Copyright
©2013 Baishideng Publishing Group Co.
World J Hepatol. Aug 27, 2013; 5(8): 417-424
Published online Aug 27, 2013. doi: 10.4254/wjh.v5.i8.417
Published online Aug 27, 2013. doi: 10.4254/wjh.v5.i8.417
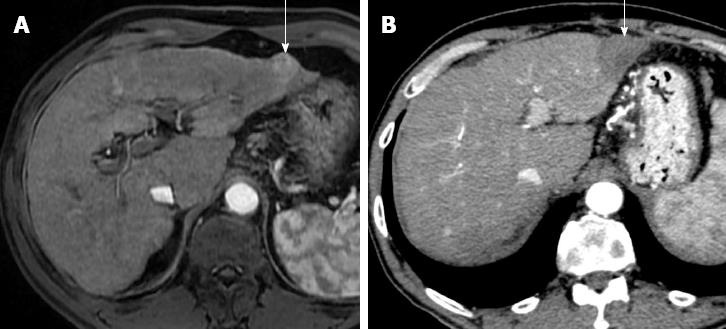
Figure 1 Successful hepatocellular carcinoma resection with radiofrequency tissue coagulation device.
A: Pretreatment arterial phase T1-weighted gradient-echo magnetic resonance shows hypervascular hepatocellular carcinoma (HCC) (arrow); B: On arterial phase computed tomography obtained 4 mo after treatment no hypervascular focus is evident (arrow). Note that resected area is larger to preexisting HCC.
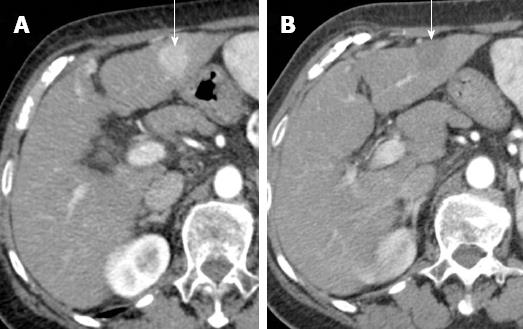
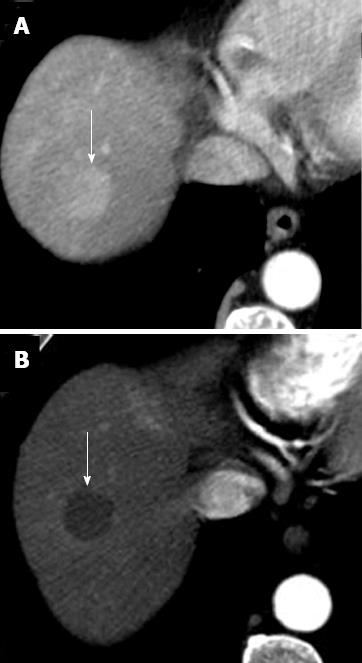
Figure 2 Complete necrosis after radiofrequency ablation for hepatocellular carcinoma.
A: Pretreatment arterial phase computed tomography (CT) shows hypervascular hepatocellular carcinoma (arrow); B: Arterial phase CT obtained 1 mo after treatment shows ablated area (arrow). Absence of arterial enhancement suggests complete tumor necrosis.
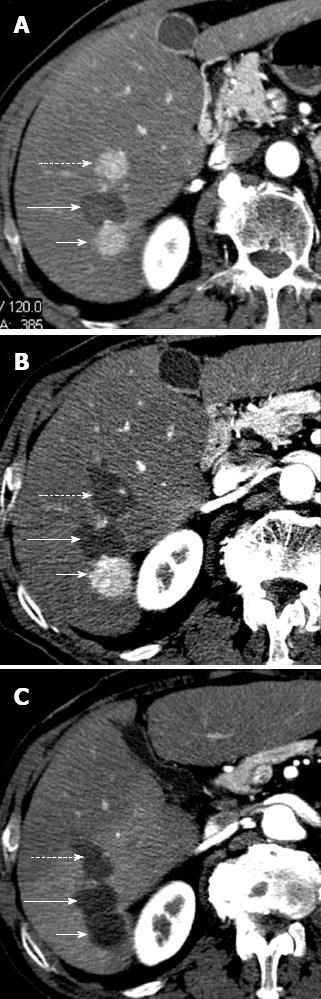
Figure 3 Hepatocellular carcinoma after multiple radiofrequency ablations.
A: Arterial phase computed tomography (CT) obtained 8 mo after radiofrequency ablation shows two new enhancing hepatocellular carcinoma (HCC) nodules located anteriorly (dotted arrow) and posteriorly (short arrow) to ablated HCC (long arrow). These findings suggest occurrence of new HCC nodules; B: Arterial phase CT obtained 2 mo after additional radiofrequency (RF) ablation shows that HCC nodule located anteriorly (dotted arrow) has been replaced by a hypoattenuating, non enhancing area (arrow) that is larger than preexisting tumor. These findings suggest complete necrosis. Posteriorly located HCC (short arrow) increased in size; C: Arterial phase CT obtained 2 mo after posterior. HCC had been replaced by a hypoattenuating, nonenhancing ablation area as a result of additional RF ablation. This example shows that RF ablation is a repeatable procedure.
Figure 4 Perfusion alteration after radiofrequency ablation for hepatocellular carcinoma.
A: Arterial phase computed tomography (CT) obtained 1 mo after treatment shows ablated zone (dotted arrow) and a semilunar enhancing area (solid arrow) medial and anterior to ablated zone; B: Delayed phase CT shows persistent enhancement of the semilunar area (solid arrow), suggesting that the arterial enhancement is due to perfusion alteration rather than residual tumor.
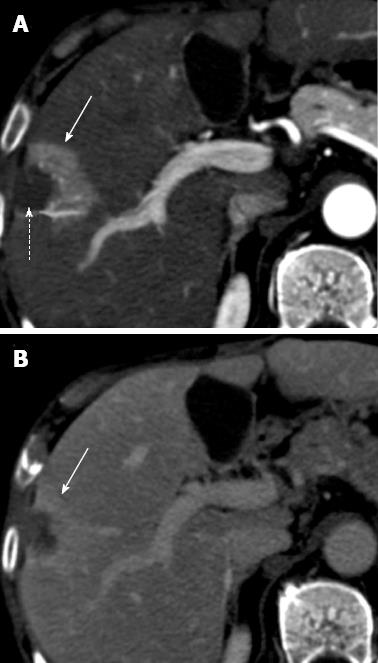
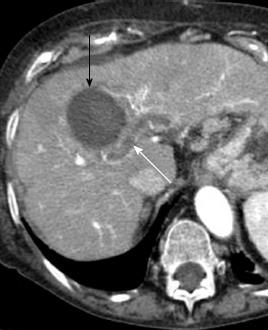
Figure 5 Portal vein thrombosis after radiofrequency ablation for hepatocellular carcinoma.
Arterial phase computed tomography obtained 1 mo after radiofrequency ablation shows a non enhancing thrombus in intrahepatic portal vein (white arrow), in proximity of ablated area (black arrow).
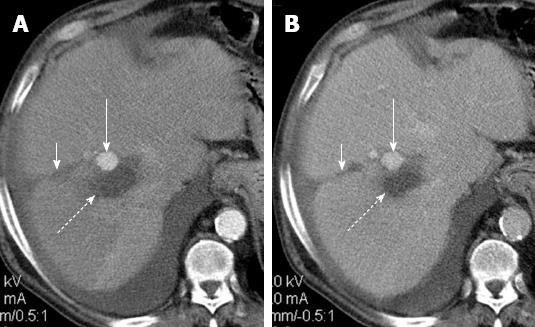
Figure 6 Arterial pseudoaneurysm after radiofrequency ablation for hepatocellular carcinoma.
Post-treatment arterial phase (A) computed tomography (CT) shows a round enhancing area (long arrow) anterior to ablated zone (dotted arrow) with persistent enhancement on portal venous phase (B) CT. Round shape, isoattenuation to aorta and absence of wash-out suggest diagnosis of iatrogenic pseudoaneurysm. Note probe track (short arrow on A and B).
Figure 7 Tumor seeding after radiofrequency ablation for hepatocellular carcinoma.
Arterial phase computed tomography shows heterogeneously enhancing hepatocellular carcinoma tissue (arrow) invading muscles of the anterior abdominal wall along needle tract.
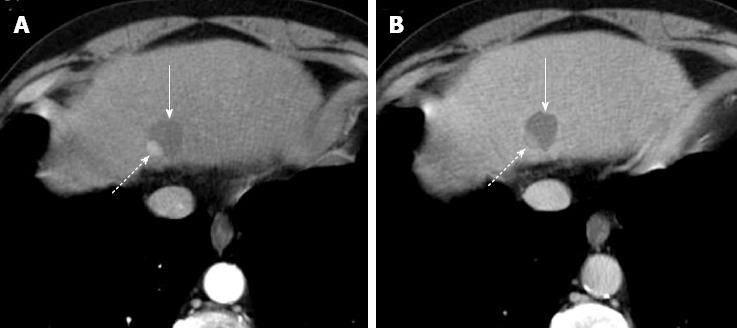
Figure 8 Incomplete hepatocellular carcinoma necrosis after percutaneous ethanol injection.
Arterial (A) and portal venous (B) computed tomography obtained 1 mo after treatment shows that approximately 10%-20% of the tumor, located in the dorsal and lateral portion of the treated, hypoattenuating area, is still viable as demonstrated by the presence of enhancement in arterial phase and hypoattenuation (“washout”) on portal venous phase (dotted arrow on A and B). The majority of tumor (solid arrow) does not show enhancement as a result of the treatment.
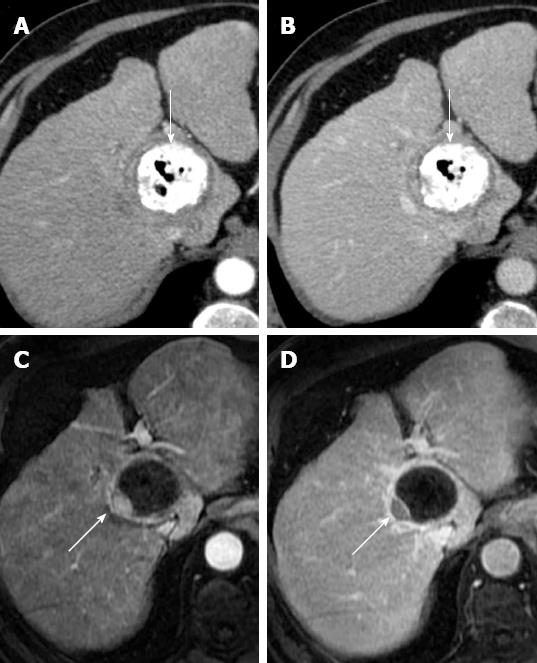
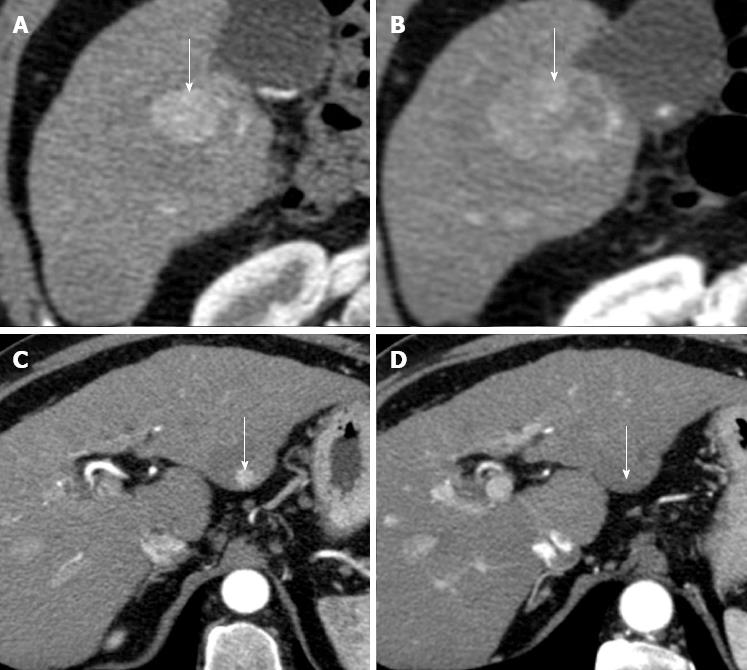
Figure 9 Incomplete hepatocellular carcinoma necrosis after transarterial chemoembolization.
Arterial (A) and portal venous (B) phase computed tomography (CT) obtained 1 mo after transarterial chemoembolization (TACE) shows that hepatocellular carcinoma (HCC) is entirely replaced by Lipiodol accumulation (arrow). No evidence of residual tumor was found. Arterial (C) and portal venous (D) phase T1-weighted gradient-echo magnetic resonance (MR) obtained 1 wk after CT shows residual viable tumor (arrow) in the posterolateral portion of the tumor. This case shows higher accuracy of MR in comparison to CT in assessing HCC response after TACE.
Figure 10 Complete hepatocellular carcinoma necrosis after transarterial chemoembolization with drug-eluting beads.
A: Pretreatment arterial phase computed tomography (CT) shows a hypervascular hepatocellular carcinoma (HCC) (arrow); B: Arterial phase CT obtained 3 mo after transarterial chemoembolization shows a hypoattenuating, non enhancing nodule (arrow). Absence of arterial enhancement suggests complete HCC necrosis.
Figure 11 Hepatocellular carcinomas after sorafenib.
A: Pretreatment arterial phase computed tomography (CT) shows a large hypervascular hepatocellular carcinoma (HCC) (arrow) in right hepatic lobe; B: Arterial phase CT obtained at the same level of A, 9 mo after the start of sorafenib, shows increase in size of HCC (arrow); C: Pretreatment arterial phase CT image shows a second, small hypervascular HCC (arrow) arising within a larger hypoattenuating dysplastic nodule in left hepatic lobe; D: Arterial phase CT obtained at the same level of C, 9 mo after the start of sorafenib, shows disappearance of HCC enhancement (arrow). This case shows that different HCC response to sorafenib may occur in the same patient.
- Citation: Agnello F, Salvaggio G, Cabibbo G, Maida M, Lagalla R, Midiri M, Brancatelli G. Imaging appearance of treated hepatocellular carcinoma. World J Hepatol 2013; 5(8): 417-424
- URL: https://www.wjgnet.com/1948-5182/full/v5/i8/417.htm
- DOI: https://dx.doi.org/10.4254/wjh.v5.i8.417