Published online Mar 27, 2019. doi: 10.4254/wjh.v11.i3.318
Peer-review started: November 30, 2018
First decision: December 17, 2018
Revised: January 19, 2019
Accepted: January 29, 2019
Article in press: January 30, 2019
Published online: March 27, 2019
Processing time: 118 Days and 2.2 Hours
Most patients with hydatid cysts are asymptomatic, and they are diagnosed incidentally during radiological evaluations performed for other reasons. However, some patients develop symptoms and complications due to cyst size, location, and the relationship between the cyst and adjacent structures. The most serious complications that can occur are rupture of the cysts into the biliary tract, vascular structures, hollow viscus, and peritoneal cavity. We aimed to describe the management of four cases of intraperitoneal rupture of hydatid cysts.
Four patients aged between 27 and 44 years (two men and two women) were admitted to our clinic with sudden abdominal pain (n = 4), hypotension (n = 3), and anaphylaxis (n = 2). Three of the perforated cysts were located in the liver, and one was located in the spleen. Two patients developed cyst rupture after minor trauma, and the other two developed spontaneous rupture. Enzyme-linked immunosorbent assay IgG results were positive for two patients and negative for the other two. All patients received albendazole treatment after surgical intervention (range: 2-6 mo). Two patients developed hepatic abscesses requiring drainage; one of these patients also developed hydatid cyst recurrence during postoperative follow-up (range: 25-80 mo).
Intraperitoneal rupture is a life-threatening complication of hydatid cysts. It is important to manage patients with surgical intervention as soon as possible with aggressive medical treatment for anaphylactic reactions.
Core tip: Spontaneous or traumatic intraperitoneal hydatid cyst rupture is a rare but life-threatening complication. Therefore, hydatid cyst rupture should be considered as a differential diagnosis in patients who have sudden onset abdominal pain and allergic reactions like urticaria, especially those in regions endemic to the disease. Deteriorated hemodynamic parameters due to anaphylactic reactions should be corrected quickly with subsequent emergent surgery for a life-saving procedure. Herein, we aimed to present the management algorithm of four patients diagnosed with intraperitoneal hydatid cyst rupture.
- Citation: Akbulut S, Ozdemir F. Intraperitoneal rupture of the hydatid cyst: Four case reports and literature review. World J Hepatol 2019; 11(3): 318-329
- URL: https://www.wjgnet.com/1948-5182/full/v11/i3/318.htm
- DOI: https://dx.doi.org/10.4254/wjh.v11.i3.318
Hydatic disease is a zoonotic disease caused by the echinococcus parasite, which is a member of the Taeniidae family. Most common echinococcus species that cause hydatid disease in humans are Echinococcus granulosus (cystic echinococcosis) and Echinococcus multilocularis (alveolar echinococcosis). Cystic echinococcosis, also known as hydatid cysts, constitute 95% of all hydatid diseases [1-3]. Hydatid diseases can develop in almost all organs and tissues of the human body, but the most frequently involved organs are the liver (50%-77%), lungs (15%-47%), spleen (0.5%-8%), and kidneys (2%-4%) [1-6]. Humans, who have no role in the biological life cycle of echinococcosis, can accidentally become intermediate hosts by ingesting tapeworm eggs [1,4]. Hydatid cysts can grow at an average of 10-50 mm/year depending on the location of the cyst, so most patients remain asymptomatic for years [3,7,8]. Usually, asymptomatic patients are diagnosed incidentally by radiological evaluations that are performed for other reasons. Nevertheless, some patients have signs and symptoms, including mild or severe abdominal pain, nausea, vomiting, jaundice due to size, location, and/or involvement of the adjacent structures and organs of the cystic lesions[1]. The most frequently reported complications are rupture (perforation), bacterial infection, anaphylactic reaction, compression of the vascular and biliary structures, and compression of the neighboring organs[4,5]. Hydatid cyst rupture can be internal (cysto-biliary fistula, rupture into the hollow viscus, broncho-biliary fistula, bronchopleural fistula, intrapericardial rupture, intrapleural rupture, intraperitoneal rupture) or more rarely, it can be external (cysto-cutaneous fistula)[3]. Intraperitoneal rupture is a rare but life-threatening, severe complication of hydatid cyst disease[3]. We aim to describe the cases of four patients who developed intraperitoneal rupture and review the medical literature.
The summary information of the four cases described below is given in Table 1.
| Parameters | Case 1 | Case 2 | Case 3 | Case 4 |
| Age | 44 | 37 | 27 | 40 |
| Gender | Male | Male | Female | Female |
| Cause of perforation | Spontaneous | Trauma | Spontaneous | Trauma |
| Clinical presentation | Pain (sudden) | Pain (sudden) | Pain (sudden) | Pain (sudden) |
| Hypotension | Hypotension | Hypotension | Anaphylaxis | |
| Anaphylaxis | Anaphylaxis | Not clear | ||
| Serology | ELISA IgG (+) | ELISA IgG (+) | Negative | Negative |
| History of HD | Known | Unknown | Unknown | Known |
| Cyst location | Liver (Bilobar) | Spleen | Liver (Bilobar) | Liver (Bilobar) |
| Retroperitoneum | ||||
| Retrovesical | ||||
| Perforated cyst location | Liver (VI) | Spleen | Liver (III) | Liver (II-VI) |
| Cysts size (mm) | 165 × 100 × 80 | 50 × 45 | 80 × 75 | 110 × 85 |
| 130 × 100 × 95 | 50 × 40 | 40 × 10 | 30 × 25 | |
| 85 × 70 × 65 | 60 × 50 | |||
| Preop antihelmintic | ALBZ (1 mo) | No | No | ALBZ (? mo) |
| Postop antihelmintic | ALBZ (6 mo) | ALBZ (2 mo) | ALBZ (2 mo) | ALBZ (2 mo) |
| Diagnostic tools | US + CT | US | US + CT | CT |
| Surgical approach | Partial Cystectomy+ | Splenectomy+ | Partial Cystectomy+ | Partial Cystectomy+ |
| CBD exploration+ | Retroperitoneal+ | Omentopexy | Omentopexy | |
| T-tube insertion+ | Retrovesical | |||
| Omentopexy | Cystectomy | |||
| Recurrence | Yes | No | No | No |
| Postop complication | Liver abscess | Bleeding | No | Liver abscess |
| Follow up (mo) | 80 | 34 | 25 | 36 |
A 44-year-old man was admitted to the emergency department with sudden onset abdominal pain, skin flushing at some areas of the abdomen and hypotensive shock without any history of trauma.
The patient was diagnosed with obstructive jaundice complicated by a hydatid cyst approximately one month ago. The connection between the biliary tract and hydatid cyst was visualized by radiological examinations. Endoscopic retrograde cholangiopancreatography (ERCP) was performed to decompress the biliary tract before surgical intervention. Albendazole treatment was initiated before the surgery.
The patient had no medical disease other than the hydatid cyst.
Complete blood count (CBC) was as follows: White blood cells (WBCs): 12900/mL, neutrophils: 80%, and eosinophils: 0.9%. Test results for biochemical analysis were as follows: Aspartate aminotransferase (AST), 152 (5-34 U/L); alanine aminotransferase (ALT), 58 (5-34 U/L); alkaline phosphatase (ALP), 260 (40-150 U/L); gamma-glutamyl transferase (GGT) 125, (12-64 U/L); and total bilirubin, 1.03 (0.2-1.2 mg/dL).
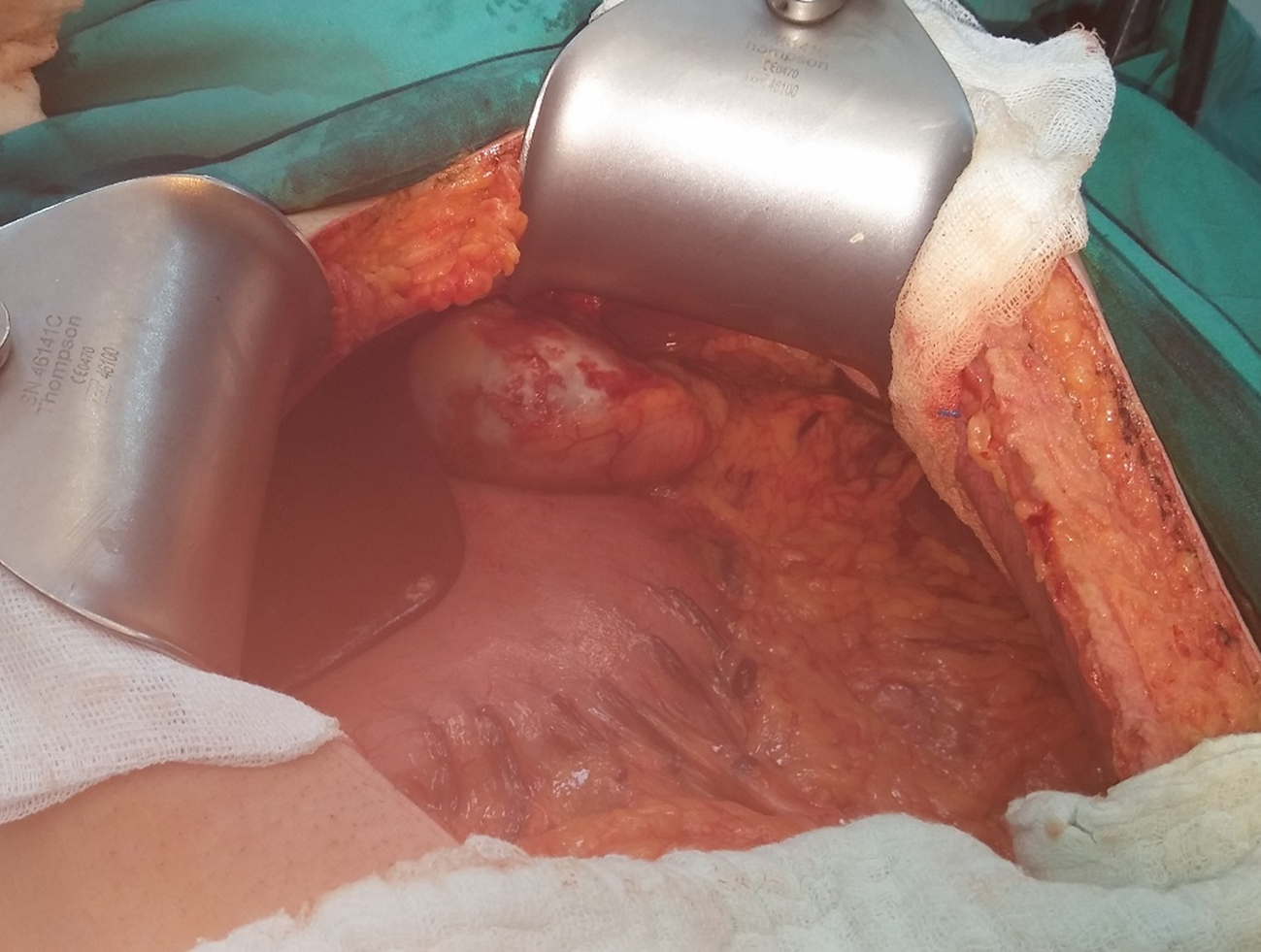
Abdominal ultrasonography (US) and contrast-enhanced abdominal computed tomography (CT) showed that multiple cystic lesions compatible with hydatid cyst disease (largest size 165 mm × 100 mm × 80 mm) were localized in the liver. CT scans also showed that the ruptured cystic lesion was localized in the VI segment of the liver (Figures 1 and 2).
The final diagnosis of the present case was intraperitoneal liver hydatid cyst rupture.
Fluid resuscitation, antihistaminic, and corticosteroid treatment was initiated at the emergency department. Laparotomy was performed due to the patient’s general condition. Intraoperatively, the cyst located in the liver ruptured, and 2500 mL of fluid containing cyst material was aspirated from the peritoneal cavity. The peritoneal cavity was washed with saline solution and partial cystectomy, omentoplasty, and common bile duct exploration with T-tube placement were performed.
The patient developed an abscess that required drainage in the postoperative period. Six albendazole treatments with 3-wk cycles were administered as medical treatment. The T-tube was removed when normal biliary tract anatomy was visualized during cholangiography, approximately three weeks postoperative.
A 37-year-old man presented in our emergency unit with severe abdominal pain and anaphylactic shock signs/symptoms, such as hypotension and allergic reaction.
The patient suddenly felt sharp abdominal pain after playing with and tossing his nephew and simultaneously felt like something was leaking inside him. Subsequently, dizziness and diffuse flushing occurred.
CBC analysis revealed leukocytosis (18800/mL), with predominant neutrophils (86.4%) and normal eosinophils (0.1%). Biochemical blood test results were within normal limits except for total bilirubin (1.5 mg/dL).
US showed massive intraabdominal fluid collections in the perihepatic and perisplenic area. Additionally, a ruptured and degenerated cyst with a germinative membrane collapse near the spleen was visualized.
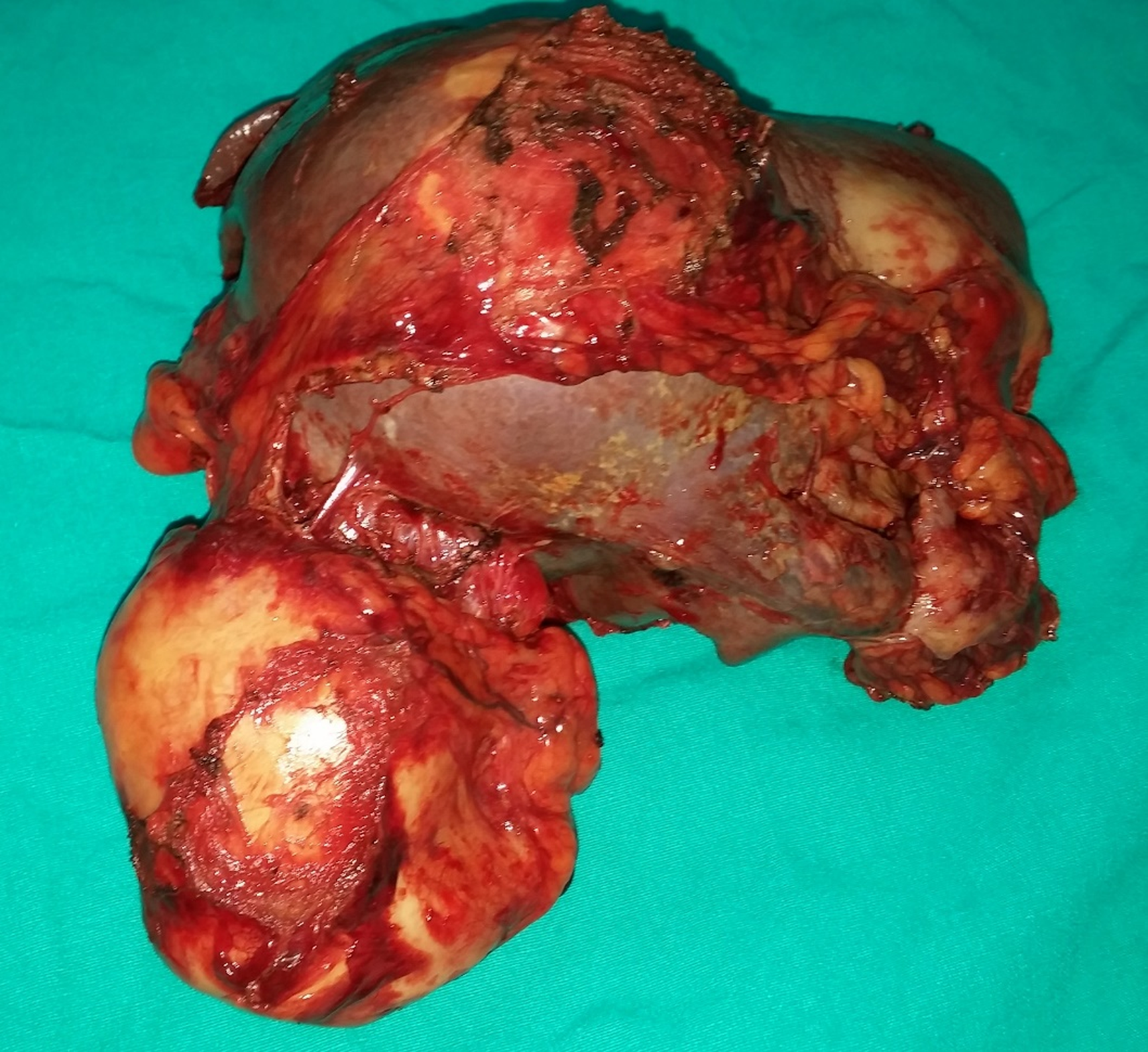
The final diagnosis of the present case was intraperitoneal splenic hydatid cyst rupture.
Fluid resuscitation, antihistaminic, and corticosteroid treatment was initiated at the emergency department. The patient was then taken to the operating room, and laparotomy was performed with a midline incision. An exophytic, ruptured hydatid cyst originating from the spleen, which had adhesions to adjacent structures, was identified. Total splenectomy was required (Figures 3 and 4). An iatrogenic left diaphragm injury due to intraabdominal adhesions occurred during surgery. A left-sided chest tube was inserted after the primary repair of the diaphragm. Additionally, other cystic lesions located at the posterior side of the urinary bladder (60 mm × 50 mm) and at the retroperitoneum (50 mm× 40 mm) were completely excised. A chest tube was removed postoperatively on the fourth day.
The patient had an uneventful postoperative clinical course. Pneumococcus vaccination was administered 14 d after surgery. Continuous albendazole treatment was administered for two months after surgery.
A 27-year-old woman experienced sudden onset abdominal pain at another medical center. She was diagnosed with a ruptured hydatid cyst and was referred to our medical center. She had hypotension during her first evaluation at the emergency unit.
She had no history of hydatid cyst.
CBC analysis showed leukocytosis (24100/mL) with predominant neutrophils (94.5%) and normal eosinophils (0.2%). Biochemical blood tests were within normal limits.
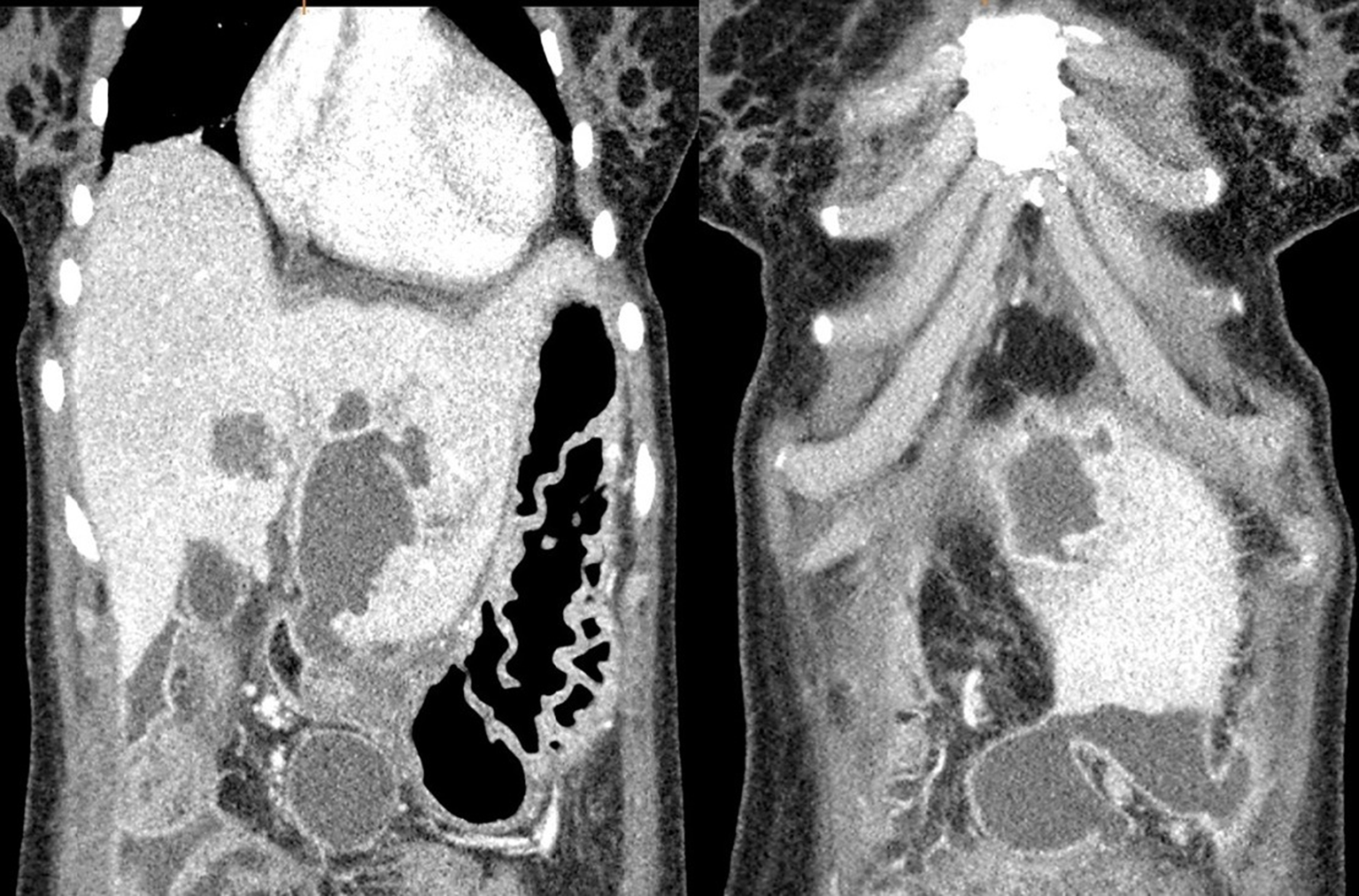
Contrast-enhanced abdominal CT revealed that one lesion was compatible with a hydatid cyst in the anterior sector of the liver (80 mm × 75 mm × 70 mm) and another one at segment III (40 mm × 10 mm). Additionally, several daughter cystic lesions (largest diameter 130 mm × 60 mm × 50 mm) secondary to the rupture of the cystic lesion near segment III were observed in the pelvic cavity (Figure 5).
The final diagnosis of the present case was an intraperitoneal liver hydatid cyst rupture.
Fluid resuscitation was initiated at the emergency department. The patient was then taken to the operating room. The anterior wall of the cyst located in the anterior sector of the liver was excised, and the cystic components were completely evacuated. Three bile ducts that opened into the cystic cavity were closed with polypropylene sutures. Afterwards, the hydatid cyst wall localized next to segment III was excised, and the cyst components were completely evacuated. Cholecystectomy was performed to place high pressure saline solution into the common bile duct via cystic duct; there was no bile leak. Daughter vesicles located in the pelvic cavity were also removed, and the peritoneal cavity was washed with hypertonic saline solution.
The patient had an uneventful postoperative clinical course. Postoperative albendazole treatment was administered for two months.
A 40-year-old woman was suffering from abdominal pain for one month, and her pain became aggravated for two days prior to admission. Physical examination revealed widespread tenderness in all quadrants of the abdomen.
The patient stated that she had received antihelmintic medical treatment several times.
CBC analysis showed leukocytosis (WBC: 23400/mm3, neutrophils: 90.6%, and eosinophils: 0.4%). Biochemical results were not altered except for ALP and GGT levels (AST: 18 U/L, ALT: 18 U/L, ALP: 197 U/L, GGT: 114 U/L, and total bilirubin 0.87 mg/dL).
Contrast-enhanced abdominal CT revealed several hydatid cysts (largest diameter 10 mm × 85 mm × 60 mm) in the left lobe of the liver. Cysts located in the left lobe of the liver compressed the main bile duct, causing dilation of the intrahepatic bile ducts of the left liver lobe (Figure 6). Several cystic lesions were also observed in the pelvic cavity.
The final diagnosis of the present case was intraperitoneal liver hydatid cyst rupture.
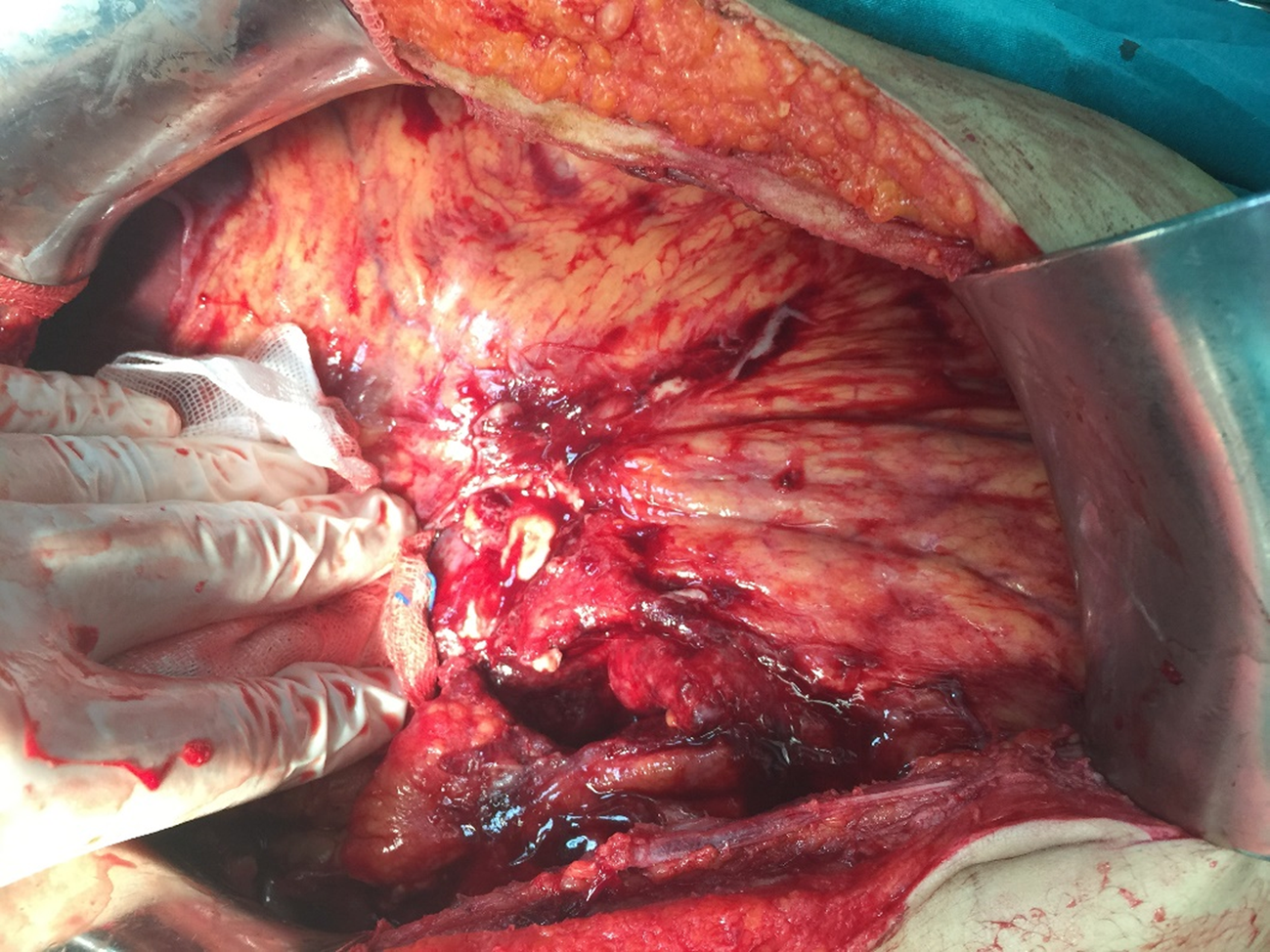
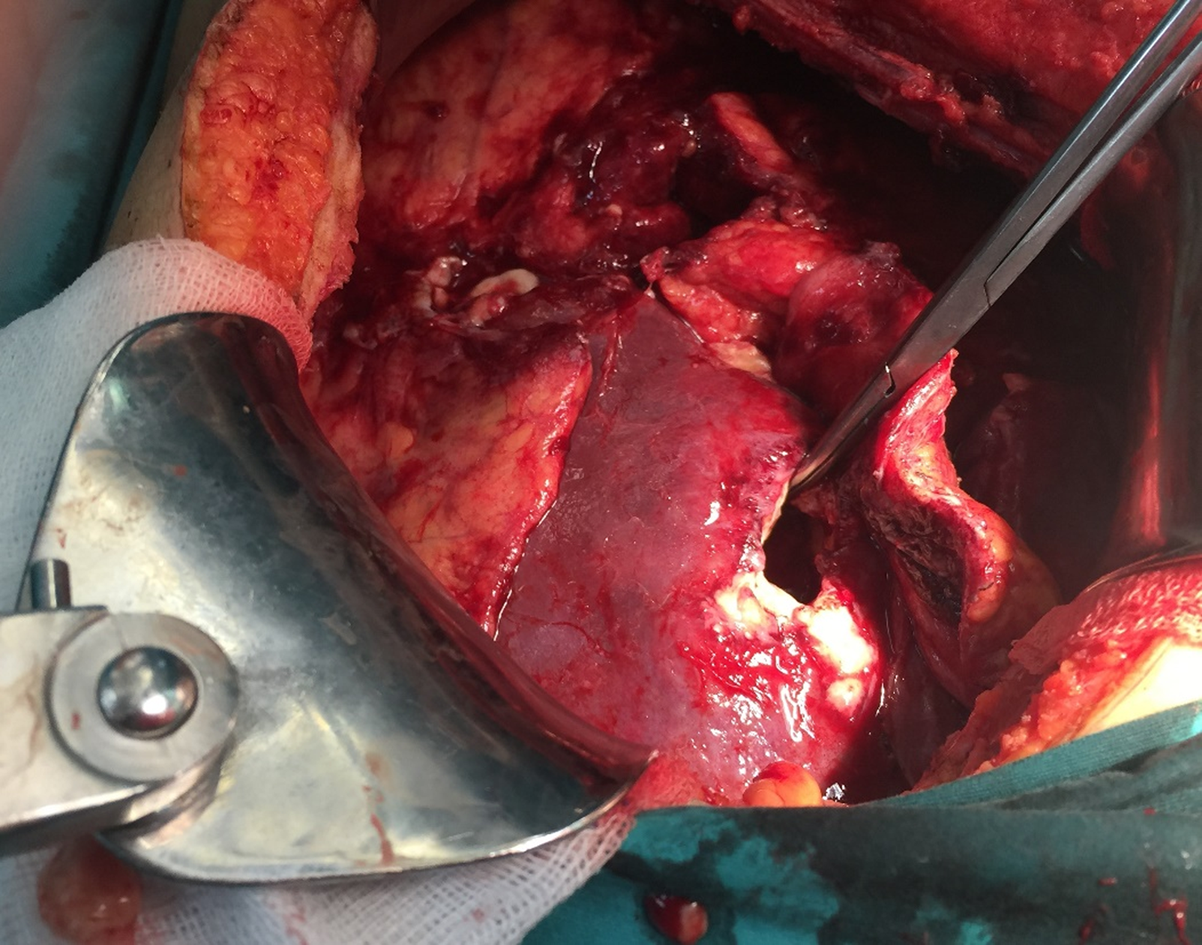
There were several adhesions secondary to the ruptured cyst, and they were diagnosed during laparotomy as sclerosing encapsulated peritonitis (Figure 7). After adhesiolysis, the perforated wall of the cyst was excised, and the cyst components were completely evacuated (Figure 8). Additionally, cystic components located in the pelvic cavity were removed.
The patient had an uneventful postoperative clinical course and was treated with continuous albendazole for two months. The patient developed left lobe liver abscess in the third postoperative year, which required percutaneous drainage.
About 5%-40% of the hydatid cysts located in the liver and other organs of the body may cause various complications. The most common complications related with hydatid cysts include superinfection, cysto-biliary fistula (obstructive jaundice, cholangitis), allergic reactions, rupture into the gastrointestinal system (duodenum, small intestine, colon), Budd Chiari syndrome, portal hypertension, gastric outlet obstruction, membranous glomerulonephritis, broncho-biliary fistula, bronchopleural fistula, intrapericardial rupture, intrapleural rupture, and intraperitoneal rupture[1,3,7,9].
Intraperitoneal hydatid cyst rupture may result from trauma or may spontaneously occur due to increased intracystic pressure [1,10,11]. Sometimes, iatrogenic hydatid cyst rupture may occur during elective surgery. Some studies have concluded that most intraperitoneal ruptures develop after trauma; nevertheless, other studies pointed out that spontaneous ruptures may develop more frequently [6,7,12].
Intraperitoneal rupture is the third most common complication (0.9%-16%) after intrabiliary rupture (5%-25%) and allergic reactions (1%-25%)[1,4,7]. Most studies regarding intraperitoneal hydatid cyst rupture have been published as case reports. To our knowledge, four or more cases were reported in a limited number of studies[4,6,9,13-22] (Table 2). Risk factors for rupture include young age, cyst diameter (> 10 cm), and superficial localization [1,4,7]. Hydatid cysts are more common in younger individuals because they are exposed to traffic accidents more often than older individuals. Intracystic pressure increases with increasing cyst dimension. When intracystic pressure increases to more than 50 cmH2O, spontaneous or traumatic rupture risk also increases [6,10]. Most superficial cyst walls are not protected by the liver parenchyma. This is a facilitating factor for rupture of the cyst into peritoneal cavity or hollow gastrointestinal organs [1,4]. The aims of emergent surgical treatment include prevention or minimization of anaphylactic reactions in the early term and prevention of the development of long-term secondary peritoneal hydatidosis [4,7].
| Authors | Years | Country | City | Study period | Perforated HC | Total HC surgery | Rate (%) |
| Toumi | 2017 | Tunusia | Monastir | 1990-2015 | 12 | 1350 | 0,9 |
| Sakcak | 2015 | Turkey | Ankara | 1996-2013 | 16 | 756 | 2,1 |
| Ozturk | 2007 | Turkey | Erzurum | 1979-2004 | 20 | 653 | 3,1 |
| Mouqait | 2013 | Morocco | Fes | 2008-2012 | 14 | 306 | 4,6 |
| Derici | 2007 | Turkey | Izmir | 1988-2005 | 17 | 306 | 5,6 |
| Unalp | 2010 | Turkey | Izmir | 2000-2009 | 21 | 368 | 5,7 |
| Kurt | 2003 | Turkey | Istanbul | 1995-2001 | 7 | 99 | 7,1 |
| Akcan | 2010 | Turkey | Kayseri | 1990-2008 | 28 | 372 | 7,5 |
| Bozdag | 2016 | Turkey | Diyarbakir | 2005-2015 | 16 | NA | NA |
| Ozturk | 2016 | Turkey | Izmir | 2008-2012 | 13 | NA | NA |
| Dirican | 2010 | Turkey | Malatya | 2003-2008 | 10 | NA | NA |
| Rami | 2009 | Morocco | Fes | NA | 4 | NA | NA |
| Gunay | 1999 | Turkey | Istanbul | 1985-1997 | 16 | NA | NA |
Clinical signs and symptoms of intraperitoneal cyst ruptures may vary widely among patients. The most frequent symptoms are mild or severe abdominal pain, vomiting, nausea, and some allergic reactions that span a wide range. If the content of the ruptured cyst is purulent or associated with the biliary tract, it may cause peritoneal irritation. Therefore, clinical signs of acute abdominal pain may occur [1,4]. A wide spectrum of life-threatening immunologic reactions, such as allergic reactions and/or anaphylactic shock, develop against the cyst content, which spread into the peritoneal cavity [1,4]. Therefore, some patients may have complaints such as hypotension, tachycardia, and respiratory distress [1].
While 16.7%-25% of patients with hydatid cyst rupture develop minor allergic reactions, such as urticaria and macular eruption, 1%-12.5% of patients develop more severe allergic reactions such as peripheral edema, syncope, and anaphylaxis [1,6]. The life-threatening anaphylactic shock incidence rate is approximately 1.4%. Allergic reactions may develop in macroscopic ruptures or when the cyst contents pass into the biliary tract after trauma, iatrogenic interventions, or spontaneously. Even allergic reactions may occur after direct communication when the cyst contents enter systemic circulation [1]. Anaphylactic reactions during cyst hydatid surgery may develop in 0.2%-3.3% of patients who do not experience rupture [1].
Most patients who have intraperitoneal rupture are admitted to the emergency unit with symptoms such as severe abdominal pain, hypotension, tachycardia, and allergic reactions[1,10,11]. Therefore, US is the most common radiologic tool for diagnosis. If patients are hemodynamically stable, contrast-enhanced CT may be used. The sensitivity of US and CT is 85% and 100%, respectively [1,8,9].
Medical treatment should be initiated as soon as possible at the emergency unit after confirming the diagnosis of intraperitoneal rupture. Moreover, it should be continued during surgery. To minimize morbidity and mortality, patients should be hemodynamically stabilized before surgery, and they should undergo surgery as soon as possible. Medical treatment is aimed at stabilizing hemodynamic status with fluid resuscitation and treating anaphylactic reactions with corticosteroids, antihistaminic, and vasopressor drugs.
There is no consensus in the literature about surgical treatment options for intraperitoneal cyst rupture [7,12]. We suggest that each case should be evaluated separately in accordance with the general principles of hydatid cyst surgery. Simply summarized, hemodynamically stable patients should undergo either laparoscopic or open surgery as soon as possible, and hemodynamically unstable patients should undergo open surgery. Cyst contents that trigger anaphylactic reactions should be removed from the abdominal cavity as soon as possible [1,5-7]. The peritoneal cavity should be washed with scolicidal solutions such as formaldehyde, hypertonic saline (3%-10%-15%-30%), silver nitrate (0.5%), cetrimide, chlorhexidine, cetrimide plus chlorhexidine (1.5%/0.15%), hydrogen peroxide (1.5%-3%), povidone iodine (10%-50%), or ethyl alcohol (70%-95%). Each solution has a different time frame for possible scolicidal effects [1,5-7]. We prefer hypertonic saline or cetrimide plus chlorhexidine to wash the peritoneal cavity at least two times within 10 min for 10-15 min each [1]. Allergens that lead to anaphylactic reactions can be removed in this manner. Perforated cystic cavities should be carefully evaluated. Remaining cystic contents should also be evacuated, and the free edges of the cystic cavity should be widely excised. Perforated cysts that are located in the liver should be examined via a leakage test, which can be performed with a saline solution administered through the common bile duct/cystic duct to observe the relationship between the cyst and the biliary tract. Bile duct orificies that lead to bile leakage should be repaired with different suture materials. Common bile duct and T-tube placement for high flow output bile fistulas can be performed simultaneously. Sometimes, ERCP can be selected instead of T-tube application to complete the surgery as soon as possible. The biliary tract can be visualized via ERCP. If possible, spleen-preserving surgical interventions should be preferred [5]. Abdominal drains should be placed both into the cystic cavity and in the abdomen before surgery completion. Next, we would like to discuss the question ‘’do we need any intervention for other unperforated cystic lesions identified during emergency surgery?’’
Antihelmintic treatment should be administered as soon as possible for patients diagnosed with intraperitoneal rupture to prevent disease recurrence due to overlooked cystic contents during surgery. The most preferred antihelmintic agent is albendazole (10-15 mg/kg per day). According to the literature, the treatment period should last between 1 and 12 mo [1,4,6,8]. Patients diagnosed with intraperitoneal hydatid cyst rupture should be followed-up more frequently than patients without complications. Morbidity and mortality rates after intraperitoneal rupture are 10-35.3% and 0-23.5%, respectively [7,9]. Clinical follow-up should be performed monthly, especially during the early period after surgery and once a year in the long-term. US, echinococcus IgG enzyme-linked immunosorbent assay, indirect hemagglutination, and CT can be selected during follow-up. If there is no recurrence after five years, clinical follow-up can be terminated. The recurrence rate after intraperitoneal hydatid cyst rupture is reported between 0-28.6%[1,4,6,7,9]. There was only one case of recurrence in our series.
Intraperitoneal hydatid cyst rupture is a life-threatening complication because it causes serious hemodynamic instability and allergic reactions. Therefore, hydatid cyst rupture should be considered a differential diagnosis in patients who have sudden onset abdominal pain and allergic reactions, like urticaria, especially in regions endemic for the disease. Deteriorated hemodynamic parameters due to anaphylactic reactions should be quickly corrected so that emergent surgery can be life-saving.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Turkey
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Farshadpour F, Jarcuska P S-Editor: Ji FF L-Editor: Filipodia E-Editor: Zhang YL
| 1. | Yilmaz M, Akbulut S, Kahraman A, Yilmaz S. Liver hydatid cyst rupture into the peritoneal cavity after abdominal trauma: case report and literature review. Int Surg. 2012;97:239-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Akbulut S, Sogutcu N, Eris C. Hydatid disease of the spleen: single-center experience and a brief literature review. J Gastrointest Surg. 2013;17:1784-1795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (2)] |
| 3. | Akbulut S. Parietal complication of the hydatid disease: Comprehensive literature review. Medicine (Baltimore). 2018;97:e10671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Toumi O, Noomen F, Salem R, Rabeh H, Jabra SB, Korbi I, Bannani S, Nasr M, Zouari K, Mondher G, Hamdi A. Intraperitoneal rupture of hydatid cysts. Eur J Trauma Emerg Surg. 2017;43:387-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Belli S, Akbulut S, Erbay G, Koçer NE. Spontaneous giant splenic hydatid cyst rupture causing fatal anaphylactic shock: a case report and brief literature review. Turk J Gastroenterol. 2014;25:88-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Unalp HR, Yilmaz Y, Durak E, Kamer E, Tarcan E. Rupture of liver hydatid cysts into the peritoneal cavity. A challenge in endemic regions. Saudi Med J. 2010;31:37-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Tinsley B, Abbara A, Kadaba R, Sheth H, Sandhu G. Spontaneous intraperitoneal rupture of a hepatic hydatid cyst with subsequent anaphylaxis: a case report. Case Reports Hepatol. 2013;2013:320418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Sozuer E, Akyuz M, Akbulut S. Open surgery for hepatic hydatid disease. Int Surg. 2014;99:764-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Mouaqit O, Hibatallah A, Oussaden A, Maazaz K, Taleb KA. Acute intraperitoneal rupture of hydatid cysts: a surgical experience with 14 cases. World J Emerg Surg. 2013;8:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Malik AA, Bari SU, Amin R, Jan M. Surgical management of complicated hydatid cysts of the liver. World J Gastrointest Surg. 2010;2:78-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Karakaya K. Spontaneous rupture of a hepatic hydatid cyst into the peritoneum causing only mild abdominal pain: a case report. World J Gastroenterol. 2007;13:806-808. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 12. | Erel S, Kilicoglu B, Kismet K, Gollu A, Akkus MA. Peritoneal hydatid cyst perforation: a rare cause of emergency abdominal surgeries. Adv Ther. 2008;25:943-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Sakcak I, Erdogan A, Aydogan I, Ismail E, Doganay M, Akat Z. Long-term outcomes of ruptured intraperitoneal hydatid cysts. J J Gastro Hepato. 2015;2:18. |
| 14. | Ozturk S, Han I, Carti EB, Unver M, Ozturk BK, Kebapci E, Olmez M, Zalluhoglu N, Aydin C, Akbulut G. A Rare emergency intraperitoneal perforation of liver hydatid cysts. clinical presentation and surgical outcomes of double center experience. J Surg Arts (Cer San D). 2016;2:61-66. |
| 15. | Ozturk G, Aydinli B, Yildirgan MI, Basoglu M, Atamanalp SS, Polat KY, Alper F, Guvendi B, Akcay MN, Oren D. Posttraumatic free intraperitoneal rupture of liver cystic echinococcosis: a case series and review of literature. Am J Surg. 2007;194:313-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Derici H, Tansug T, Reyhan E, Bozdag AD, Nazli O. Acute intraperitoneal rupture of hydatid cysts. World J Surg. 2006;30:1879-1883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Kurt N, Oncel M, Gulmez S, Ozkan Z, Uzun H. Spontaneous and traumatic intra-peritoneal perforations of hepatic hydatid cysts: a case series. J Gastrointest Surg. 2003;7:635-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Akcan A, Sozuer E, Akyildiz H, Ozturk A, Atalay A, Yilmaz Z. Predisposing factors and surgical outcome of complicated liver hydatid cysts. World J Gastroenterol. 2010;16:3040-3048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Bozdag Z, Turkoglu A, Yilmaz EE, Gul M. A rare reason for acute abdomen: Intraperitoneal liver hydatid cyst rupture. Dig Liver Dis. 2016;48:98-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Dirican A, Yilmaz M, Unal B, Tatli F, Piskin T, Kayaalp C. Ruptured Hydatid Cysts into the peritoneum: A case series. Eur J Trauma Emerg Surg. 2010;36:375–379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Rami M, Khattala K, Mahmoudi A, El Madi A. Ruptured hepatic hydatid cyst: Report of four cases. Ann Pediatr Surg. 2009;5:146-149. |