Copyright
©2013 Baishideng Publishing Group Co.
World J Hepatol. May 27, 2013; 5(5): 288-291
Published online May 27, 2013. doi: 10.4254/wjh.v5.i5.288
Published online May 27, 2013. doi: 10.4254/wjh.v5.i5.288
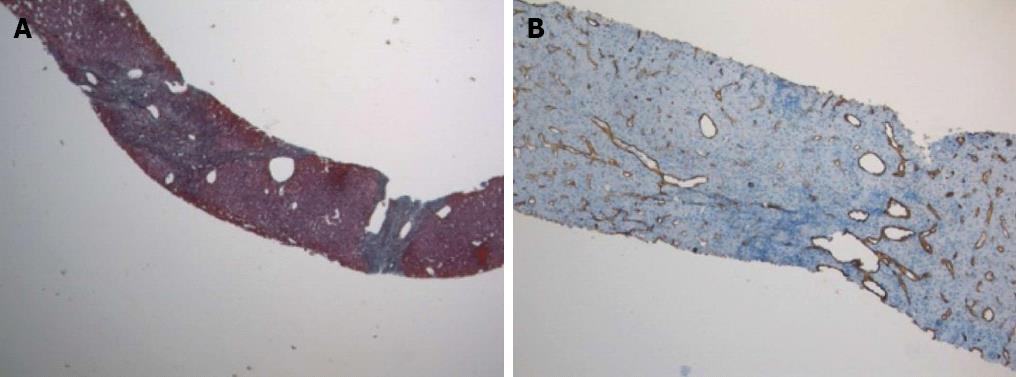
Figure 1 Focal nodular hyperplasia.
A: Fibrous septa (green) giving a nodular appearance to liver parenchyma. Masson’s trichrome staining; original magnification × 40; B: Diffuse CD34 positive immunostaining in the sinusoids; original magnification × 100.
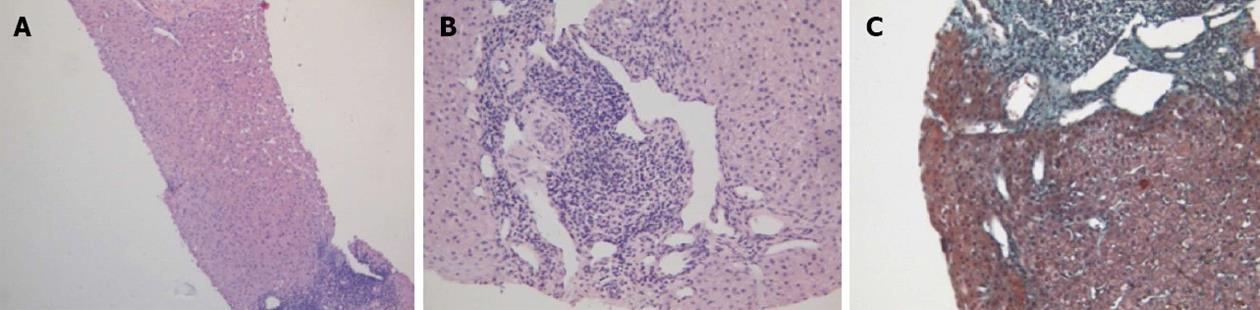
Figure 2 Hereditary hemorrhagic telangiectasia.
Liver parenchyma, devoid of fibrous intra-parenchimal septa, with widespread angiectases in portal and peri-portal areas. A: Hematoxylin-eosin staining; original magnification × 100; B: Hematoxylin-eosin staining; original magnification × 200; C: Masson’s trichrome staining; original magnification × 400.
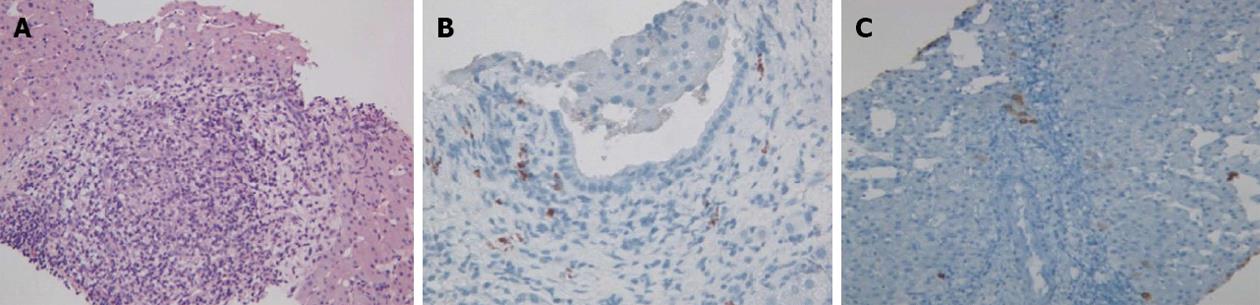
Figure 3 Primary biliary cirrhosis.
A: Intra-portal granuloma. Hematoxylin-eosin staining; original magnification × 200; B: Portal immunoglobulin M (IgM) lymphoplasmacytic infiltrate and bile duct damage. IgM immunostaining; original magnification × 400; C: Absence of cytokeratin 7 (CK7) positive bile ducts in some portal tracts. CK7 immunostaining; original magnification × 200.
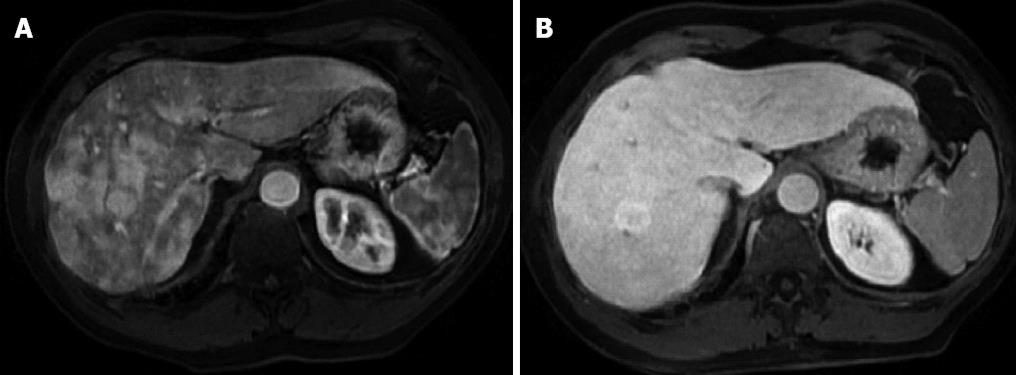
Figure 4 Magnetic resonance.
A: Fat saturation gradient echo T1-weighted hepatic arterial phase magnetic resonance (MR) shows multiple ill defined hypervascular areas in the the right liver lobe, due to arterovenous shunts, and a round, clearly visible, 3 cm lesion surrounded by a hypointense halo; B: On hepatobiliary phase MR, arteriovenous shunt are no longer visible, while lesion, proven to be focal nodular hyperplasia at core biopsy, is hyperintense in comparison to surrounding liver parenchyma.
- Citation: Macaluso FS, Maida M, Alessi N, Cabibbo G, Cabibi D. Primary biliary cirrhosis and hereditary hemorrhagic telangiectasia: When two rare diseases coexist. World J Hepatol 2013; 5(5): 288-291
- URL: https://www.wjgnet.com/1948-5182/full/v5/i5/288.htm
- DOI: https://dx.doi.org/10.4254/wjh.v5.i5.288