Copyright
©The Author(s) 2016.
World J Hepatol. Jan 28, 2016; 8(3): 162-182
Published online Jan 28, 2016. doi: 10.4254/wjh.v8.i3.162
Published online Jan 28, 2016. doi: 10.4254/wjh.v8.i3.162
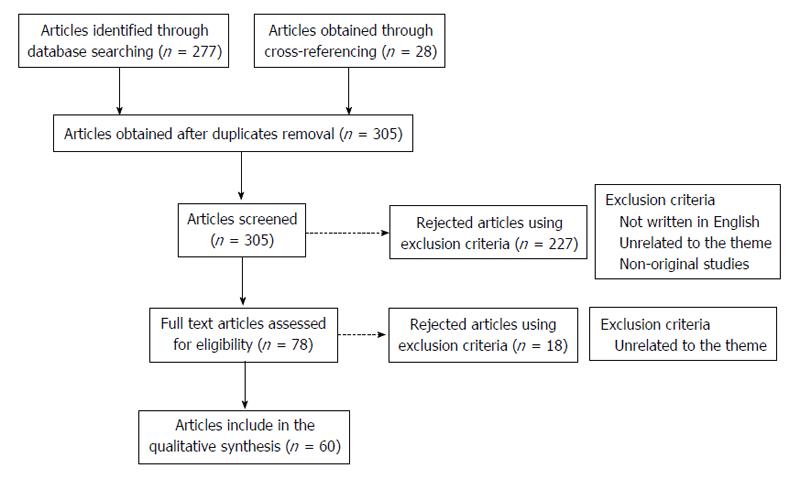
Figure 1 Methods’ flowchart.
A total amount of 277 articles were obtained, on PubMed, through the query [(hepatocarcinoma) OR (hepatocarcinogenesis) OR (hepatic cancer) OR (hepatocellular carcinoma) OR (liver cancer)] AND [(toll like receptors) OR (toll like receptor)]. After discarding the duplicates and adding 28 articles obtained through cross-referencing, 305 articles were available to be screened. The following inclusion criteria were used: (1) studies that were published until the end March 2015; (2) the article should be written in English; and (3) studies relevant to the theme (presenting original data). As exclusion criteria we defined: (1) studies considered by the authors as unrelated to the theme; and (2) non-original studies. These criteria were applied by reading the title and abstract resulting in 227 articles excluded. After this step, the remaining 78 studies were selected for full-text reading. On a second level of eligibility, 18 more studies were excluded and 60 studies were selected, analysed and included in this revision.
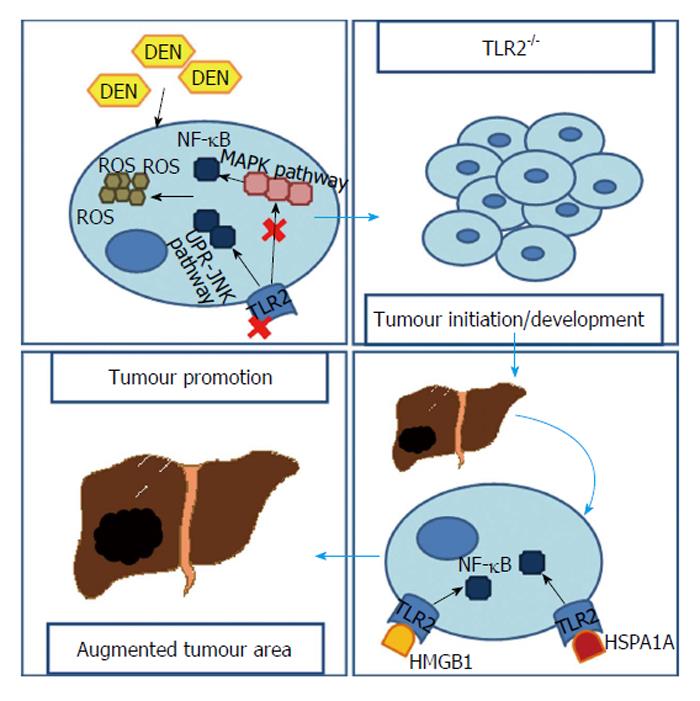
Figure 2 Toll-like receptor 2’s signalling pathways contributing to hepatocarcinoma.
In the absence of TLR2, cells are incapable of responding to an increasing ROS when submitted to DEN. This is the result of an absence of MAPK/NF-κB pathway and an up-regulation of the UPR-JNK pathway. Consequently, cells containing higher ROS and DNA damages have more chances to survive and, HCC develops. In a second stage, where HCC is already established, HMGB1 and HSPA1A released by tumour’s dying cells, through TLR2 stimulation, lead to an NF-κB up-regulation which, in this contest, seems to contribute to tumour’s growth. HCC: Hepatocarcinoma; TLR2: Toll-like receptor 2; ROS: Reactive oxigen species; DEN: Diethylnitrosamine; MAPK: Mitogen-activated protein kinase; NF-κB: Nuclear transcription factor kappa B; UPR: Unfold protein response; JNK: Junamino-terminal kinase; HMGB1: High mobility group box 1; HSPA1A: Heat shock protein A1A.
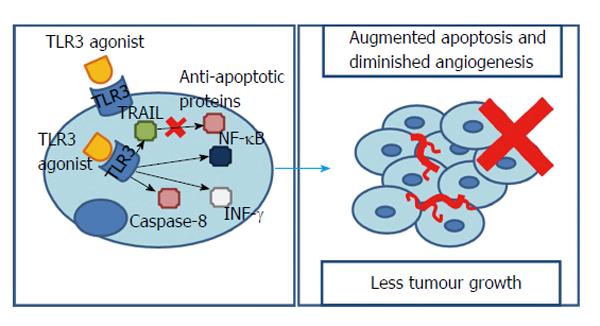
Figure 3 How toll-like receptor 3 stimulus works against hepatocarcinoma.
Stimulation of intracellular TLR3 is able to elicit cell apoptosis in a TRAIL-dependent manner that synergistically accompanies a down-regulation of anti-apoptotic proteins. Additionally, TLR3 stimulus can promote either an inflammatory or an apoptotic response. The first one pending on NF-κB, the second in caspase-8 activation and INF-γ release. As a result, TLR3 works as a protector against cancer which stimulation results in diminished tumour growth. TLR3: Toll-like receptor 3; TRAIL: Tumour necrosis factor-related apoptosis-inducing ligand; INF-γ: Interferon gamma; NF-κB: Nuclear transcription factor kappa B.
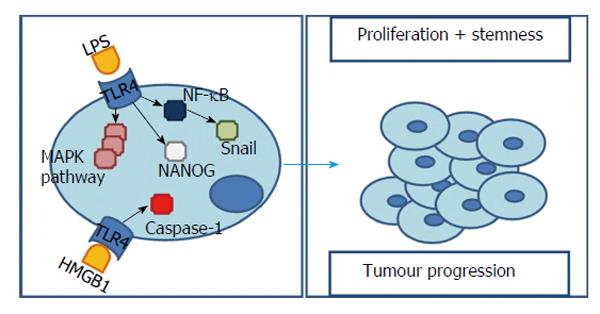
Figure 4 Toll-like receptor 4’s signalling pathways influencing hepatocarcinogenesis.
Bacterial LPS is capable of initiate TLR4 signalling and subsequently activate NF-κB and MAPK signalling pathways. In one hand, in a HCC cell line incubated with bacterial LPS both TLR4 expression and MAPK signalling pathways are significantly augmented, contributing to cell survival and proliferation. On the other hand, TLR4 over-expression contributes to an EMT through MAPKs pathway and Snail. Additionally, NANOG induces TICs’ formation. Both are considered to be the molecular basis of tumour cell infiltration and metastasis. HMGB1’s stimulation of TLR4 with caspase-1 activation is related with maturation of pro-inflammatory cytokines and consequent tumorigenesis and tumour progression. TLR4: Toll-like receptor 4; LPS: Lipopolysaccharides; HCC: Hepatocarcinoma; MAPK: Mitogen-activated protein kinase; EMT: Epithelial-mesenchymal transition; TICs: Tumour-initiating stem-like cells; NF-κB: Nuclear transcription factor kappa B; HMGB1: High mobility group box 1.
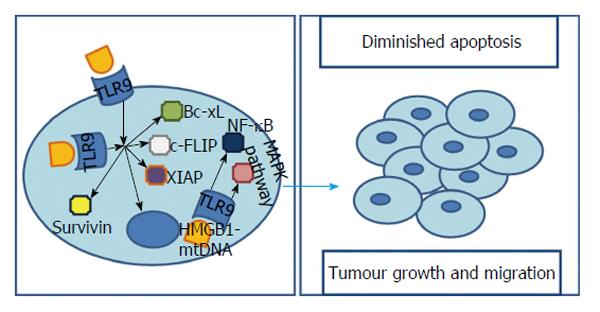
Figure 5 Toll-like receptor 9’s signalling pathways influencing hepatocarcinoma.
TLR9 is present not only in the cytoplasm but also on cells’ membrane. However, it is still controversial whether cytoplasmatic stimulation results in increased cell viability. Independently, membrane receptors’ stimulation results, not only, in up-regulation of apoptosis inhibitors such as survivin, Bcl-xL, XIAP and c-FLIP, but also, in a modulation of oncogenic genes with a major contribution in tumorigenesis and cancer progression. Additionally, a cytoplasmatic HMGB1-mtDNA interaction was proved to be capable of activating TLR9 and MAPK pathway as well as NF-κB leading to augmented survival, growth, proliferation, differentiation and migration of cancer cells. TLR9: Toll-like receptor 9; XIAP: X-linked inhibitor of apoptosis protein; c-FLIP: Cellular FLICE-Like inhibitory protein; MAPK: Mitogen-activated protein kinase; NF-κB: Nuclear transcription factor kappa B; HMGB1: High mobility group box 1.
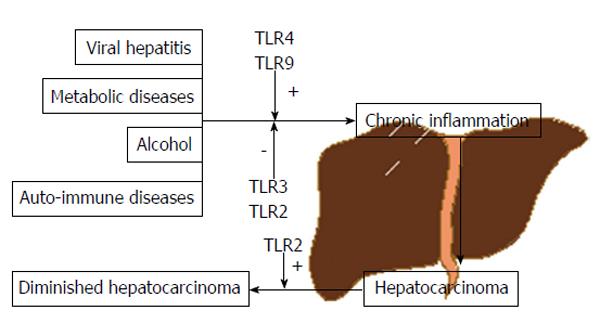
Figure 6 Toll-like receptors influence on the pathway to hepatocarcinoma.
Several factors are known to contribute to the carcinogenic process including viral hepatitis, alcohol, auto-immune or metabolic diseases, among others and the link between all this factors is chronic inflammation which, in turn, is an important hepatocarcinoma’s percursor. Moreover, innate immunity represents an important player in this equation with TLRs such as 4 and 9 having, mainly, a positive contribution to hepatocarcinogenesis and TLR3, essentially, a negative/protective one. TLR2 still presents an ambiguous role, possibly depending on liver’s stage in the inflammation-cirrhosis-carcinoma axis to exert its pro-tumorigenic or anti-tumorigenic capacity. TLR: Toll-like receptor.
- Citation: Lopes JAG, Borges-Canha M, Pimentel-Nunes P. Innate immunity and hepatocarcinoma: Can toll-like receptors open the door to oncogenesis? World J Hepatol 2016; 8(3): 162-182
- URL: https://www.wjgnet.com/1948-5182/full/v8/i3/162.htm
- DOI: https://dx.doi.org/10.4254/wjh.v8.i3.162