Copyright
©The Author(s) 2025.
World J Hepatol. Aug 27, 2025; 17(8): 108772
Published online Aug 27, 2025. doi: 10.4254/wjh.v17.i8.108772
Published online Aug 27, 2025. doi: 10.4254/wjh.v17.i8.108772
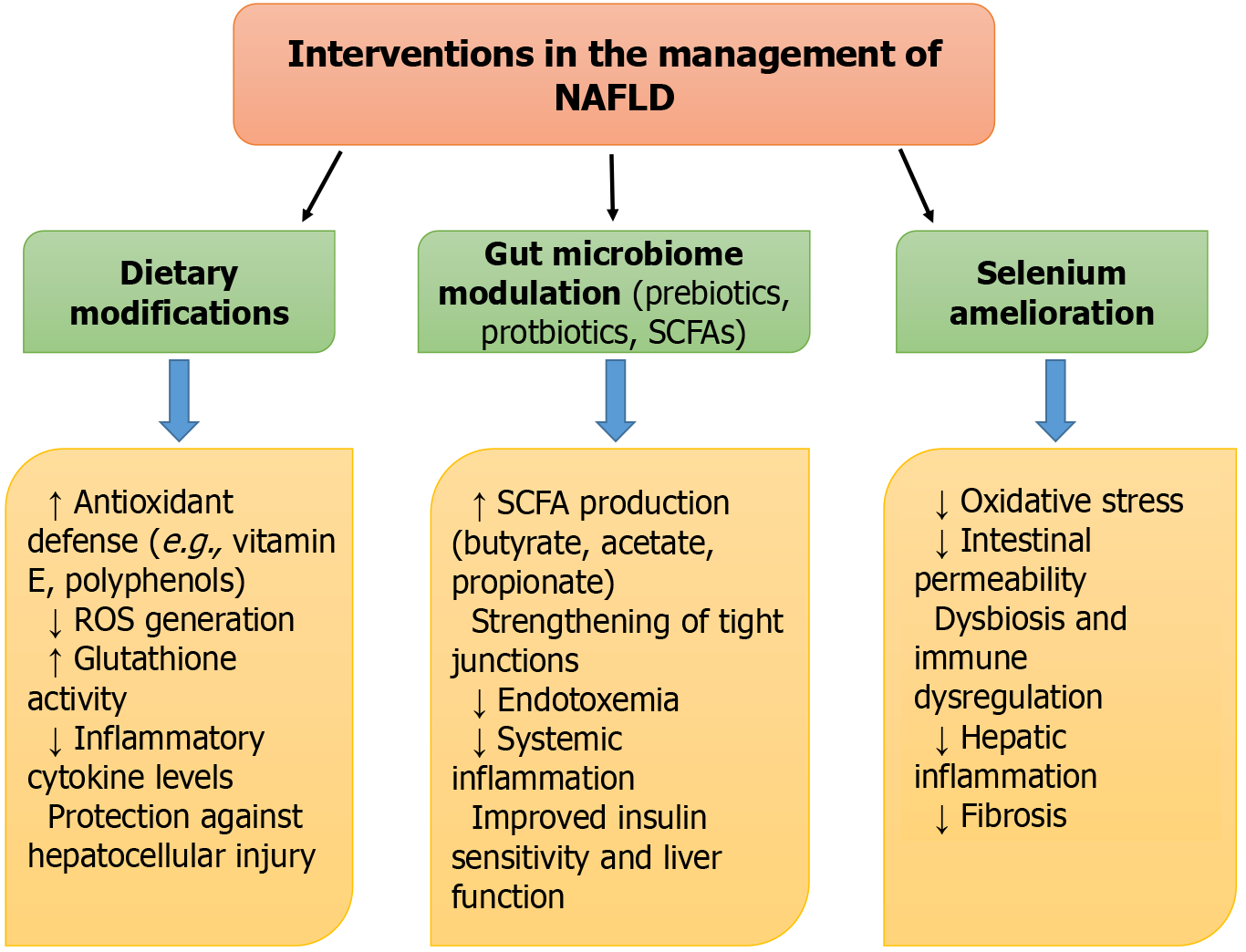
Figure 1 Progression of gut-liver axis dysfunction in non-alcoholic fatty liver disease.
This panel demonstrates the pathophysiological cascade resulting from gut dysbiosis, leading to non-alcoholic fatty liver disease (NAFLD). Disruption of the gut barrier increases intestinal permeability, allowing microbial endotoxins such as lipopolysaccharide to translocate into systemic circulation. This triggers immune activation involving macrophages, promoting the release of pro-inflammatory cytokines (e.g., tumor necrosis factor-α and interleukin-6). The resulting hepatic inflammation and insulin resistance drive the progression from a healthy liver to steatosis and non-alcoholic steatohepatitis. The figure underscores the critical role of the gut-liver axis in NAFLD pathogenesis. NAFLD: Non-alcoholic fatty liver disease; SCFA: Short-chain fatty acid; ROS: Reactive oxygen species.
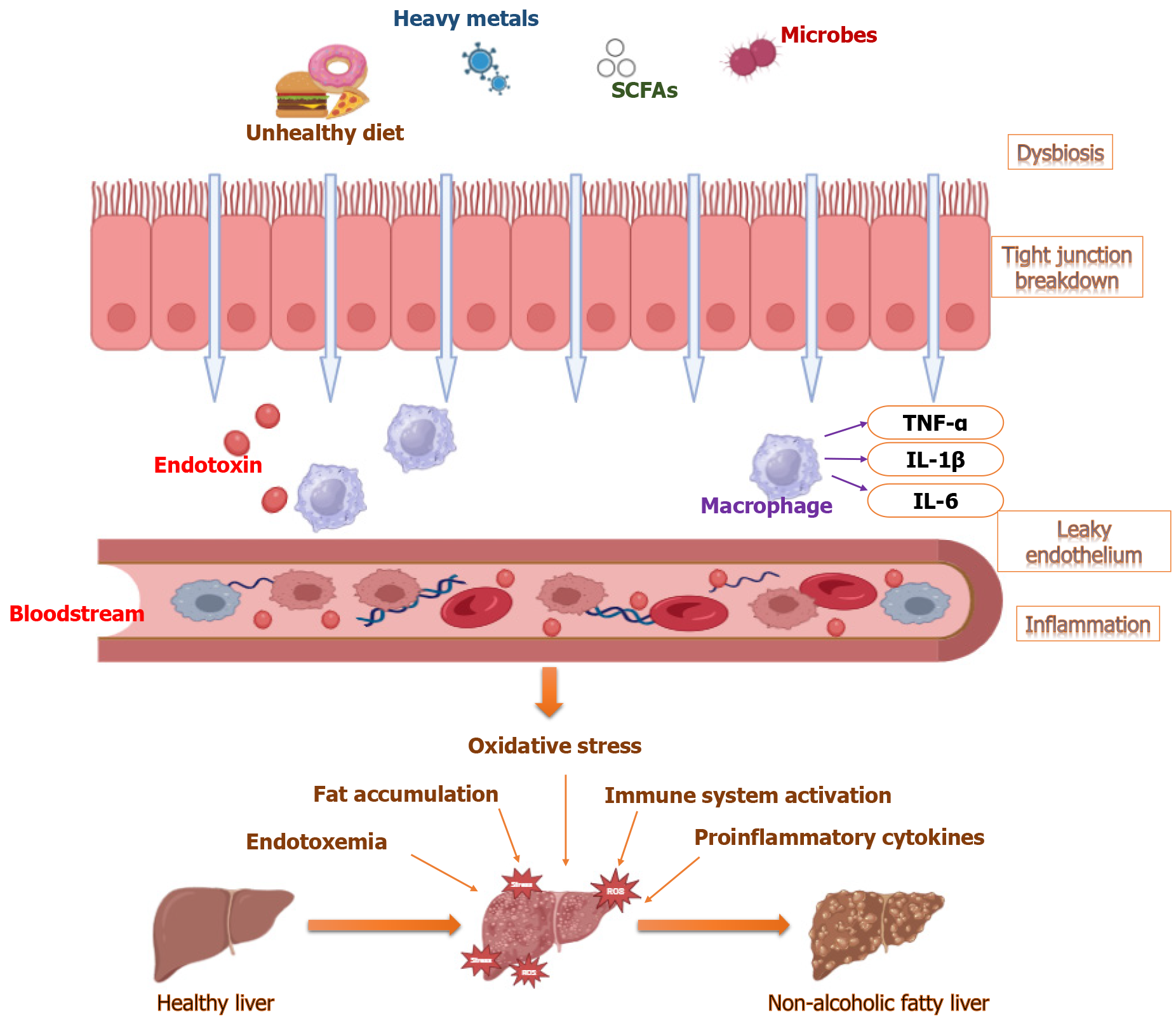
Figure 2 Intervention in the management of non-alcoholic fatty liver disease.
The figure highlights various therapeutic interventions aimed at restoring gut and liver health, including dietary modifications incorporating antioxidants and hepatoprotective nutrients, microbiome-targeted approaches using probiotics and postbiotics like short-chain fatty acids, and the use of essential metal, Selenium. These strategies collectively help in enhancing gut integrity, reducing inflammation, and improving metabolic outcomes. SCFA: Short-chain fatty acid; IL-6: Interleukin-6; IL-1β: Interleukin-1β.
- Citation: Sharma T, Kaushal N, Garla R. Toxins to treatments: Impact of environmental pollutants, gut microbiota, and natural compounds on non-alcoholic fatty liver disease progression. World J Hepatol 2025; 17(8): 108772
- URL: https://www.wjgnet.com/1948-5182/full/v17/i8/108772.htm
- DOI: https://dx.doi.org/10.4254/wjh.v17.i8.108772