Copyright
©The Author(s) 2017.
World J Hepatol. Jun 28, 2017; 9(18): 823-832
Published online Jun 28, 2017. doi: 10.4254/wjh.v9.i18.823
Published online Jun 28, 2017. doi: 10.4254/wjh.v9.i18.823
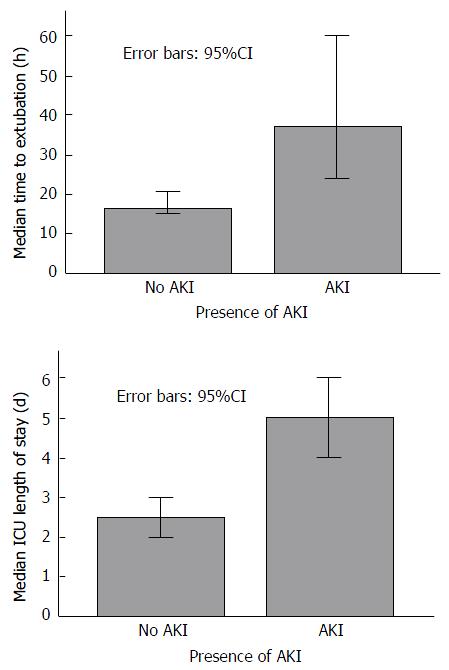
Figure 1 Bar graphs demonstrating median time to extubation and intensive care unit length of stay in the absence or presence of acute kidney injury.
ICU: Intensive care unit; AKI: Acute kidney injury.
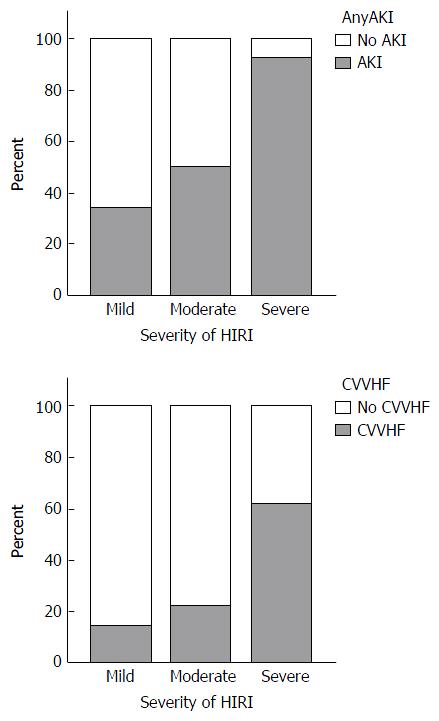
Figure 2 Bar graphs demonstrating the presence of acute kidney injury and use of continuous veno-venous haemofiltration in context of the severity of hepatic ischaemia reperfusion injury.
Mild HIRI n = 35; moderate HIRI n = 68; severe HIRI n = 13. AKI: Acute kidney injury; CVVHF: Continuous veno-venous haemofiltation; HIRI: Hepatic ischaemia reperfusion injury.
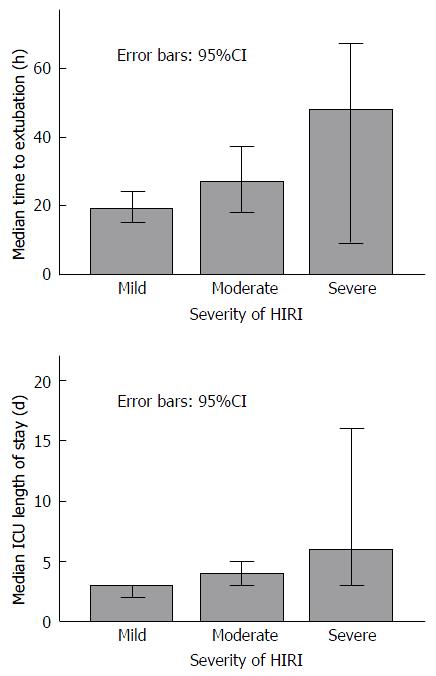
Figure 3 Increasing severity of hepatic ischaemia reperfusion injury compared with median time to extubation and median intensive care unit length of stay.
ICU: Intensive care unit; HIRI: Hepatic ischaemia reperfusion injury.
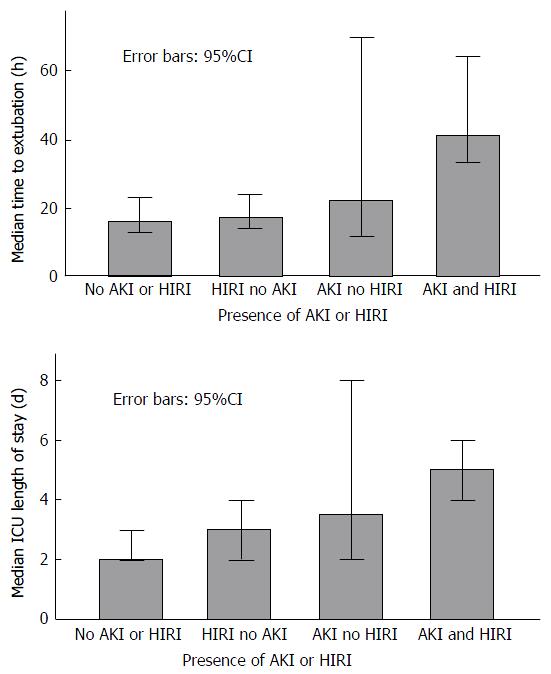
Figure 4 Median time to extubation and median intensive care unit length of stay in groups with the combined absence or presence of acute kidney injury and hepatic ischaemia reperfusion injury.
ICU: Intensive care unit; AKI: Acute kidney injury; HIRI: Hepatic ischaemia reperfusion injury.
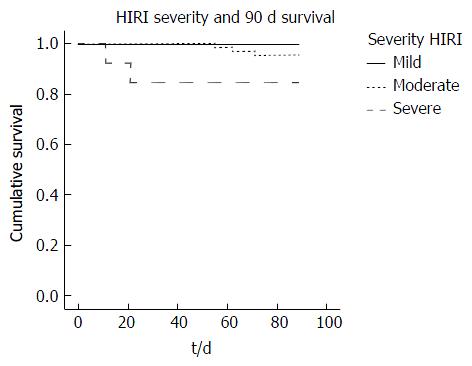
Figure 5 Kaplan Meier plot of 90-d patient survival in those with mild, moderate and severe hepatic ischaemia reperfusion injury.
HIRI: Hepatic ischaemia reperfusion injury.
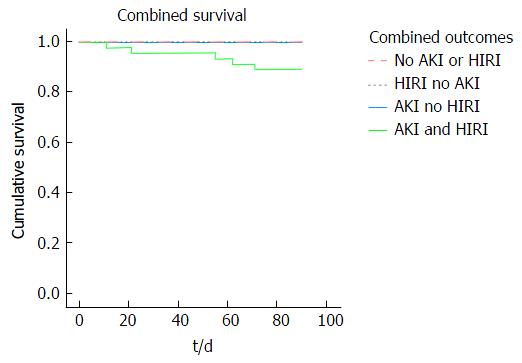
Figure 6 Kaplan Meier plot of 90-d patient survival in those with the combined absence or presence of acute kidney injury and hepatic ischaemia repefusion injury.
AKI: Acute kidney injury; HIRI: Hepatic ischaemia reperfusion injury.
- Citation: Rahman S, Davidson BR, Mallett SV. Early acute kidney injury after liver transplantation: Predisposing factors and clinical implications. World J Hepatol 2017; 9(18): 823-832
- URL: https://www.wjgnet.com/1948-5182/full/v9/i18/823.htm
- DOI: https://dx.doi.org/10.4254/wjh.v9.i18.823