Published online Feb 27, 2019. doi: 10.4254/wjh.v11.i2.217
Peer-review started: August 31, 2018
First decision: October 16, 2018
Revised: December 31, 2018
Accepted: January 9, 2019
Article in press: January 9, 2019
Published online: February 27, 2019
Processing time: 179 Days and 7.8 Hours
Transjugular intrahepatic portosystemic shunts (TIPS) can alleviate complications of portal hypertension such as ascites and variceal bleeding by decreasing the portosystemic gradient. In limited clinical situations, parallel TIPS may be only solution to alleviate either variceal bleeding or ascites secondary to portal hypertension when the primary TIPS fails to do so. Data specifically addressing the use of this partially polytetrafluoroethylene covered nitinol stent (Viatorr®) is largely lacking despite Viatorr® being the current gold standard for modern TIPS placement.
All three patients had portal hypertension and already had a primary Viatorr® TIPS placed previously. All patients have undergone failed endoscopy to manage acute variceal bleeding before referral for a parallel stent (PS). PS were placed in patients presenting with recurrent variceal bleeding despite existence of a widely patent primary TIPS. Primary stent patency was verified with either Doppler ultrasound or intra-procedural TIPS stent venography. Doppler ultrasound follow-up imaging demonstrated complete patency of both primary and parallel TIPS. All three patients did well on clinical follow-up of up to six months and no major complications were recorded. A review of existing literature on the role of PS in the management of portal hypertension complications is discussed. There are three case reports of use of primary and PS Viatorr® stents placement, only one of which is in a patient with gastrointestinal variceal bleeding despite a patent primary Viatorr® TIPS.
Viatorr® PS placement in the management of variceal hemorrhage is feasible with promising short term patency and clinical follow-up data.
Core tip: To our knowledge, we are first to report a three-case series with 6-month follow-up data using Viatorr® for both primary transjugular intrahepatic portosystemic shunt (TIPS) and parallel TIPS placement for the management of recurrent upper gastrointestinal variceal hemorrhage. Although, parallel TIPS placement has been previously reported, it was largely using bare metal stents and/or fully covered stents. Data regarding the use of the partially polytetrafluoroethylene-covered nitinol stent (Viatorr®) in parallel TIPS placement is largely lacking despite this device being the current gold standard for TIPS placement.
- Citation: Raissi D, Yu Q, Nisiewicz M, Krohmer S. Parallel transjugular intrahepatic portosystemic shunt with Viatorr® stents for primary TIPS insufficiency: Case series and review of literature . World J Hepatol 2019; 11(2): 217-225
- URL: https://www.wjgnet.com/1948-5182/full/v11/i2/217.htm
- DOI: https://dx.doi.org/10.4254/wjh.v11.i2.217
Gastroesophageal varices and ascites are common complications of portal hyperten-sion and cirrhosis. It is estimated that the mortality during the first episode of acute upper gastrointestinal variceal bleeding in cirrhotic patients is between 15%-30%[1-3], whereas the mortality rates of ascites in those patients increases from 15% to 44% between one-year and five-year follow-ups[4,5]. Transjugular intrahepatic portosystemic shunt (TIPS) can alleviate these two complications by decreasing the portosystemic gradient. This is achieved by decompressing the portal venous system directly via a stent supported shunt into the systemic circulation[6-9]. A previous study suggested an association between the early use of TIPS in cirrhotic patients with variceal bleeding with a reduction in mortality[10]. Additionally, according to a meta-analysis of four randomized trials, cirrhotic patients with recurring ascites that have received TIPS demonstrated a higher transplant-free survival compared to those receiving paracentesis at 6, 12, 24, and 36 months: 75.1% vs 65.3%, 63.1% vs 52.5%, 49.0% vs 35.2%, and 38.1% vs 28.7% (P = 0.035)[11]. Yet, one complication of TIPS was shunt dysfunction, which could be manifested by the persistence or recurrence of ascites, variceal bleeding after the initial procedure, unsuccessful reduction of portal venous pressure, elevated portosystemic gradient, and decreased mid-shunt velocity on Doppler imaging during surveillance[12-16]. Once shunt dysfunction has been confirmed, multiple approaches may be adopted: shunt revision with angioplasty, repeat stenting, deployment of endoprosthesis, and/or catheter directed thrombolysis[16,17]. Rarely, a second parallel stent (PS) can be placed to overcome primary TIPS insufficiency and alleviate upper gastrointestinal variceal bleeding or ascites. Here, we report a case series of PS placements in three patients with portal hypertension secondary to alcoholic cirrhosis, alpha-1 antitrypsin deficiency (AATD), and non-alcoholic steatohepatitis (NASH) respectively.
Chief complaints: Vomiting blood and lightheadedness.
History of present illness: A 46-year-old female with alcoholic cirrhosis and esophageal varices presented to the emergency department (ED) with recent 2 episodes of hematochezia. She endorsed nausea and lightheadedness for the past few days, denying hematemesis or coffee-ground emesis. Four months ago, she presented with GI bleeding from esophageal varices and failed repeated esophageal bandings. TIPS and coronary vein varices coil-embolization were performed at that time: Portosystemic gradient (PSG) was reduced from 17 mmHg to 10 mmHg; direct portal pressure decreased from 27 mmHg to 23 mmHg. She was discharged 3 d later. During one-month follow-up after the procedure, she was clinically asymptomatic with adequate flow-velocities in her TIPS (Table 1).
| Status | Patient 1 | Patient 2 | Patient 3 |
| Before TIPS | Child-Pugh B; MELD 11; bilirubin 1.1, INR 1.5, PTT 18.6, albumin 2.6; DV post TIPS: 153 (TIPS), 33 cm/s (MPV). Lactulose 10 g/d | Child-Pugh B; MELD 11; bilirubin 0.7, INR 1.3, PTT 16.6, and albumin 3.5. Rifaximin 550 mg × 2/d, Lactulose 20 g × 3/d | Child-Pugh C; MELD 12; bilirubin 1.6, INR 1.4, PTT 17.1, and albumin 2.5; DV immediately post-TIPS: 96 (TIPS), 89.5 cm/s (MPV). Rifaximin 550 mg × 2/d, Lactulose 30 g/45 mL × 3/d |
| Before PS | Child-Pugh B; MELD 15; bilirubin 4.6, INR 1.3, PTT 17.0, and albumin 2.5; DV: 155 (TIPS), 18 cm/s (MPV). Rifaximin 550 mg × 2/d Lactulose 10 g/d | Child-Pugh B; MELD 10; bilirubin 0.7, INR 1.4, PTT 17.1, and Albumin 2.1; DV 2 wk post-PS: 147 (TIPS), 138 (PS), and 16 cm/s (MPV). Rifaximin 550 mg × 2/d, Lactulose 20 g × 3/d | Child-Pugh C; MELD 13; bilirubin 0.7, INR 1.4, PTT 17.1, and Albumin 2.5; DV: 90.9 (TIPS) 37 cm/s (MPV). Rifaximin 550 mg × 2/d, Lactulose (20 g) 30 mL × 3/d, Piperacillin 4.5 g/6 h |
| 6 mo post-PS | Child-Pugh B; MELD 21; bilirubin 4.5, INR 1.3, PTT 16.5, and albumin 3.5; DV: 78 (TIPS), 144 (PS), 39.3 cm/s (MPV). Rifaximin 550 mg × 2/d Lactulose 10 g/d | Child-Pugh B; MELD 21; bilirubin 2.5, INR 1.5, PTT 18.5, and albumin 2.8; DV: 85.8 (TIPS), 109 (PS), and 83 cm/s (MPV). Rifaximin 550 mg × 2/d, Lactulose 20 g × 3/d | Child-Pugh C; MELD 14; bilirubin 2.1, INR 1.3, PTT 16.7, and albumin 2.0; DV: 72 (TIPS), 92 (PS), and 68 (MPV) cm/s. Rifaximin 550 mg × 2/d, Lactulose (20 g) 30 mL × 3/d |
History of past illness: Chronic pancreatitis;; non-bleeding grade 1 gastric varices status post coronary vein coil-embolization; hypertension; endometriosis.
Personal and family history: No current tobacco, alcohol, or substance use. Family history was non-contributory.
Physical examination upon admission: Mildly jaundiced; abdomen was soft and non-distended; clear bilateral lung sounds, intact neurological exams with appropriate mood and affect.
Laboratory examinations: Hemoglobin: 4.7 g/dL and platelets: 25000/mL consistent with anemia secondary to acute blood loss; abnormal liver function tests (Table 1).
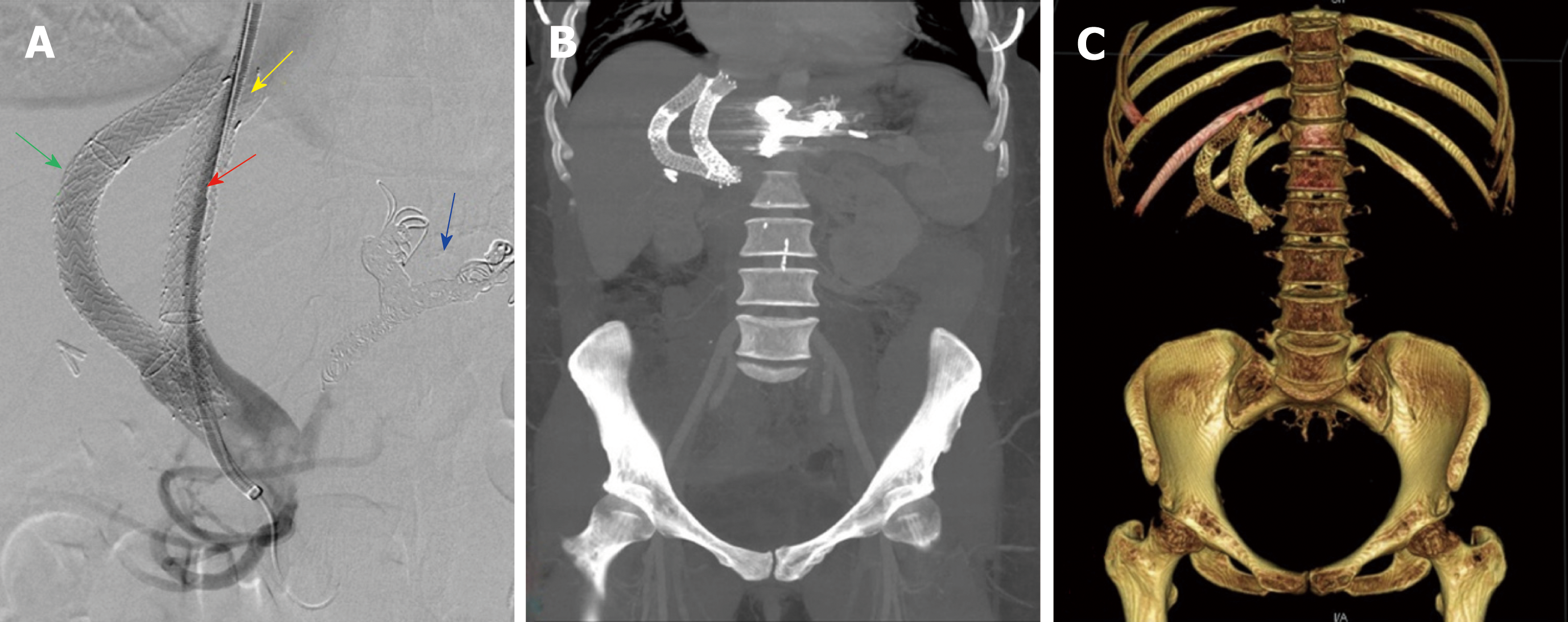
Imaging examinations: Esophagogastroduodenoscopy (EGD) showed blood-filled stomach and type-1 isolated gastric varices. Contrast enhanced computed tomography of the abdomen showed a blood-filled stomach and large gastric wall varices. Four months ago, a 10 mm × 8 cm Viatorr® (GORE, Flagstaff AR, United States) stent was placed from right hepatic vein to the left portal vein with a 4-cm bare metal stent extension for optimal outflow positioning into the inferior vena cava (Figure 1A-C). Doppler ultrasound (US) demonstrated a patent stent with adequate velocities (Table 1).
Kinjal Dave, MD, Assistant Professor of Medicine, Division of Gastroenterology; Jen Rosenau, MD, Assistant Professor of Medicine, Division of Hepatology.
Primary TIPS insufficiency with recurrent variceal bleeding.
Parallel TIPS placement: A TIPS revision procedure demonstrated a widely patent stent and a portosystemic gradient of 9 mmHg. A parallel 10 mm × 8 cm Viatorr® TIPS was inserted to manage continued bleeding, reducing PSG to 4 mmHg. The direct portal pressure remained constant (25 mmHg) before and after the procedure. Patient later developed urinary sepsis and was successfully treated with broad spectrum antibiotics.
Six months later, patient returned to ED reporting progressive abdominal pain and swelling. Both TIPS stents were found to be patent by US (Table 1). No ascites was seen on US.
Chief complaints: Persistent engorged esophageal varices on surveillance EGD.
History of present illness: A 56-year-old male with cirrhosis secondary to AATD status post TIPS was referred to interventional radiology (IR) in June 2017 because of persistent large esophageal varices on EGD. He was clinically asymptomatic at presentation. Previously, he was admitted in April 2017 with abdominal distension, hematemesis and acute blood loss anemia. At that time, US showed large volume ascites and an occluded TIPS stent. In addition to paracentesis and blood transfusion, sharp recanalization of the shunt was performed reducing PSG from 15 mmHg to 10 mmHg. He was discharged 3 d after the May 2017 admission.
History of past illness: Cirrhosis with prior esophageal variceal bleeding status post TIPS in 2009; esophageal banding; hypertension; inguinal hernia; umbilical hernia.
Personal and family history: No tobacco, alcohol, or substance use. Family history was positive for AATD affecting his mother’s lungs.
Physical examination upon admission: Jaundiced; abdomen was soft and non-distended; clear bilateral lung sounds, intact neurological exams with appropriate mood and affect.
Laboratory examinations: Abnormal liver function tests (Table 1).
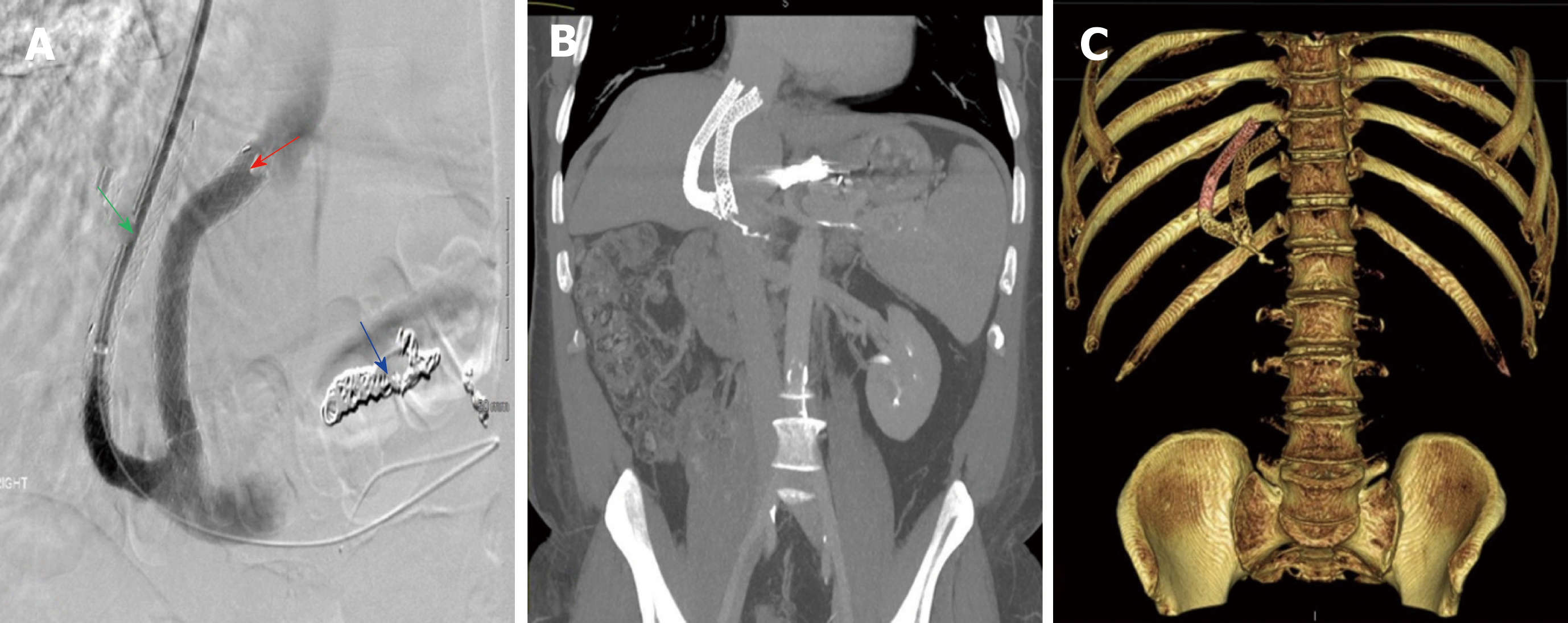
Imaging examinations: Given concern for shunt occlusion, we obviated the TIPS US and proceeded immediately to TIPS revision procedure. The first Viatorr® TIPS stent was inserted directly from the middle hepatic vein. Contrast venography demonstrated patency of the primary TIPS stent. The PSG was 13 mmHg despite 12-mm balloon angioplasty.
Primary TIPS insufficiency with recurrent variceal bleeding.
Parallel TIPS placement: A 10 mm × 10 cm PS Viatorr® TIPS was inserted from right hepatic vein to the confluence of right portal and left portal veins and coronary vein varices were coil embolized (Figure 2A-C). PS reduced PSG from 13 mmHg to 7 mmHg and direct portal pressure from 34 mmHg to 21 mmHg.
Doppler US revealed patency in both stents during 2-wk and 6-mo follow-ups (Table 1). In December 2017, patient presented to ED with worsening bilateral lower extremity edema. Whereas Doppler showed an average velocity of 121 cm/s for the new shunt and 95 cm/s for portal vein, there was markedly decrease flow in the old shunt with a peak velocity of 10 cm/s. IR was consulted to evaluate suspected shunt dysfunction. However, the measured portosystemic gradient of 7 mmHg was deemed adequate, and contrast flow through both stents was excellent. Considering the increased model for end-stage liver disease (MELD) score (Table 1), the patient was evaluated for liver transplant in February 2018 and at that time, his follow-up demonstrated patency of both shunts with the following velocities of 55 cm/s, 60 cm/s, and 66 cm/s for the old shunt, new shunt, and portal vein respectively.
Chief complaints: Hematemesis.
History of present illness: A 54-year-old female with esophageal varices secondary to NASH cirrhosis presented with hematemesis. Initial EGD showed type 2 gastroesophageal varices (GOV2) and endoscopic banding was performed. However, the patient continued having hematemesis and was referred to IR. A 10 mm × 8 cm Viatorr® TIPS was inserted from right hepatic vein to the right portal vein. The procedure decreased PSG from 20 mmHg to 12 mmHg. Doppler US confirmed TIPS patency (Table 1). Five days following the procedure, patient began to experience significant hematemesis.
History of past illness: Type 2 diabetes mellitus, hypertension, gastroesophageal reflux disease, chronic obstructive pulmonary disease, umbilical hernia, hysterectomy.
Personal and family history: No tobacco, alcohol, or substance use. Family history was non-contributory.
Physical examination upon admission: Sclera icteric; abdomen was soft and non-distended; tachypnea, clear bilateral lung sounds, intact neurological exams with appropriate mood and affect.
Laboratory examinations: Hemoglobin 10.95 g/dL, white blood cells 21900/mm3, platelets 84000/mL; abnormal Liver function tests (Table 1).
Imaging examinations: EGD showed recurrent bleeding from GOV2 with no evidence of isolated gastric varices. Doppler US revealed TIPS patency (Table 1).
Sara Pasha, MD, Assistant Professor of Medicine, Department of Internal Medicine-Pulmonary Division; Alla Grigorian, MD, PhD, Assistant Professor of Medicine, Medical Director of Liver Transplant; Terrence Barrett, MD, Professor of Medicine and Microbiology/Immunology, Chief, Division of Digestive Diseases and Nutrition.
Primary TIPS insufficiency with recurrent variceal bleeding.
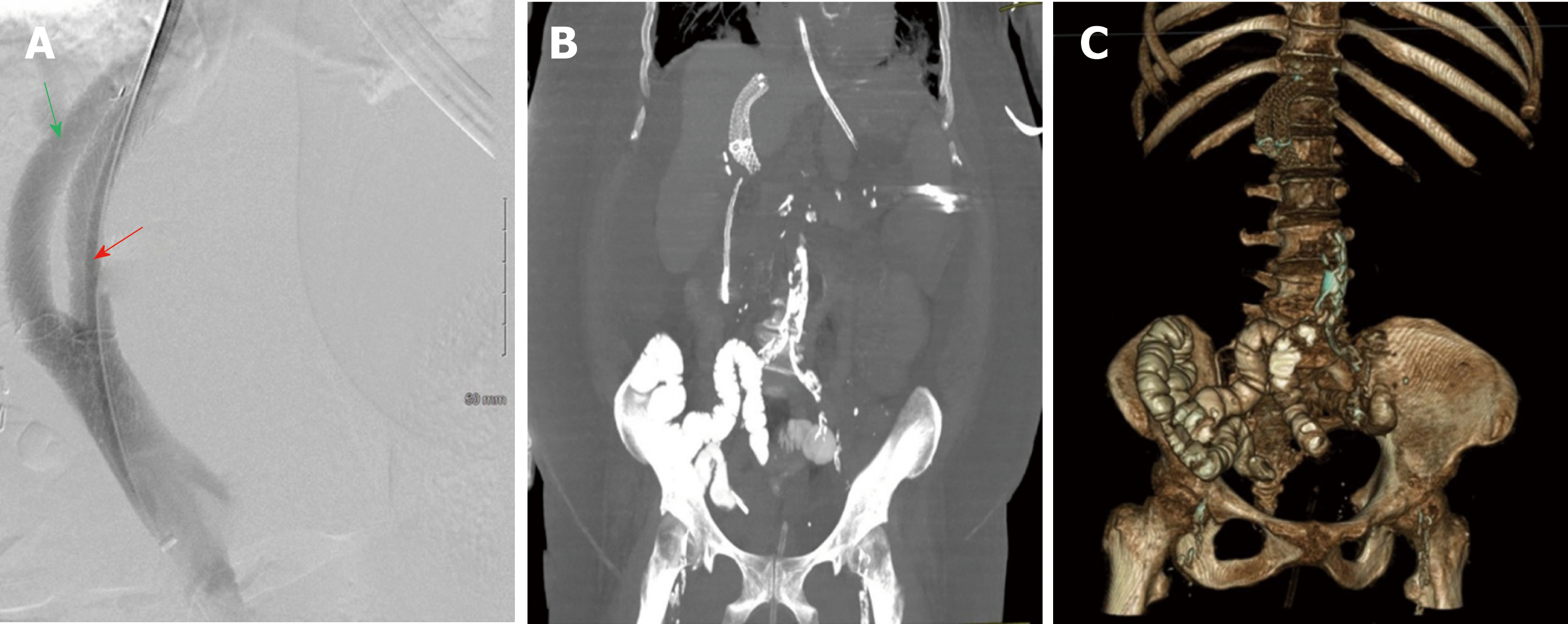
Parallel TIPS placement: Due to recurrent variceal bleed and decompensated cirrhosis, a second 10 mm × 8 cm Viatorr® TIPS was inserted from right hepatic vein to the left portal vein (Figure 3A-C). Procedure was a technical success, decreasing PSG from 9 to 4 mmHg. Direct portal pressure decreased from 40 mmHg to 35 mmHg. Following the procedure, patient developed hypernatremia which was managed with intravenous fluids. Patient was discharged home seven days after.
Six-month US follow-up was unremarkable. Doppler demonstrated patency of both shunts with adequate flow (Table 1).
TIPS failure can either be due to stent occlusion or stenosis, which has become significantly less frequent with the widespread use of covered stents[14,18,19]. This complication can be diagnosed with Doppler imaging and confirmed during TIPS revision procedure[20-24]. However, in the presence of a well-functioning primary stent, the recurrence or persistence of ascites and variceal bleeding can be a therapeutic challenge. We present a short case series to illustrate three patients with portal hypertension who underwent a second TIPS stent placement using Viatorr® stents. This is commonly known as parallel TIPS (PS) or double barrel TIPS. As early as 1990s, the effectiveness of PS in treating shunt insufficiency had been demonstrated along with other options such as re-stenting and balloon angioplasty[25]. In our practice, PS is pursued in symptomatic patients in whom the primary TIPS shunt insufficient or is thrombosed and recanalization techniques have failed.
In our case series, the primary TIPS were insufficient in alleviating portal hypertension symptoms despite their patency being verified during follow-ups and/or before PS placement. Furthermore, the PSGs prior to PS were below 10 mmHg in cases 1 and 3. No laboratory values were predictive of shunt insufficiency or the need for a PS. A study by Haskal et al[13] reported a cohort of 10 out of 93 patients that underwent PS placement. This study alluded to insufficiency of the primary TIPS stent in decreasing the PSG as a predictor for the need of PS placement; the mean post procedural PSG in after the first TIPS was 10.2 ± 3.7 mmHg. In patients who received a PS, the mean post procedural gradient was 19.1 ± 3.8 mmHg after placement of the first TIPS and 12.5 ± 3.5 mmHg after placing a PS[13]. As the previous gradients indicate, the initial TIPS were suboptimal to begin with even at maximum diameter of 10 mm expansion.
A similar trend was observed in another retrospective study, in which 40 out of 338 TIPS patients underwent parallel Wallstent® placement[26]. In this study by Helmy et al[26], PS patients exhibited lower portal pressure gradient drop compared to single TIPS only patients with means of (10.4 ± 5.4 mmHg vs 12.4 ± 7.1 mmHg) after the first TIPS procedure. Whether the patients from these two studies would have benefited from primary shunts with larger diameters to begin with and therefore avoid subsequent PS should be further investigated. In our report, single TIPS were not sufficient for symptomatic relief despite achieving maximum stent expansion, and in cases 1 and 3 despite optimal PSGs. This is similar to Helmy et al[26] patient cohort requiring PS placement despite achieving a mean portal pressure gradient of 7.9 ± 4.8 mmHg after the initial shunt placement. However, as previously mentioned, his study used bare metal stent with its inherent lower patency rate overtime.
Case 2 was secondary to an occluded primary TIPS, though it provided an impressive symptom-free period of 8 years. The successful recanalization of this occluded shunt failed to provide symptomatic relief requiring us to place a PS to further decrease the PSG from 13 mmHg to 7 mmHg. Also, the patient’s MELD score increased from 10 to 21 over the following 6 mo (Table 1); on one hand, patients with AATD tend to have rapidly progressive cirrhosis with extensive inflammation and fibrosis far beyond other causes for cirrhosis[27,28]. On the other hand, excessive shunting of portal venous blood away from liver parenchyma after PS placement may have contributed to worsening liver function. This way addressed in Helmy et al[18] study and they advocated for the use of smaller PS to decrease the risk of hepatic encephalopathy and mortality after PS placement.
In addition to the studies mentioned above, literature on PS is rather limited. More recently, one group reported 18 out of 132 TIPS patients underwent PS placement after primary TIPS stent dysfunction, indicating that shunt patency of 1-year post-PS was higher in the patients who received Fluency® endoprosthesis than those who received Wallgraft® (87.5% vs 70.0%, P = 0.358)[29]. Another study described the application of PS in 10 cases of cirrhotic patients due to hepatitis B infection[30]. Although covered stents were placed for both primary TIPS stent and PS, unfortunately, the authors did not specify the exact type and brand of stents used. Like our cases, most primary TIPS dysfunctions were manifested by symptoms such as ascites and recurrent variceal bleeding rather than surveillance US findings. In addition to the PSG decease after PS placement in both studies (25.5 ± 7.3 mmHg to 10.9 ± 2.3 mmHg, and 35.60 ± 2.72 mmHg to 15.30 ± 3.27 mmHg, respectively), the most common post procedural symptom was hepatic encephalopathy, requiring only medical management with Lactulose and Rifaximin, which were also prescribed for all our patients (Table 1). With average follow-ups of 16.7 ± 10.8 mo and 14.0 ± 1.13 mo, these two studies reported adverse outcomes including worsening liver function, recurrent variceal bleed and death. In comparison, our case series of PS achieved patency at 6-mo follow-up. However, only patient 1 and 3 from our report remained symptom free post-PS for those 6 mo, while patient 2 developed progressive worsening of hepatic function, likely a combination of ATTD progression of the disease and excessive portal blood shunting away from liver parenchyma. In terms of portal hypertensive symptoms, PS successfully prevented recurrent variceal bleeding and ascites in all 3 cases for at least 6-mo follow-up.
A pre-procedural review of abdominal cross-sectional imaging and of the initial TIPS procedure can assist in optimal planning of PS placement. For the patient discussed in case 2, the initial TIPS was placed from the middle hepatic vein to the right main portal vein. This left us ample space for placement of the second TIPS from the right hepatic vein to the left portal vein. As for cases 1 and 3, the first TIPS was placed from the right hepatic vein to the right portal vein. In each case, the origin of the right hepatic vein was peripheral enough into the liver to allow for a new access of the right hepatic vein for a subsequent PS placement into the left portal vein. Overall, placement of a second TIPS stent is not technically challenging after careful review of the hepatic venous anatomy and of the target portal venous branch. The left portal vein can be accessed from the hepatic vein aided by a more acute angle of the TIPS needle to allow a more anterior reach and can be easily targeted from either the right or the middle hepatic veins. We typically avoid placing a PS within the same portal vein of the primary stent to avoid a crowded space that would limit stent expansion. Shunt reduction maybe performed if needed to address medically uncontrollable hepatic encephalopathy, however, this was not observed in our series.
Despite the widespread use of Viatorr® stents in TIPS placement for over 20 years, there are only two reports of use of primary and PS Viatorr® stents placement with limited follow-up data. The first of which is a single case report describing the use of Viatorr® stent for both primary TIPS and PS in an alcoholic cirrhotic patient that initially presented with recurrent variceal bleeding after being lost to follow-up for 3 years[31]. Similar to cases 1 and 3, his PSG was as low as 10 mmHg prior to PS placement and was then reduced to 5 mmHg post-PS. Unfortunately; the authors did not provide clinical or imaging follow-up data. Another case report of two cases described the successful placement of primary and parallel Viatorr® stents in recurrent hydrothorax and ascites respectively. In both instances the PSG at the time was suboptimal at ≥ 12 mmHg prior to PS placement, but with no radiological evidence of primary stent dysfunction. The only follow-up data provided was clinical resolution of hydrothorax and ascites at two and three months respectively. No follow-up Doppler US data was provided on these shunts[23].
In our case series, all patients underwent Viatorr® PS placement for recurrent upper gastrointestinal variceal bleeding despite adequate PSG in two out of three cases. Also, we were fortunate to have follow-up data showing technical and clinical success of up to 6 mo including Doppler US velocities of primary and PS shunts.
To our knowledge, we are the first to report a three-case series with 6-mo follow-up data, using Viatorr® for both primary TIPS and PS placement for the management of recurrent upper gastrointestinal variceal hemorrhage. Patients after TIPS placement should be monitored routinely using Doppler US of the stents to avoid TIPS stent occlusion. Previous studies recommend US follow-up every 3-12 mo after TIPS procedure[18]. Within our institution, shunt patency evaluations are performed at 3 mo, 6 mo, 1 year and yearly thereafter. A mean shunt velocity < 90 cm/s or > 200 cm/s, or a value lower than 30 cm/s in the main portal vein should raise the suspicion of shunt dysfunction[18]. TIPS catheter venography and PSG are performed in patients with suspicious US findings and/or in those with persistent portal hypertensive symptoms despite US evidence of a well-functioning primary TIPS. We pursue a PS in patients with either a non-salvageable primary TIPS or with symptom persistence despite a well-functioning primary TIPS.
In conclusion, the addition of a second Viatorr® TIPS stent to a preexisting primary TIPS stent in patients with recalcitrant upper gastrointestinal variceal hemorrhage after a single Viatorr® stent placement proves insufficient in the control of variceal bleeding despite maintaining adequate patency, is feasible and has promising short term follow-up data. These findings are supported by Haskal et al[13] retrospective data on the role of parallel TIPS stents for primary TIPS insufficiency. And while Haskal’s study used bare metal stents, Bureau et al[19] randomized controlled trial from 2004 supported the superiority and safety of several covered stents over bare metal stents when placed as a primary TIPS. Hence, considering the added design specific advantages of Viatorr® stents when placed as the primary TIPS, their therapeutic value in treating recurrent variceal bleeding after primary shunt insufficiency should be investigated further with a prospective data that addresses this unique cohort of patients in need of parallel TIPS stents for adequate control of their portal hypertension.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
CARE Checklist (2013) statement: The authors have checked the manuscript according to CARE Checklist (2013).
P- Reviewer: Acevedo JG, Garbuzenko DV, Grgurevic I, Procopet B S- Editor: Ma RY L- Editor: A E- Editor: Zhang YL
| 1. | Mallet M, Rudler M, Thabut D. Variceal bleeding in cirrhotic patients. Gastroenterol Rep (Oxf). 2017;5:185-192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Rudler M, Rousseau G, Benosman H, Massard J, Deforges L, Lebray P, Poynard T, Thabut D. Peptic ulcer bleeding in patients with or without cirrhosis: different diseases but the same prognosis? Aliment Pharmacol Ther. 2012;36:166-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Carbonell N, Pauwels A, Serfaty L, Fourdan O, Lévy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004;40:652-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 568] [Cited by in RCA: 527] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 4. | Biecker E. Diagnosis and therapy of ascites in liver cirrhosis. World J Gastroenterol. 2011;17:1237-1248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 58] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Planas R, Montoliu S, Ballesté B, Rivera M, Miquel M, Masnou H, Galeras JA, Giménez MD, Santos J, Cirera I, Morillas RM, Coll S, Solà R. Natural history of patients hospitalized for management of cirrhotic ascites. Clin Gastroenterol Hepatol. 2006;4:1385-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 262] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 6. | Rössle M. TIPS: 25 years later. J Hepatol. 2013;59:1081-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 287] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 7. | Bandali MF, Mirakhur A, Lee EW, Ferris MC, Sadler DJ, Gray RR, Wong JK. Portal hypertension: Imaging of portosystemic collateral pathways and associated image-guided therapy. World J Gastroenterol. 2017;23:1735-1746. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 58] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (3)] |
| 8. | Boyer TD, Haskal ZJ; American Association for the Study of Liver Diseases. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension: update 2009. Hepatology. 2010;51:306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 405] [Article Influence: 27.0] [Reference Citation Analysis (1)] |
| 9. | Shibata D, Brophy DP, Gordon FD, Anastopoulos HT, Sentovich SM, Bleday R. Transjugular intrahepatic portosystemic shunt for treatment of bleeding ectopic varices with portal hypertension. Dis Colon Rectum. 1999;42:1581-1585. [PubMed] |
| 10. | García-Pagán JC, Caca K, Bureau C, Laleman W, Appenrodt B, Luca A, Abraldes JG, Nevens F, Vinel JP, Mössner J, Bosch J; Early TIPS (Transjugular Intrahepatic Portosystemic Shunt) Cooperative Study Group. Early use of TIPS in patients with cirrhosis and variceal bleeding. N Engl J Med. 2010;362:2370-2379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 826] [Cited by in RCA: 842] [Article Influence: 56.1] [Reference Citation Analysis (0)] |
| 11. | Salerno F, Cammà C, Enea M, Rössle M, Wong F. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology. 2007;133:825-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 366] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 12. | Haskal ZJ, Carroll JW, Jacobs JE, Arger PH, Yin D, Coleman BG, Langer JE, Rowling SE, Nisenbaum HL. Sonography of transjugular intrahepatic portosystemic shunts: detection of elevated portosystemic gradients and loss of shunt function. J Vasc Interv Radiol. 1997;8:549-556. [PubMed] |
| 13. | Haskal ZJ, Ring EJ, LaBerge JM, Peltzer MY, Radosevich PM, Doherty MM, Gordon RL. Role of parallel transjugular intrahepatic portosystemic shunts in patients with persistent portal hypertension. Radiology. 1992;185:813-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Angermayr B, Cejna M, Koenig F, Karnel F, Hackl F, Gangl A, Peck-Radosavljevic M; Vienna TIPS Study Group. Survival in patients undergoing transjugular intrahepatic portosystemic shunt: ePTFE-covered stentgrafts versus bare stents. Hepatology. 2003;38:1043-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 78] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Jahangiri Y, Kerrigan T, Li L, Prosser D, Brar A, Righetti J, Schenning RC, Kaufman JA, Farsad K. Risk factors for stent graft thrombosis after transjugular intrahepatic portosystemic shunt creation. Cardiovasc Diagn Ther. 2017;7:S150-S158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Suhocki PV, Lungren MP, Kapoor B, Kim CY. Transjugular intrahepatic portosystemic shunt complications: prevention and management. Semin Intervent Radiol. 2015;32:123-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 92] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 17. | Haskal ZJ, Pentecost MJ, Soulen MC, Shlansky-Goldberg RD, Baum RA, Cope C. Transjugular intrahepatic portosystemic shunt stenosis and revision: early and midterm results. AJR Am J Roentgenol. 1994;163:439-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 139] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Ferral H, Gomez-Reyes E, Fimmel CJ. Post-Transjugular Intrahepatic Portosystemic Shunt Follow-Up and Management in the VIATORR Era. Tech Vasc Interv Radiol. 2016;19:82-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Bureau C, Garcia-Pagan JC, Otal P, Pomier-Layrargues G, Chabbert V, Cortez C, Perreault P, Péron JM, Abraldes JG, Bouchard L, Bilbao JI, Bosch J, Rousseau H, Vinel JP. Improved clinical outcome using polytetrafluoroethylene-coated stents for TIPS: results of a randomized study. Gastroenterology. 2004;126:469-475. [PubMed] |
| 20. | Kanterman RY, Darcy MD, Middleton WD, Sterling KM, Teefey SA, Pilgram TK. Doppler sonography findings associated with transjugular intrahepatic portosystemic shunt malfunction. AJR Am J Roentgenol. 1997;168:467-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 79] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Longo JM, Bilbao JI, Rousseau HP, García-Villareal L, Vinel JP, Zozaya JM, Joffre FG, Prieto J. Transjugular intrahepatic portosystemic shunt: evaluation with Doppler sonography. Radiology. 1993;186:529-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Dodd GD, Zajko AB, Orons PD, Martin MS, Eichner LS, Santaguida LA. Detection of transjugular intrahepatic portosystemic shunt dysfunction: value of duplex Doppler sonography. AJR Am J Roentgenol. 1995;164:1119-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 64] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Feldstein VA, Patel MD, LaBerge JM. Transjugular intrahepatic portosystemic shunts: accuracy of Doppler US in determination of patency and detection of stenoses. Radiology. 1996;201:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 66] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 24. | Chong WK, Malisch TA, Mazer MJ, Lind CD, Worrell JA, Richards WO. Transjugular intrahepatic portosystemic shunt: US assessment with maximum flow velocity. Radiology. 1993;189:789-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 49] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Dabos K, Stanley A, Redhead D, Jalan R, Hayes RC. Efficacy of balloon angioplasty, restenting, and parallel shunt insertion for shunt insufficiency after transjugular intrahepatic portosystemic stent-shunt (TIPSS). Minim Invasive Ther Allied Technol. 1998;7:287-293. |
| 26. | Helmy A, Redhead DN, Stanley AJ, Hayes PC. The natural history of parallel transjugular intrahepatic portosystemic stent shunts using uncovered stent: the role of host-related factors. Liver Int. 2006;26:572-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Hazari YM, Bashir A, Habib M, Bashir S, Habib H, Qasim MA, Shah NN, Haq E, Teckman J, Fazili KM. Alpha-1-antitrypsin deficiency: Genetic variations, clinical manifestations and therapeutic interventions. Mutat Res. 2017;773:14-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 28. | Lomas DA, Evans DL, Finch JT, Carrell RW. The mechanism of Z alpha 1-antitrypsin accumulation in the liver. Nature. 1992;357:605-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 789] [Cited by in RCA: 767] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 29. | Luo X, Nie L, Tsauo J, Wang Z, Tang C, Li X. Parallel shunt for the treatment of transjugular intrahepatic portosystemic shunt dysfunction. Korean J Radiol. 2013;14:423-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 30. | He FL, Wang L, Yue ZD, Zhao HW, Liu FQ. Parallel transjugular intrahepatic portosystemic shunt for controlling portal hypertension complications in cirrhotic patients. World J Gastroenterol. 2014;20:11835-11839. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |