Copyright
©The Author(s) 2015.
World J Hepatol. Jul 8, 2015; 7(13): 1730-1734
Published online Jul 8, 2015. doi: 10.4254/wjh.v7.i13.1730
Published online Jul 8, 2015. doi: 10.4254/wjh.v7.i13.1730
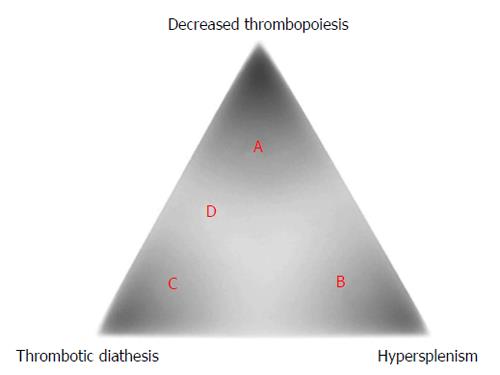
Figure 1 Theoretically ideal therapies against cirrhosis-related thrombocytopenia depending on the etiology.
The platelet count in cirrhotics is determined mainly by three major factors, including (A) a rate of thrombopoiesis, (B) the presence/abscence of hypersplenism, and (C) the presence/abscence of thrombotic diathesis, which differently affect each case. Patients with thrombocytopenic conditions A, B, or C are considered to respond well to thrombopoietin receptor agonists, splenectomy, and anti-platelet/coagulation drugs, respectively. In patients with condition D, a combination of thrombopoietin receptor agonists and anti-platelet/coagulation drugs is thought to be necessary.
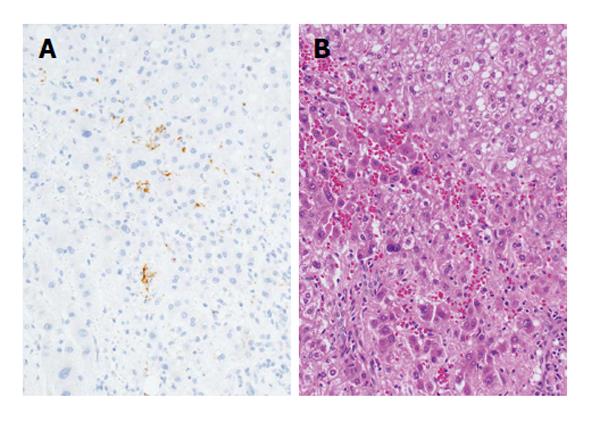
Figure 2 Platelet aggregation in a cirrhotic liver.
A: Immunohistochemical findings. Platelets are stained in brown. (Immunoperoxidase for CD41; original magnification, × 400); B: The corresponding histological findings. Platelets cannot be identified in this photomicrograph. (Hematoxylin-eosin; original magnification, × 400).
- Citation: Ikura Y, Osuga T. Changing common sense: Anti-platelet/coagulation therapy against cirrhosis. World J Hepatol 2015; 7(13): 1730-1734
- URL: https://www.wjgnet.com/1948-5182/full/v7/i13/1730.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i13.1730