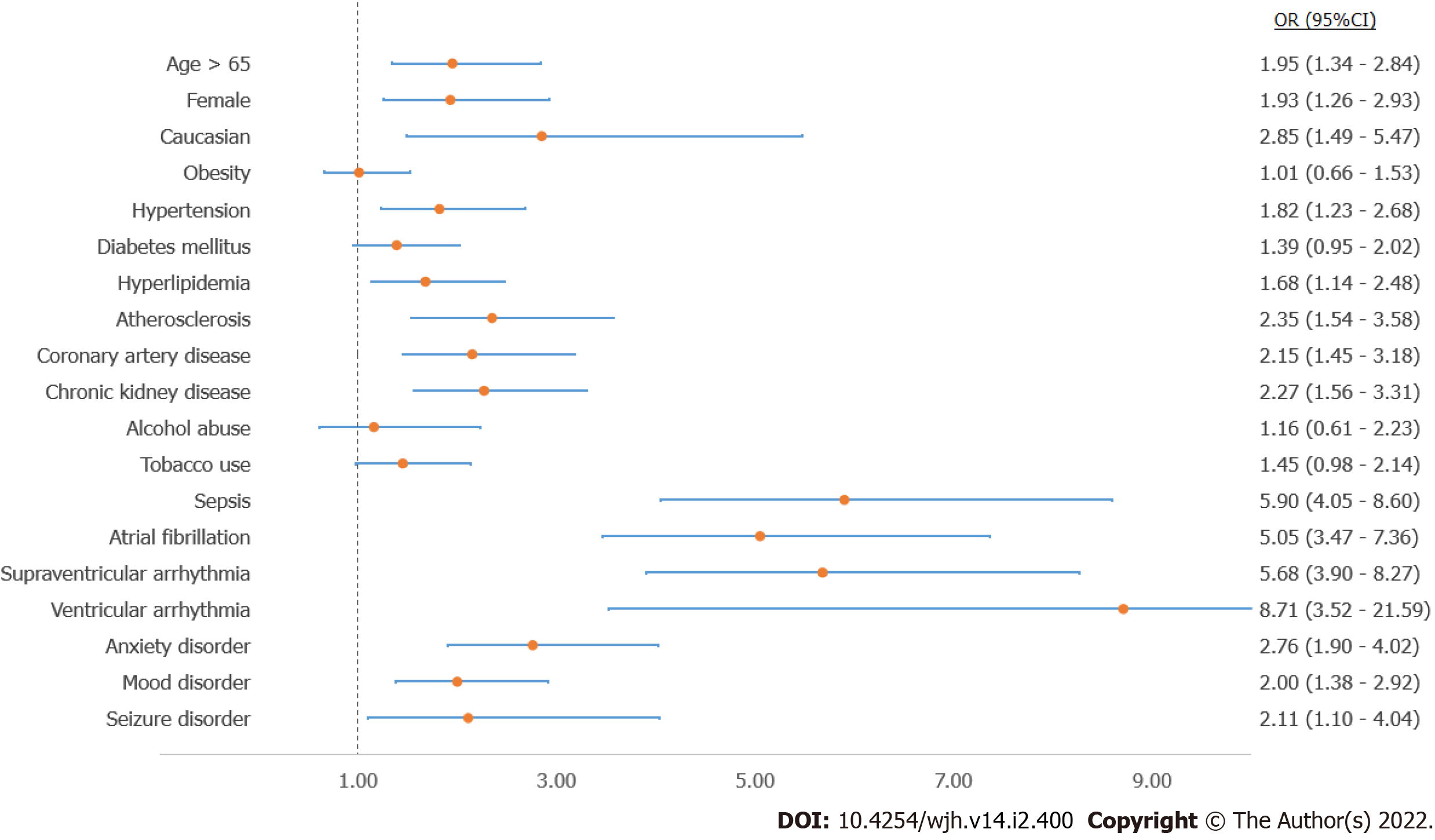
Of the 110 patients with the diagnosis of TCM, the majority were elderly (> 65 years old) (54.5%), female (72.7%), and Caucasian (90.9%) (Table 2). Patients with a diagnosis of TCM were more likely to have other medical diseases including hypertension (OR: 1.82, 95%CIs: 1.23-2.68, P = 0.0027), hyperlipidemia (OR: 1.68, 95%CIs: 1.14-2.48, P = 0.009), atherosclerosis (OR: 2.35, 95%CIs: 1.54-3.58, P = 0.0001), coronary artery disease (OR: 2.15, 95%CIs: 1.45-3.18, P = 0.0001), chronic kidney disease (OR: 2.27, 95%CIs: 1.56-3.31, P < 0.0001), sepsis (OR: 5.90, 95%CIs: 4.05-8.60, P < 0.0001), anxiety (OR: 2.76, 95%CIs: 1.90-4.02, P < 0.0001), and mood disorders (OR: 2.00, 95%CIs: 1.38-2.92, P = 0.0003) (Figure 3).
| Takotsubo cardiomyopathy | No takotsubo cardiomyopathy | P value | |||
| n = 110 | % | n = 38640 | % | ||
| Age > 65 | 60 | 54.5 | 14720 | 38.1 | 0.0005 |
| Age 18-65 | 50 | 45.5 | 23400 | 60.6 | 0.0014 |
| Age < 18 | 0 | 0.0 | 500 | 1.3 | |
| Male | 30 | 27.3 | 16200 | 41.9 | 0.0022 |
| Female | 80 | 72.7 | 22440 | 58.1 | 0.0022 |
| Caucasian | 100 | 90.9 | 30060 | 77.8 | 0.0016 |
| African American | 5 | 4.5 | 6060 | 15.7 | 0.0042 |
| Obesity | 30 | 27.3 | 10500 | 27.2 | 0.9814 |
| Hypertension | 40 | 36.4 | 9250 | 23.9 | 0.0027 |
| Diabetes mellitus | 60 | 54.5 | 17910 | 46.4 | 0.0867 |
| Hyperlipidemia | 70 | 63.6 | 19720 | 51.0 | 0.009 |
| Atherosclerosis | 30 | 27.3 | 5320 | 13.8 | 0.0001 |
| Coronary artery disease | 50 | 45.5 | 12280 | 31.8 | 0.0001 |
| Chronic kidney disease | 60 | 54.5 | 13350 | 34.5 | < 0.0001 |
| Alcohol abuse | 10 | 9.1 | 3060 | 7.9 | 0.6499 |
| Smoking | 40 | 36.4 | 10930 | 28.3 | 0.0621 |
| Sepsis | 60 | 54.5 | 6530 | 16.9 | < 0.0001 |
| Atrial fibrillation | 50 | 45.5 | 5470 | 14.2 | < 0.0001 |
| Supraventricular arrhythmia | 60 | 54.5 | 6740 | 17.4 | < 0.0001 |
| Ventricular arrhythmia | 5 | 4.5 | 210 | 0.5 | < 0.0001 |
| Anxiety disorder | 60 | 54.5 | 11700 | 30.3 | < 0.0001 |
| Mood disorder | 60 | 54.5 | 14470 | 37.4 | 0.0003 |
| Seizure disorder | 10 | 9.1 | 1750 | 4.5 | 0.025 |
Outcomes of Takotsubo cardiomyopathy among patients with OLT.
Among patients with a history of OLT, patients who were diagnosed with TCM were more likely to have cardiogenic shock (OR: 12.61, 95%CIs: 6.52-24.4, P < 0.0001), and to require mechanical circulatory support with an intra-aortic balloon bump (OR: 19.22, 95%CIs: 7.66-48.21, P < 0.0001). These patients were also at a higher risk of developing cardiac arrest (OR: 9.52, 95%CIs: 5.84-15.52, P < 0.0001). Other complications include cerebrovascular accidents, liver failure, gastrointestinal bleeding, and an increased requirement of invasive mechanical ventilation and renal replacement therapy (Figure 4).
The diagnosis of end-stage liver disease (ESLD) carries a poor prognosis and is associated with increased cardiovascular risk[16]. It is well-known that orthotopic liver transplantation (OLT) is the treatment of choice for patients with irreversible ESLD due to the improved survival after transplantation[17]. Nowadays, with the high prevalence of ESLD, increasing numbers of patients are being referred for OLT[18,19]. Although OLT improves the survival of ESLD patients, post-operative complications that affect the outcomes and survival of this patient group may occur, including cardiac complications, such as TCM[6,20]. As such, it is imperative to perform careful preoperative cardiac risk evaluation prior to the transplantation[21].
The current study is the first national database study to assess the association between liver transplantation and the development of TCM. There are several important findings in this retrospective observational study. We found that liver transplant recipients were more likely to develop TCM compared to non-recipients. It is conceivable that OLT predisposes to TCM from a pathophysiologic standpoint, given the increased levels of stress, and thus, a higher catecholamine surge around the time of liver transplant surgery.
On further analysis of OLT subgroup based on occurrence of TCM, we found that the group of patients who developed TCM were more likely to be female, Caucasian, and elderly. This is consistent with prior epidemiological and clinical studies[22-24]. In a retrospective observational study that looked at various co-morbidities, it was found that patients with certain co-morbid conditions were more likely to have concurrent TCM, compared with age-matched control groups[25]. In that study, it was reported that sepsis, cerebrovascular accident, malignancy, and anxiety disorder increased the risk of TCM with an OR 13.94 (95%CI: 11.69-16.62), 10.81 (95%CI: 8.70-13.43), 1.73 (95%CI: 1.63-1.83), and 2.54 (95%CI: 2.34-2.75), respectively. Patients who developed TCM in our study were also more likely to have chronic medical conditions, which may have possibly predisposed them to this condition via coronary microcirculatory dysfunction, one of the mechanisms that was proposed as a contributor in the pathogenesis of TCM[26]. Importantly, patients who developed TCM were found to have higher rates of arrhythmias, including those of atrial and ventricular origin, which is an important finding, and may contribute to higher morbidity and mortality in this group of patients[27,28]. It is well-known that infection and critical illness are associated with development of TCM, which may explain the finding of a higher association with sepsis in our TCM cohort[29-31]. Nonetheless, it is unclear whether sepsis preceded the occurrence of TCM, given the limitations of the database utilized in this study.
Furthermore, we found an increasing prevalence of TCM in our studied population of OLT recipients between 2015 and 2020. This higher event rate may be attributed to the increasing numbers of patients undergoing OLT, and perhaps more importantly, better recognition and improved diagnosis of the syndrome. Additionally, data from observational studies reported that coronavirus disease 2019 (COVID-19) pandemic, which started in early 2020, may have contributed to the higher incidence of TCM[32-34]. The increased incidence was seen in both the general population and COVID-19 patients, which was linked to increased psychological distress as well as heightened sympathetic responses, cytokine storm, and microvascular dysfunction seen in COVID-19 patients[32]. The adverse effects on mental health may be consequences of social distancing, economic worry, and fear of contracting the virus, among other concerns. The association between COVID-19 and TCM may be explained by potential pathophysiological links between the two conditions. Though these direct connections are not fully understood, different mechanisms were proposed for this association. First, the heightened release of pro-inflammatory cytokines and chemokines seen in some COVID-19 patients can trigger myocardial injury that may lead to TCM[35]. Second, the increased sympathetic nervous system activity, noted in some COVID-19 patients, may result in a catecholamine-induced myocardial stunning, and subsequently stress-induced cardiomyopathy[36]. Last, microvascular dysfunction has been reported in some cases of COVID-19 infection and was attributed to virus-induced systemic inflammatory response and coagulopathy. This microvascular dysfunction has been proposed as a potential mechanism for COVID-associated TCM[37]. Previous reports have shown that patients with COVID-19 infection may demonstrate various histopathological findings on postmortem examinations, including but not limited to, myocyte necrosis, inflammatory cell infiltration, lymphocytic or eosinophilic myocarditis, among others[38]. Whether these findings are associated with, or increase the risk of, developing TCM remains largely unknown.
Another key finding in our study was that patients who developed TCM had significantly higher rates of life-threatening complications and adverse events, including cardiogenic shock, ventricular arrhythmias, cardiac arrest, respiratory failure requiring invasive mechanical ventilation, acute kidney injury requiring renal replacement therapy, as well as ischemic cerebrovascular accidents. These findings are consistent with prior reports of increased in-hospital complications among patients who developed TCM[1,39-41]. Nonetheless, the observed differences in baseline comorbidities between the two study groups of OLT recipients could also represent a driving factor for the higher in-hospital morbidity and adverse events presenting in patients who developed TCM. Regardless of the exact etiology and pathogenesis, recognition of TCM as a potential postoperative complication in OLT recipients is pivotal, given its implications on patient outcomes with higher rates of in-hospital complications. Prior studies showed that despite a better recognition of the syndrome, short-term mortality rates remained relatively high[1].
There are several limitations to the current study due to the nature and well‐described shortcomings of database studies. First, there is an inability to verify the accuracy of diagnoses or outcomes with potential errors in coding of diseases or procedures. Second, the database does not capture variables related to the severity of TCM (e.g., left ventricular ejection fraction), cardiac-imaging data, use of antithrombotic agents or inotropes, and long-term outcomes. As the database also does not provide information regarding the temporal relationship between diagnoses, it is not possible to reliably distinguish in-hospital complications from comorbidities using this database. Third, owing to the observational nature, our study is subject to traditional biases, such as selection bias. Moreover, the differences reported during comparison of outcomes are subject to residual confounding. Fourth, the lack of follow-up data of patients limited our ability to report outcomes after hospital discharge for patients who developed TCM following OLT.
In conclusion, in this large, multicenter retrospective analysis of OLT recipients, transplant recipients had a higher rate of TCM occurrence compared to the general population. The majority of patients who developed TCM following OLT had higher rates of in-hospital complications, including cardiogenic shock, respiratory failure, ventricular arrhythmias, and the need for renal replacement therapy. Hence, TCM development among OLT patients contributes to significant patient morbidity and resource utilization. Multicenter, prospective studies focusing on risk factors and predictors of TCM in OLT recipients are required, in order to fully explore the factors responsible for this disease association and confirm the various outcomes observed in this patient population.
Orthotopic liver transplant recipients are a particularly vulnerable patient population with an elevated risk of developing various complications. Takotsubo cardiomyopathy (TCM) is one of the complications that is thought to have an association with liver transplantation, and can impact the overall prognosis.
Limited data is available regarding the association between orthotopic liver transplantation and TCM. The current research study evaluated this proposed association, and investigated the predictors and outcomes in this specific patient population.
To study the association between orthotopic liver transplantation and TCM, provide details about the demographic characteristics of the patient cohort, and examine the factors that affect the development of TCM in liver transplant patients, with a focus on identifying predictive variables and associated outcomes.
Using a multi-center database of de-identified electronic health record data, a cohort of patients who underwent orthotopic liver transplant during the study period was identified. The sample was investigated to reveal the subset of patients who developed TCM. The data was analyzed to evaluate the association of TCM and liver transplantation, and descriptive statistical methods were utilized to demonstrate the specific features pertaining to the cohort of interest.
The study revealed that TCM is more likely to develop in liver transplant recipients compared to non-recipients. Predictors for the development of this association are described, with older age, female gender, and Caucasian ethnicity being a few notable risk factors. The research study also showed a higher incidence of poor outcomes in liver transplant patients who develop TCM, including but not limited to, cardiogenic shock, cardiac arrest, and multi-organ failure.
Liver transplant recipients are a vulnerable patient population who have a higher risk of developing TCM. The development of this cardiac complication is associated with a heightened rate of in-hospital complications. Knowledge of preexisting risk factors may help identify high-risk patients, and can impact management decisions.
Future multicenter, prospective research studies focusing on risk factors and predictors of TCM in orthotopic liver transplant recipients are required, in order to fully explore this disease association and confirm the various outcomes observed in this patient population.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American College of Cardiology; American Society of Echocardiography; Royal Australasian College of Physicians.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eccher A S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, Sarcon A, Geyer V, Neumann CA, Seifert B, Hellermann J, Schwyzer M, Eisenhardt K, Jenewein J, Franke J, Katus HA, Burgdorf C, Schunkert H, Moeller C, Thiele H, Bauersachs J, Tschöpe C, Schultheiss HP, Laney CA, Rajan L, Michels G, Pfister R, Ukena C, Böhm M, Erbel R, Cuneo A, Kuck KH, Jacobshagen C, Hasenfuss G, Karakas M, Koenig W, Rottbauer W, Said SM, Braun-Dullaeus RC, Cuculi F, Banning A, Fischer TA, Vasankari T, Airaksinen KE, Fijalkowski M, Rynkiewicz A, Pawlak M, Opolski G, Dworakowski R, MacCarthy P, Kaiser C, Osswald S, Galiuto L, Crea F, Dichtl W, Franz WM, Empen K, Felix SB, Delmas C, Lairez O, Erne P, Bax JJ, Ford I, Ruschitzka F, Prasad A, Lüscher TF. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med. 2015;373:929-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1401] [Cited by in RCA: 1717] [Article Influence: 171.7] [Reference Citation Analysis (1)] |
| 2. | Kurisu S, Sato H, Kawagoe T, Ishihara M, Shimatani Y, Nishioka K, Kono Y, Umemura T, Nakamura S. Tako-tsubo-like left ventricular dysfunction with ST-segment elevation: a novel cardiac syndrome mimicking acute myocardial infarction. Am Heart J. 2002;143:448-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 617] [Cited by in RCA: 609] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 3. | Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. [Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases]. J Cardiol. 1991;21:203-214. [PubMed] |
| 4. | Akashi YJ, Goldstein DS, Barbaro G, Ueyama T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation. 2008;118:2754-2762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 662] [Cited by in RCA: 590] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 5. | Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblith G, Wu KC, Rade JJ, Bivalacqua TJ, Champion HC. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2159] [Cited by in RCA: 2156] [Article Influence: 107.8] [Reference Citation Analysis (0)] |
| 6. | Vitin AA, Azamfirei L, Tomescu D. Perioperative Stress-Induced (Takotsubo) Cardiomyopathy in Liver Transplant Recipients. J Crit Care Med (Targu Mures). 2018;4:56-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Galván NT, Kumm K, Kueht M, Ha CP, Yoeli D, Cotton RT, Rana A, O'Mahony CA, Halff G, Goss JA. Mending a Broken Heart: Treatment of Stress-Induced Heart Failure after Solid Organ Transplantation. J Transplant. 2018;2018:9739236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Raval Z, Harinstein ME, Skaro AI, Erdogan A, DeWolf AM, Shah SJ, Fix OK, Kay N, Abecassis MI, Gheorghiade M, Flaherty JD. Cardiovascular risk assessment of the liver transplant candidate. J Am Coll Cardiol. 2011;58:223-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 178] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 9. | Alqahtani SA, Fouad TR, Lee SS. Cirrhotic cardiomyopathy. Semin Liver Dis. 2008;28:59-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 10. | Solution Brief The IBM Explorys Platform Liberate your healthcare data [Internet]. [cited 2021 Jun 26]. Available from: https://www.ibm.com/downloads/cas/4P0QB9JN. |
| 11. | US National Library of Medicine Unified Medical Language System (UMLS). Systematized Nomenclature of Medicine-Clinical Terms (SNOMED CT) [Internet]. [cited 2021 May 22]; Available from: https://www.nlm.nih.gov/healthit/snomedct/index.html. |
| 12. | Nelson SJ, Zeng K, Kilbourne J, Powell T, Moore R. Normalized names for clinical drugs: RxNorm at 6 years. J Am Med Inform Assoc. 2011;18:441-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 286] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 13. | Alkhayyat M, Qapaja T, Aggarwal M, Almomani A, Abureesh M, Al-Otoom O, Zmaili M, Mansoor E, Abou Saleh M. Epidemiology and risk of psychiatric disorders among patients with celiac disease: A population-based national study. J Gastroenterol Hepatol. 2021;36:2165-2170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Alkhayyat M, Abureesh M, Almomani A, Abou Saleh M, Zmaili M, El Ouali S, Mansoor E, Rubio-Tapia A, Regueiro M. Patients With Inflammatory Bowel Disease on Treatment Have Lower Rates of Celiac Disease. Inflamm Bowel Dis. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Ashby D. Practical statistics for medical research. Douglas G. Altman, Chapman and Hall, London, 1991. Stat Med [Internet] 1991 [cited 2021 Jun 25]; 10:1635-6. [RCA] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Fede G, Privitera G, Tomaselli T, Spadaro L, Purrello F. Cardiovascular dysfunction in patients with liver cirrhosis. Ann Gastroenterol. 2015;28:31-40. [PubMed] |
| 17. | Åberg F, Isoniemi H, Höckerstedt K. Long-term results of liver transplantation. Scand J Surg. 2011;100:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 18. | Jain A, Reyes J, Kashyap R, Dodson SF, Demetris AJ, Ruppert K, Abu-Elmagd K, Marsh W, Madariaga J, Mazariegos G, Geller D, Bonham CA, Gayowski T, Cacciarelli T, Fontes P, Starzl TE, Fung JJ. Long-term survival after liver transplantation in 4,000 consecutive patients at a single center. Ann Surg. 2000;232:490-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 415] [Cited by in RCA: 410] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 19. | Jadlowiec CC, Taner T. Liver transplantation: Current status and challenges. World J Gastroenterol. 2016;22:4438-4445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 238] [Cited by in RCA: 211] [Article Influence: 23.4] [Reference Citation Analysis (2)] |
| 20. | Moreno R, Berenguer M. Post-liver transplantation medical complications. Ann Hepatol. 2006;5:77-85. [PubMed] [DOI] [Full Text] |
| 21. | Raval Z, Harinstein ME, Skaro AI, Erdogan A, DeWolf AM, Shah SJ, Fix OK, Kay N, Abecassis MI, Gheorghiade M, Flaherty JD. Cardiovascular risk assessment of the liver transplant candidate. J Am Coll Cardiol. 2011;58:223-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 178] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 22. | Khera R, Light-McGroary K, Zahr F, Horwitz PA, Girotra S. Trends in hospitalization for takotsubo cardiomyopathy in the United States. Am Heart J. 2016;172:53-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 89] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 23. | Deshmukh A, Kumar G, Pant S, Rihal C, Murugiah K, Mehta JL. Prevalence of Takotsubo cardiomyopathy in the United States. Am Heart J. 2012;164:66-71.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 299] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 24. | Lemor A, Ramos-Rodriguez AJ, De La Villa R, Hosseini Dehkordi SH, Vazquez de Lara F, Lee S, Rodriguez Rivera M, Casso Dominguez A, Argulian E. Impact of gender on in-hospital outcomes in patients with Takotsubo syndrome: A nationwide analysis from 2006 to 2014. Clin Cardiol. 2019;42:13-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 25. | El-Sayed AM, Brinjikji W, Salka S. Demographic and co-morbid predictors of stress (takotsubo) cardiomyopathy. Am J Cardiol. 2012;110:1368-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 93] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 26. | Vitale C, Rosano GM, Kaski JC. Role of Coronary Microvascular Dysfunction in Takotsubo Cardiomyopathy. Circ J. 2016;80:299-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 27. | Syed FF, Asirvatham SJ, Francis J. Arrhythmia occurrence with takotsubo cardiomyopathy: a literature review. Europace. 2011;13:780-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 28. | Pant S, Deshmukh A, Mehta K, Badheka AO, Tuliani T, Patel NJ, Dabhadkar K, Prasad A, Paydak H. Burden of arrhythmias in patients with Takotsubo cardiomyopathy (apical ballooning syndrome). Int J Cardiol. 2013;170:64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 29. | Vallabhajosyula S, Deshmukh AJ, Kashani K, Prasad A, Sakhuja A. Tako-Tsubo Cardiomyopathy in Severe Sepsis: Nationwide Trends, Predictors, and Outcomes. J Am Heart Assoc. 2018;7:e009160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 30. | Cappelletti S, Ciallella C, Aromatario M, Ashrafian H, Harding S, Athanasiou T. Takotsubo Cardiomyopathy and Sepsis. Angiology. 2017;68:288-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 31. | Richard C. Stress-related cardiomyopathies. Ann Intensive Care. 2011;1:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 32. | Haft JW, Atluri P, Ailawadi G, Engelman DT, Grant MC, Hassan A, Legare JF, Whitman GJR, Arora RC; Society of Thoracic Surgeons COVID-19 Task Force and the Workforce for Adult Cardiac and Vascular Surgery. Adult Cardiac Surgery During the COVID-19 Pandemic: A Tiered Patient Triage Guidance Statement. Ann Thorac Surg. 2020;110:697-700. [PubMed] |
| 33. | Giustino G, Croft LB, Oates CP, Rahman K, Lerakis S, Reddy VY, Goldman M. Takotsubo Cardiomyopathy in COVID-19. J Am Coll Cardiol. 2020;76:628-629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 103] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 34. | Dweck MR, Bularga A, Hahn RT, Bing R, Lee KK, Chapman AR, White A, Salvo GD, Sade LE, Pearce K, Newby DE, Popescu BA, Donal E, Cosyns B, Edvardsen T, Mills NL, Haugaa K. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21:949-958. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 213] [Cited by in RCA: 300] [Article Influence: 60.0] [Reference Citation Analysis (0)] |
| 35. | Figueiredo Neto JA, Marcondes-Braga FG, Moura LZ, Figueiredo AMES, Figueiredo VMES, Mourilhe-Rocha R, Mesquita ET. Coronavirus Disease 2019 and the Myocardium. Arq Bras Cardiol. 2020;114:1051-1057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 36. | Chadha S. 'COVID-19 pandemic' anxiety-induced Takotsubo cardiomyopathy. QJM. 2020;113:488-490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 37. | Montone RA, Iannaccone G, Meucci MC, Gurgoglione F, Niccoli G. Myocardial and Microvascular Injury Due to Coronavirus Disease 2019. Eur Cardiol. 2020;15:e52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 38. | Satturwar S, Fowkes M, Farver C, Wilson AM, Eccher A, Girolami I, Pujadas E, Bryce C, Salem F, El Jamal SM, Paniz-Mondolfi A, Petersen B, Gordon RE, Reidy J, Fraggetta F, Marshall DA, Pantanowitz L. Postmortem Findings Associated With SARS-CoV-2: Systematic Review and Meta-analysis. Am J Surg Pathol. 2021;45:587-603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 77] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 39. | Vallabhajosyula S, Barsness GW, Herrmann J, Anavekar NS, Gulati R, Prasad A. Comparison of Complications and In-Hospital Mortality in Takotsubo (Apical Ballooning/Stress) Cardiomyopathy Versus Acute Myocardial Infarction. Am J Cardiol. 2020;132:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 40. | Tsuchihashi K, Ueshima K, Uchida T, Oh-mura N, Kimura K, Owa M, Yoshiyama M, Miyazaki S, Haze K, Ogawa H, Honda T, Hase M, Kai R, Morii I; Angina Pectoris-Myocardial Infarction Investigations in Japan. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol. 2001;38:11-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1181] [Cited by in RCA: 1142] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 41. | Bybee KA, Kara T, Prasad A, Lerman A, Barsness GW, Wright RS, Rihal CS. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med. 2004;141:858-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1048] [Cited by in RCA: 1020] [Article Influence: 48.6] [Reference Citation Analysis (0)] |