Copyright
©The Author(s) 2024.
World J Hepatol. Mar 27, 2024; 16(3): 316-330
Published online Mar 27, 2024. doi: 10.4254/wjh.v16.i3.316
Published online Mar 27, 2024. doi: 10.4254/wjh.v16.i3.316
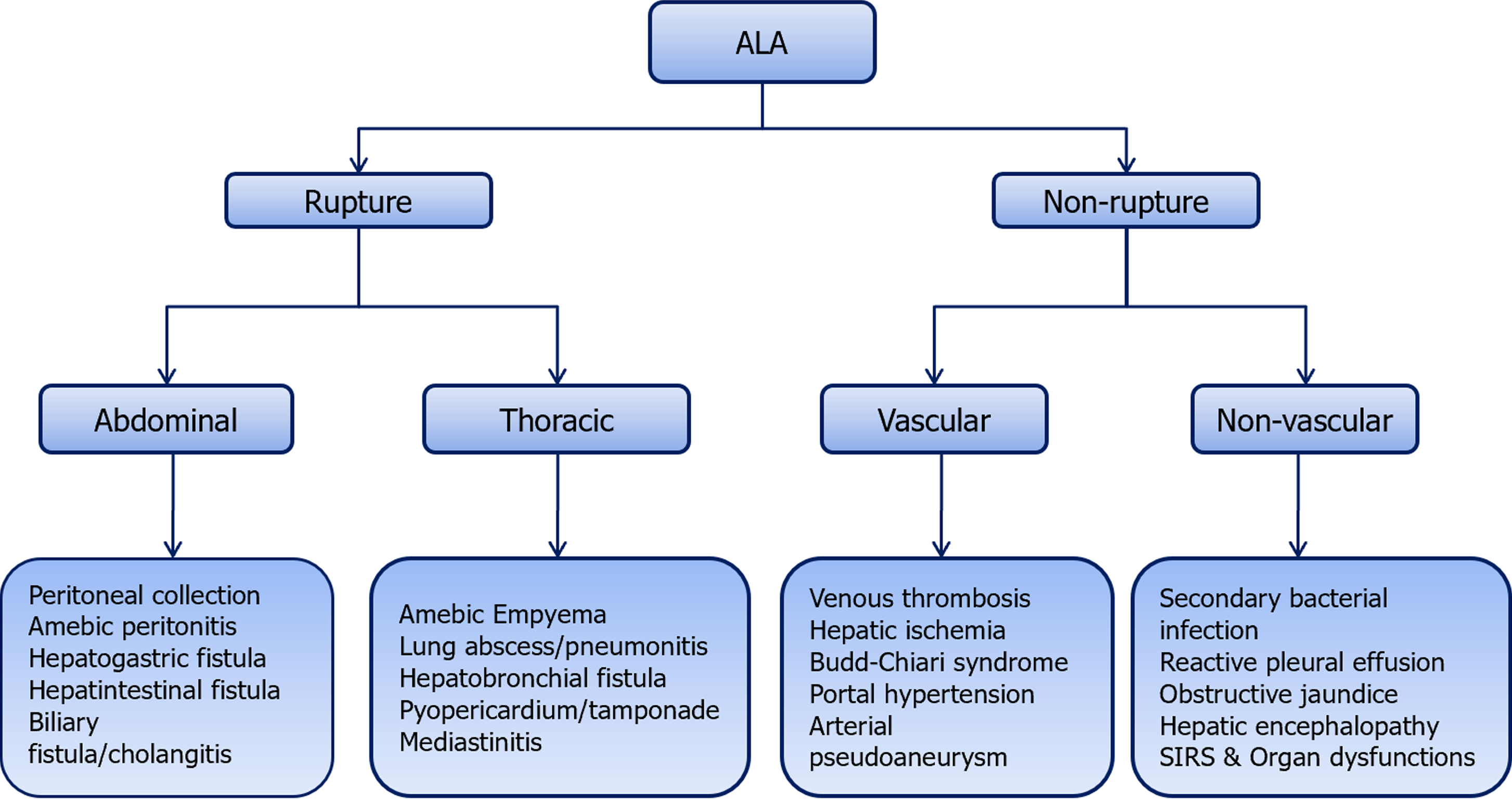
Figure 1 Complications of amebic liver abscess.
The complications can be broadly divided into two groups: Those related to amebic liver abscess rupture and those that are not. The common complications included rupture into the adjacent structures, vascular thrombosis, and secondary bacterial infection. ALA: Amebic liver abscess; SIRS: Systemic inflammatory response syndrome.
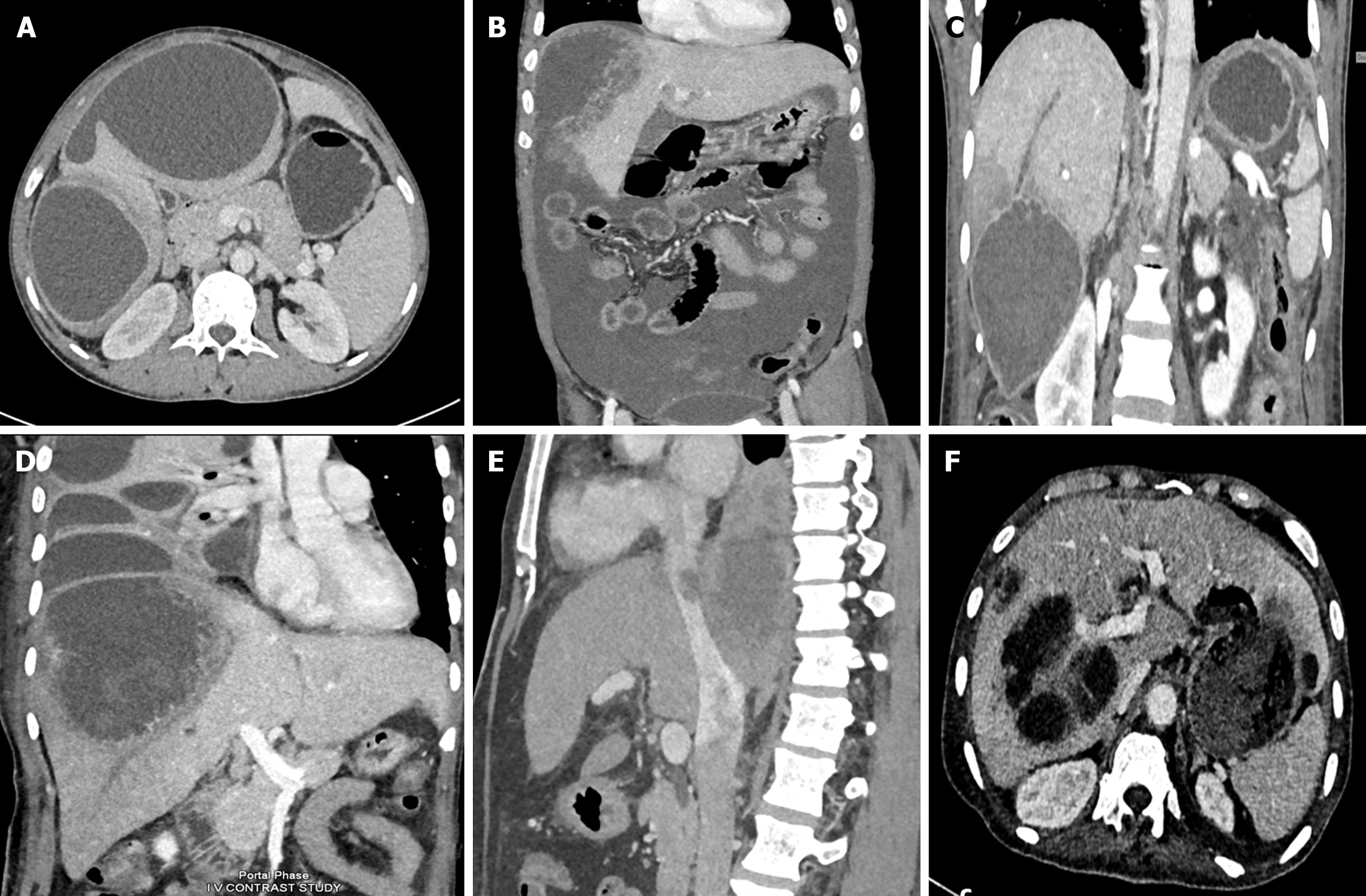
Figure 2 Computed tomographic scans showing various spectrum of complicated amebic liver abscess.
A: Axial computed tomography (CT) scan showing a contained rupture of an abscess with localized fluid collection in the perihepatic area. There is a thin enhancing rim around the abscess, characteristic of a type II amebic liver abscess (ALA); B: Coronal CT scan of a 54-year-old male showing rupture of the abscess with intraperitoneal fluid collection diffusely spreading throughout the entire peritoneal cavity, indicative of free abscess rupture; C: Coronal contrast-enhanced CT image showing an amebic abscess located in segment VI with long-segment thrombosis in the peripheral branch of the right hepatic vein. Note the triangular hypodense area surrounding the abscess, indicating hypoperfused parenchyma; D: Coronal contrast-enhanced CT image showing a large amebic abscess that has ruptured into the thoracic cavity with loculated pleural fluid collections. Note that the abscess demonstrates ragged edges with indistinct enhancement, characteristic of a type I abscess; E: Sagittal contrast-enhanced venous phase CT image of a patient showing thrombus extending from the ALA into the inferior vena cava; F: Axial CT scan showing a communication of left lobe ALA with the gastric lumen forming a hepatogastric fistula.
Figure 3 Computed tomographic classification of amebic liver abscess.
A: Type I amebic liver abscess (ALA) shows incomplete wall and ragged edges with irregular enhancement; B: Type II ALA showing a complete rim enhancement with peripheral hypodense halo; C: Type III ALA showing a chronic non-enhancing wall.
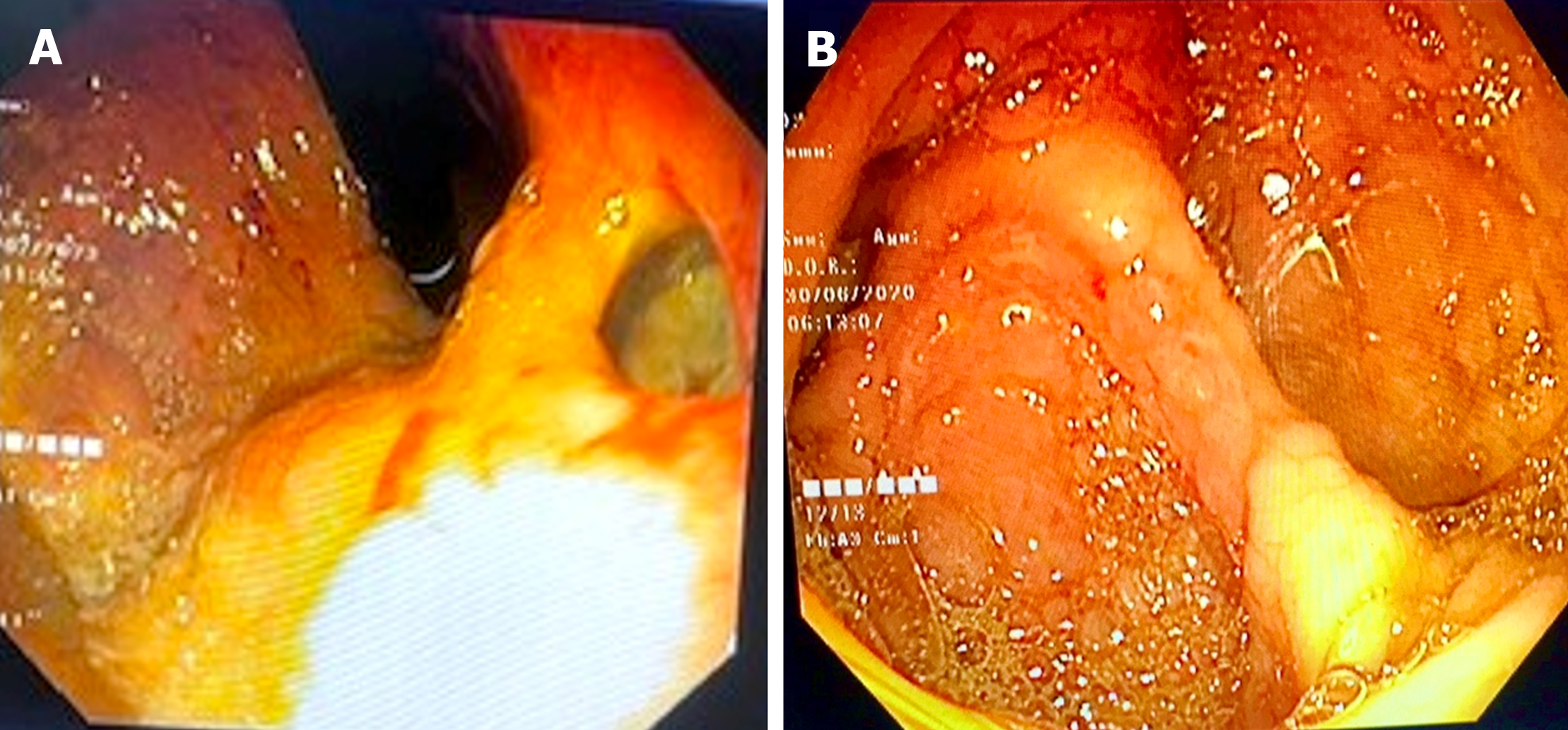
Figure 4 Endoscopic images of complicated amebic liver abscess patients.
A: Shows an upper endoscopic view of hepatogastric fistula resulting from rupture of a left lobe amebic liver abscess (ALA) into the stomach near high lesser curve; B: Shows colonoscopic view of a complicated ALA patient presenting with lower gastrointestinal bleeding from multiple small ulcers from the cecum.
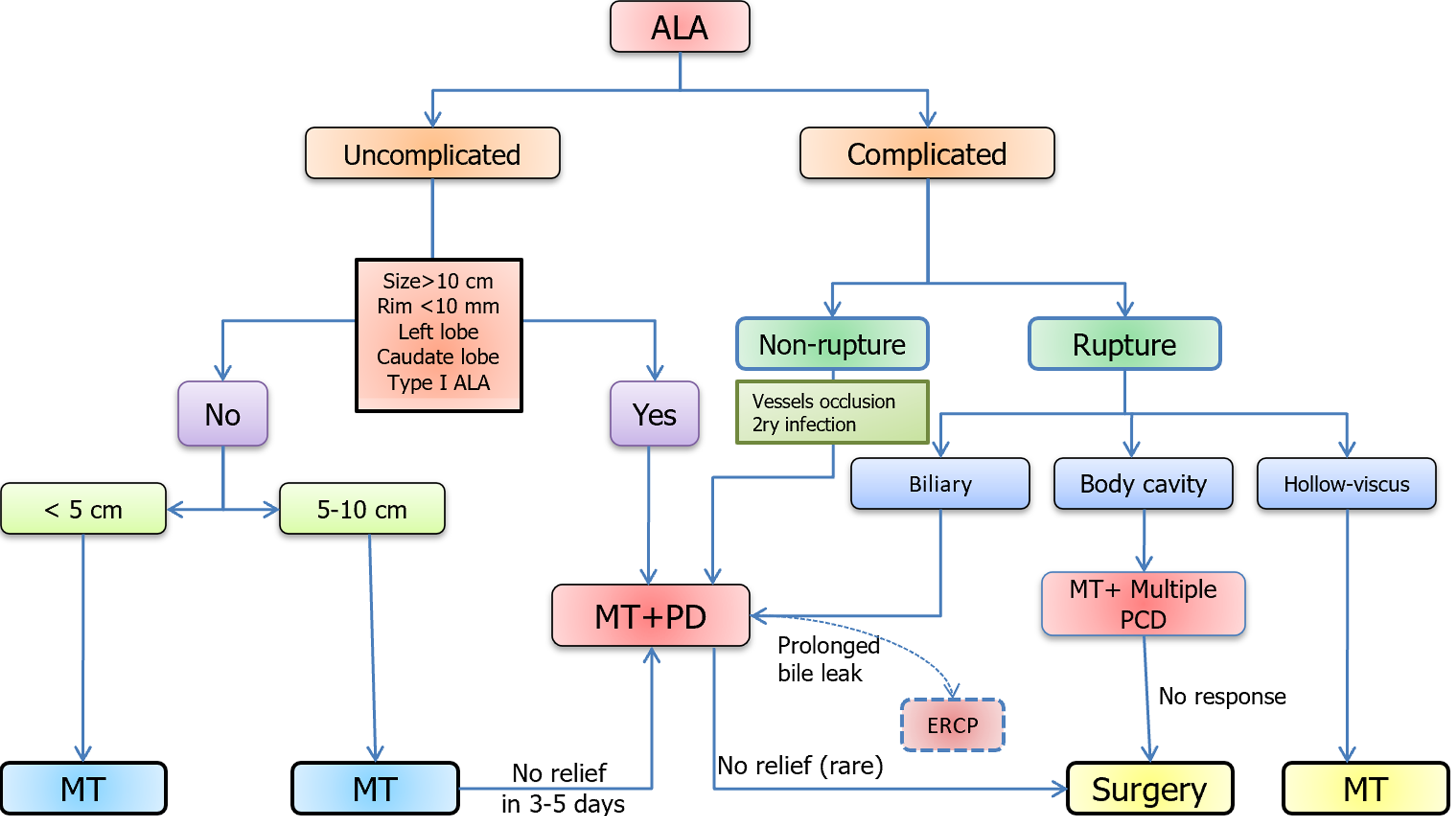
Figure 5 Proposed treatment algorithm for patient with amebic liver abscess.
For uncomplicated amebic liver abscess (ALA): Upfront percutaneous drainage (PD) should be considered only in the presence of high risk signs; PD doesn’t provide added benefit when ALA size is < 5 cm, and ALA with size > 5 should be treated initially with medical therapy (MT) consisting of anti-amebic drug for 3-5 d before considering PD in case of non-response. For PD, a percutaneous catheter drainage (PCD) is preferred over needle aspiration, particularly for larger and incompletely liquified ALA. For complicated ALA patients, some form of drainage procedure is always required. A large majority of such patients can be treated with PCD along with MT. ALA with biliary fistula can be treated with prolonged PCD, and only on rare occasion, an endoscopic retrograde cholangiopancreatography will be required. Finally, ALA with rupture into a hollow viscus can be treated with MT alone. MT: Medical therapy; PD: Percutaneous drainage; ALA: Amebic liver abscess; PCD: Percutaneous catheter drainage; ERCP: Endoscopic retrograde cholangiopancreatography.
- Citation: Kumar R, Patel R, Priyadarshi RN, Narayan R, Maji T, Anand U, Soni JR. Amebic liver abscess: An update. World J Hepatol 2024; 16(3): 316-330
- URL: https://www.wjgnet.com/1948-5182/full/v16/i3/316.htm
- DOI: https://dx.doi.org/10.4254/wjh.v16.i3.316