Copyright
©The Author(s) 2023.
World J Hepatol. Jul 27, 2023; 15(7): 867-882
Published online Jul 27, 2023. doi: 10.4254/wjh.v15.i7.867
Published online Jul 27, 2023. doi: 10.4254/wjh.v15.i7.867
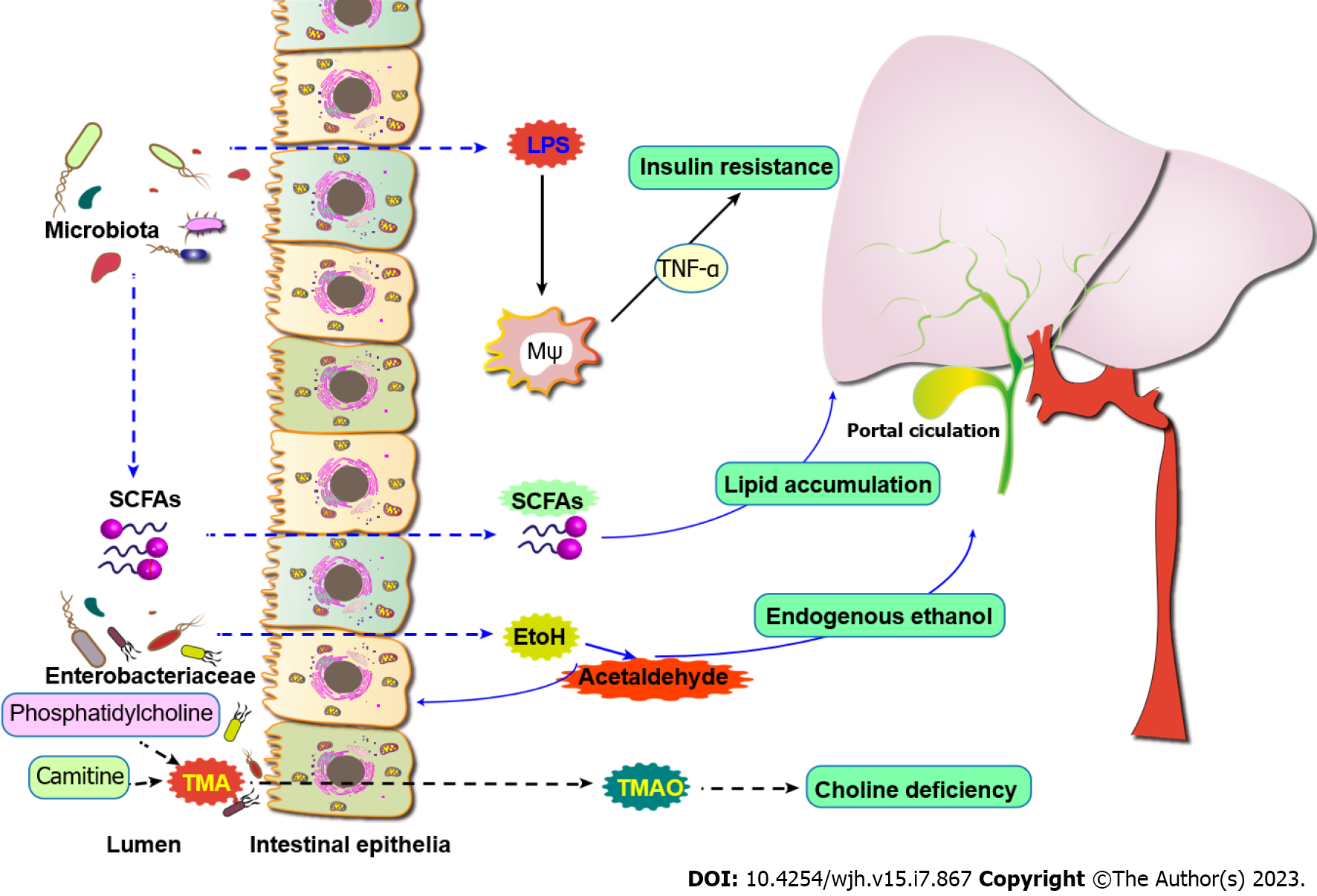
Figure 1 Gut microflora can affect several factors related to the development of metabolic-associated fatty liver disease.
These effects lead to the production of free fatty acids, insulin resistance, and impaired bile secretion in the liver, respectively. In addition, changes in intestinal microflora may lead to increased intestinal permeability, and microbial-derived compounds are transferred from the intestine to the liver through the portal vein, resulting in changes in pro-inflammatory signals, metabolism, and toxicity. Finally, ethanol and its toxic derivative acetaldehyde aggravated hyperoxidative stress and choline deficiency in hepatocytes. EtOH: Ethanol; LPS: Lipopolysaccharides; SCFAs: Short chain fatty acids; TNF-α: Tumor-necrosis factor; TMAO: Trimethylamine N-oxide.
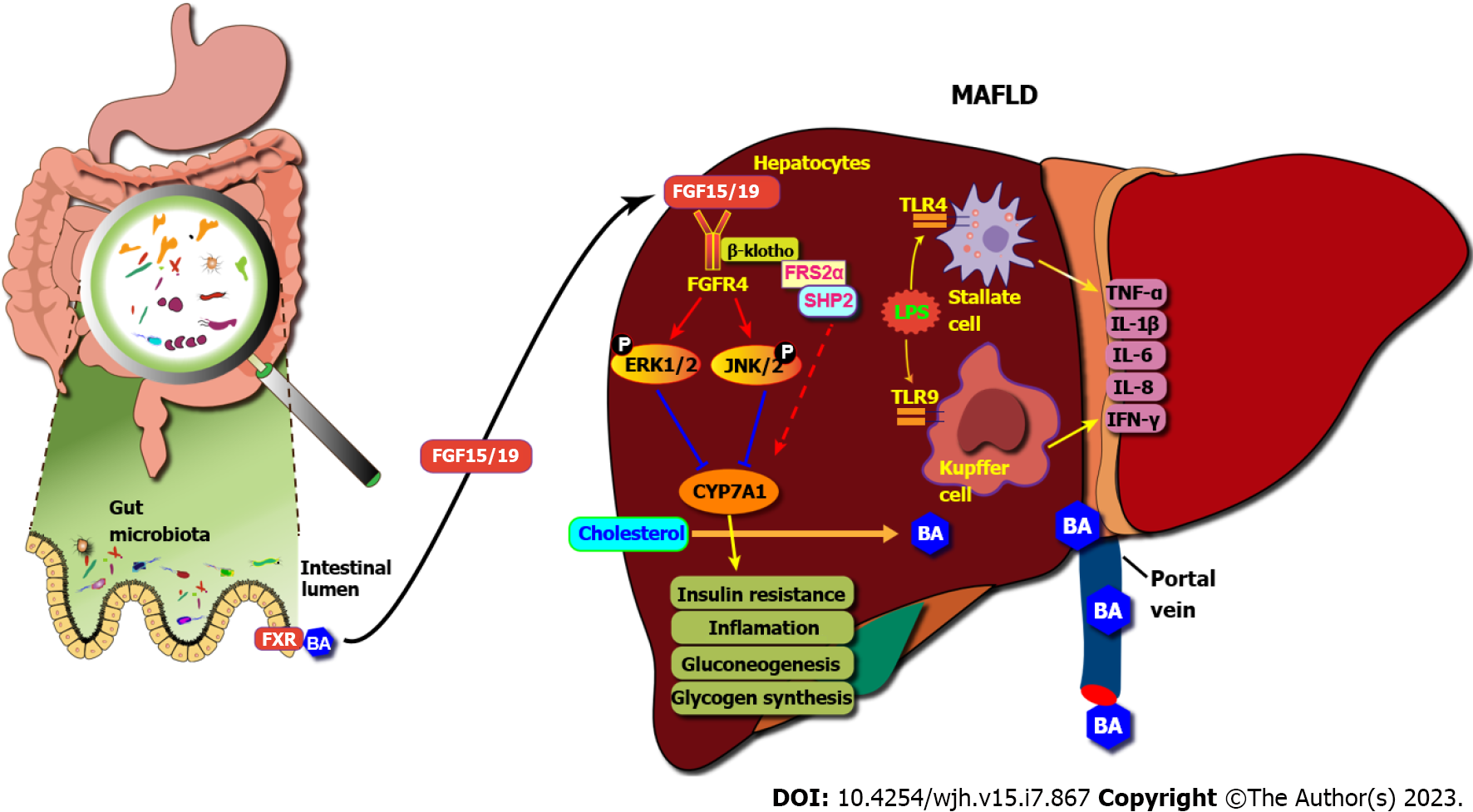
Figure 2 Mechanisms showing the role of gut microbiota in metabolic-associated fatty liver disease.
FXR: Farnesoid X receptor; TGR5: Takeda G protein-coupled; MAFLD: Metabolic-associated fatty liver disease; BA: Bile acid; LPS: Lipopolysaccharides; TNF-α: Tumor-necrosis factor alpha; TLR: Toll like receptor.
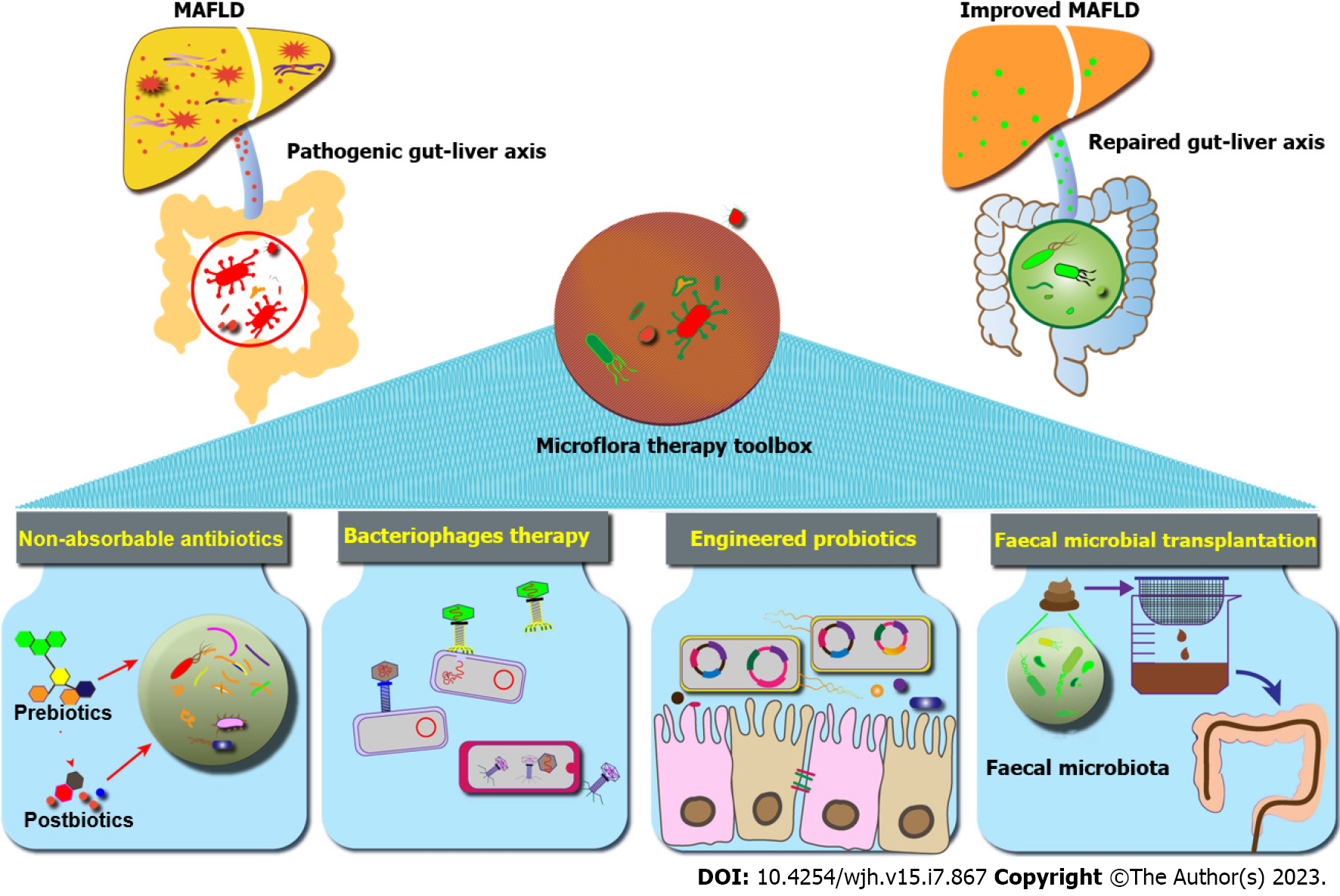
Figure 3 Therapeutic interventions for metabolic-associated fatty liver disease based on microbiota.
Intestinal-centered therapy including antibiotics, bacterial metabolites, probiotics, engineered bacteria, bacteriophages, and fecal microbial transplantation can specifically interfere with intestinal microflora to re-establish the interface between the liver and the microbiome. MAFLD: Metabolic-associated fatty liver disease.
- Citation: Guo GJ, Yao F, Lu WP, Xu HM. Gut microbiome and metabolic-associated fatty liver disease: Current status and potential applications. World J Hepatol 2023; 15(7): 867-882
- URL: https://www.wjgnet.com/1948-5182/full/v15/i7/867.htm
- DOI: https://dx.doi.org/10.4254/wjh.v15.i7.867