Copyright
©The Author(s) 2023.
World J Hepatol. Oct 27, 2023; 15(10): 1140-1152
Published online Oct 27, 2023. doi: 10.4254/wjh.v15.i10.1140
Published online Oct 27, 2023. doi: 10.4254/wjh.v15.i10.1140
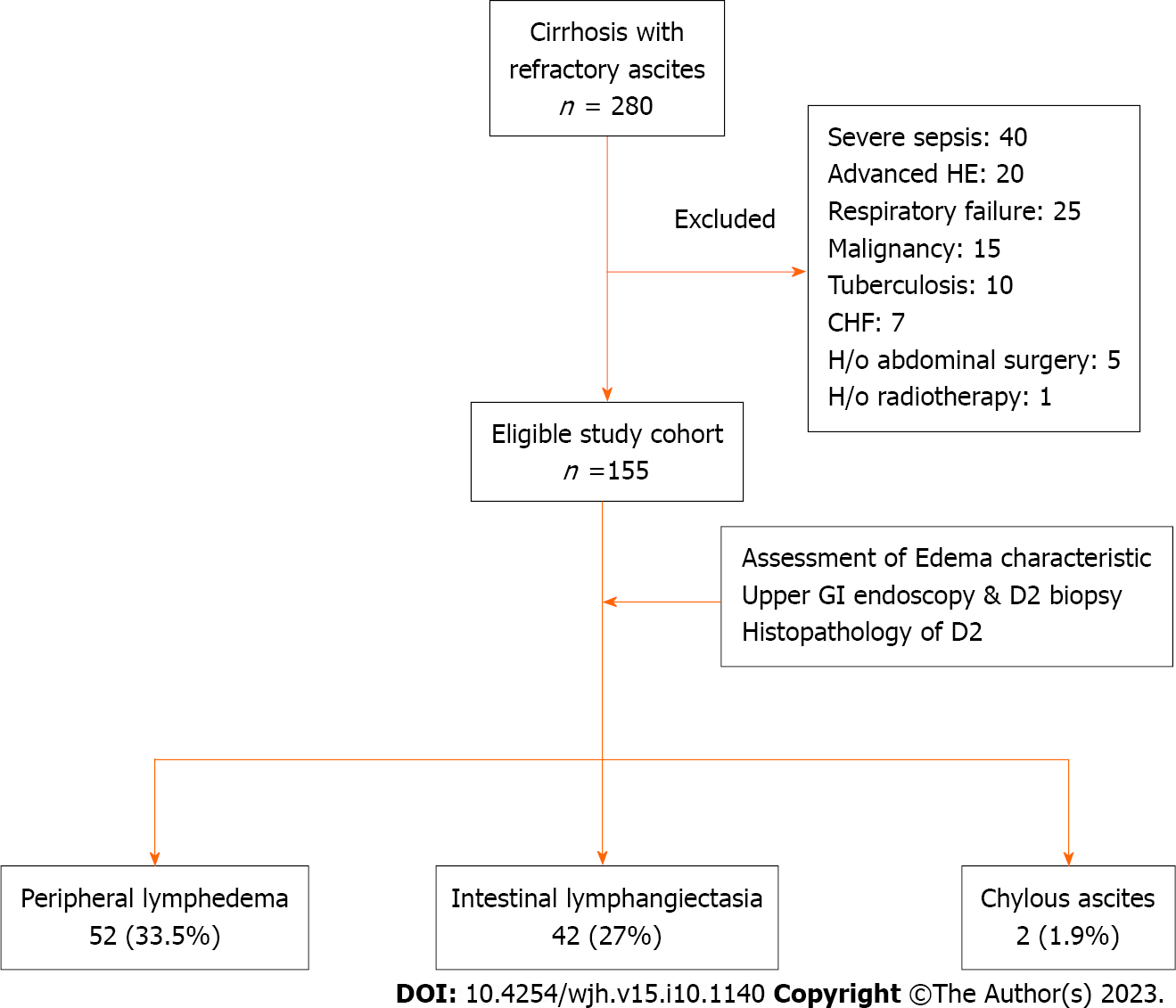
Figure 1 Flow-diagram showing selection, evaluation, and categorization of study population based on lymphatic dysfunction.
A total of 280 cirrhosis patients with refractory ascites were screened, and eventually 155 patients were found to be eligible based on the inclusion and exclusion criteria. Subsequent to evaluation, 69 (44.5%) patients were found to have evidence of lymphatic dysfunction in the form of lymphedema, intestinal lymphangiectasia, and chylous ascites, either alone or in combination. CHF: Congestive heart failure; D2: Second part of duodenum; GI: Gastrointestinal; HE: Hepatic encephalopathy; H/o: History of.
Figure 2 Representative images showing two distinct patterns of peripheral edema among cirrhosis patients with refractory ascites.
A and B: Physical appearance of peripheral edema revealed two distinct patterns. In the majority of patients, edema was pitting type and skin texture was smooth (A), which is a finding consistent with edema due to the hydrostatic-oncotic pressure imbalance. In about one-third of patients, edema was severe, mostly non-pitting type with skin texture showing exaggerated dorsal skin creases, hyperkeratosis, and peau d’orange appearance (B), suggesting lymphedema. Some patients with lymphedema also had evidence of cellulitis.
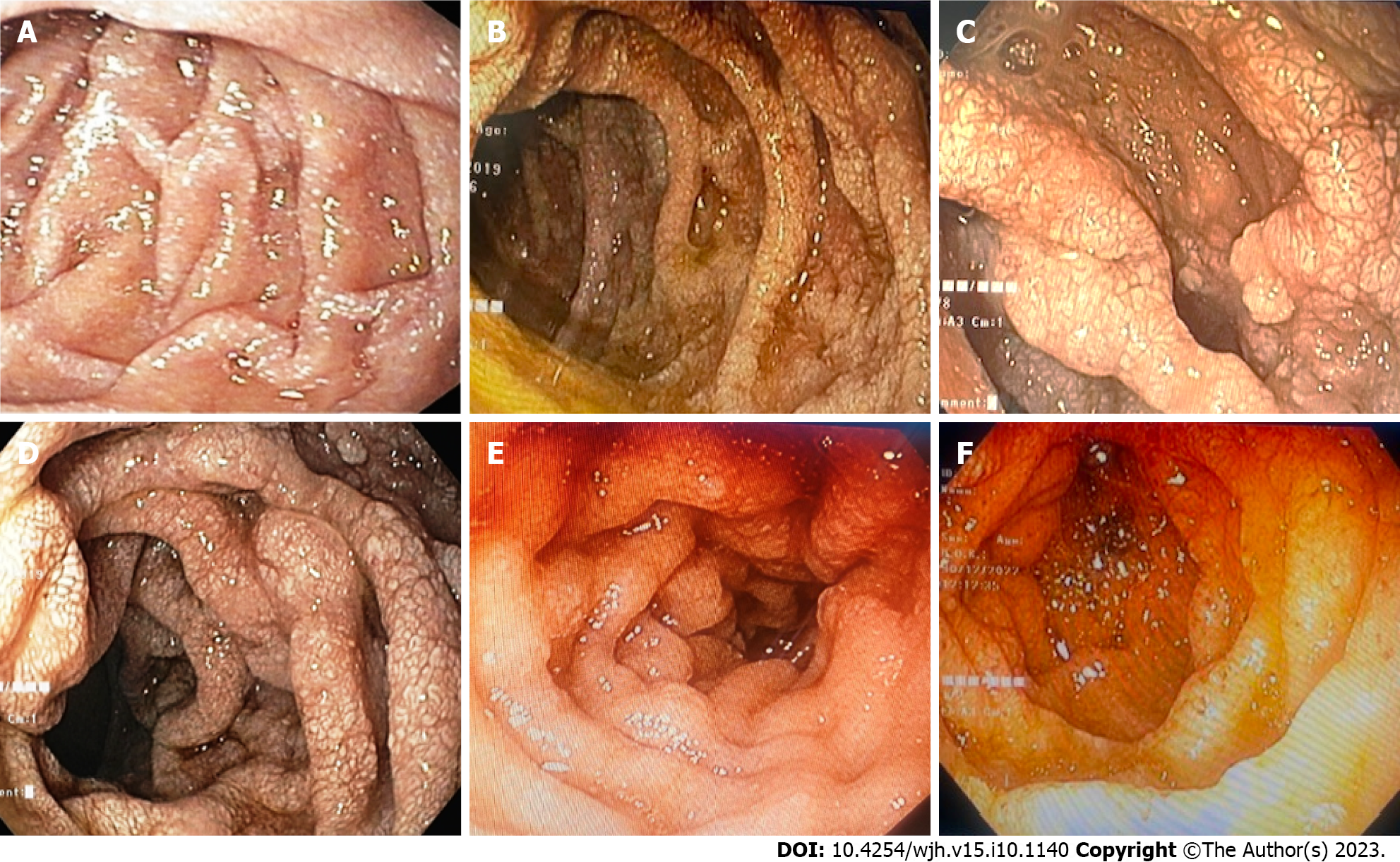
Figure 3 Endoscopic evaluation of study population.
A-F: Representative endoscopic images of duodenum of study population showing portal hypertensive duodenopathy with evidence of intestinal lymphangiectasia visualized as scattered white spots suggestive of dilated lacteals.
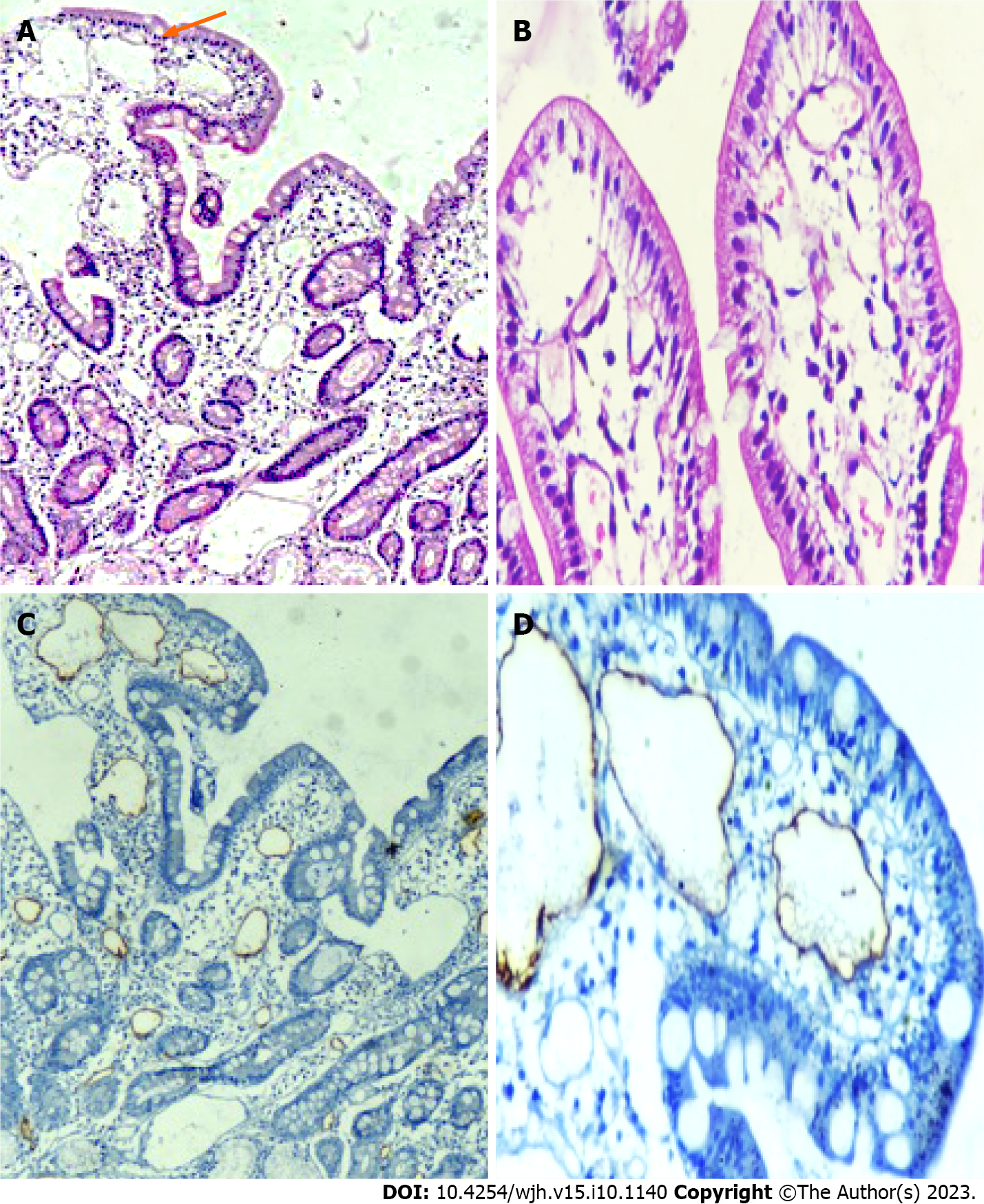
Figure 4 Histological examination of second part of duodenum biopsy specimens.
A-D: Representative histopathological images (hematoxylin and eosin) of duodenum showing markedly dilated vessels in the lamina propria (A and B), which on immunohistochemistry showing strong D2-40 positivity (C and D), confirming the presence of intestinal lymphangiectasia.
- Citation: Arya R, Kumar R, Kumar T, Kumar S, Anand U, Priyadarshi RN, Maji T. Prevalence and risk factors of lymphatic dysfunction in cirrhosis patients with refractory ascites: An often unconsidered mechanism. World J Hepatol 2023; 15(10): 1140-1152
- URL: https://www.wjgnet.com/1948-5182/full/v15/i10/1140.htm
- DOI: https://dx.doi.org/10.4254/wjh.v15.i10.1140