Copyright
©The Author(s) 2022.
World J Hepatol. Jul 27, 2022; 14(7): 1291-1306
Published online Jul 27, 2022. doi: 10.4254/wjh.v14.i7.1291
Published online Jul 27, 2022. doi: 10.4254/wjh.v14.i7.1291
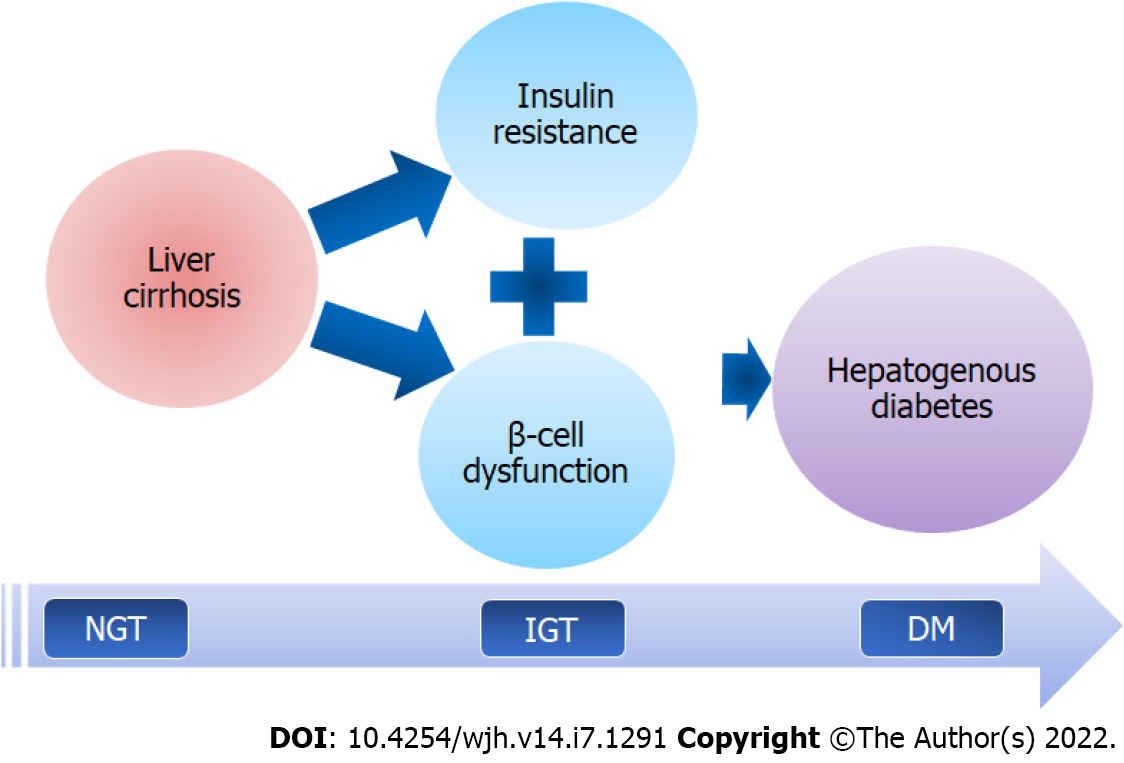
Figure 1 Key events leading to development of hepatogenous diabetes in patients with liver cirrhosis.
Insulin resistance, followed by β-cell dysfunction, occurs as a result of liver cirrhosis, culminating in a progressive worsening of glucose tolerance and the onset of hepatogenous diabetes. Both of these occurrences are linked to the pathophysiological changes in the body caused by liver cirrhosis. NGT: Normal glucose tolerance; IGT: Impaired glucose tolerance; DM: Diabetes mellitus.
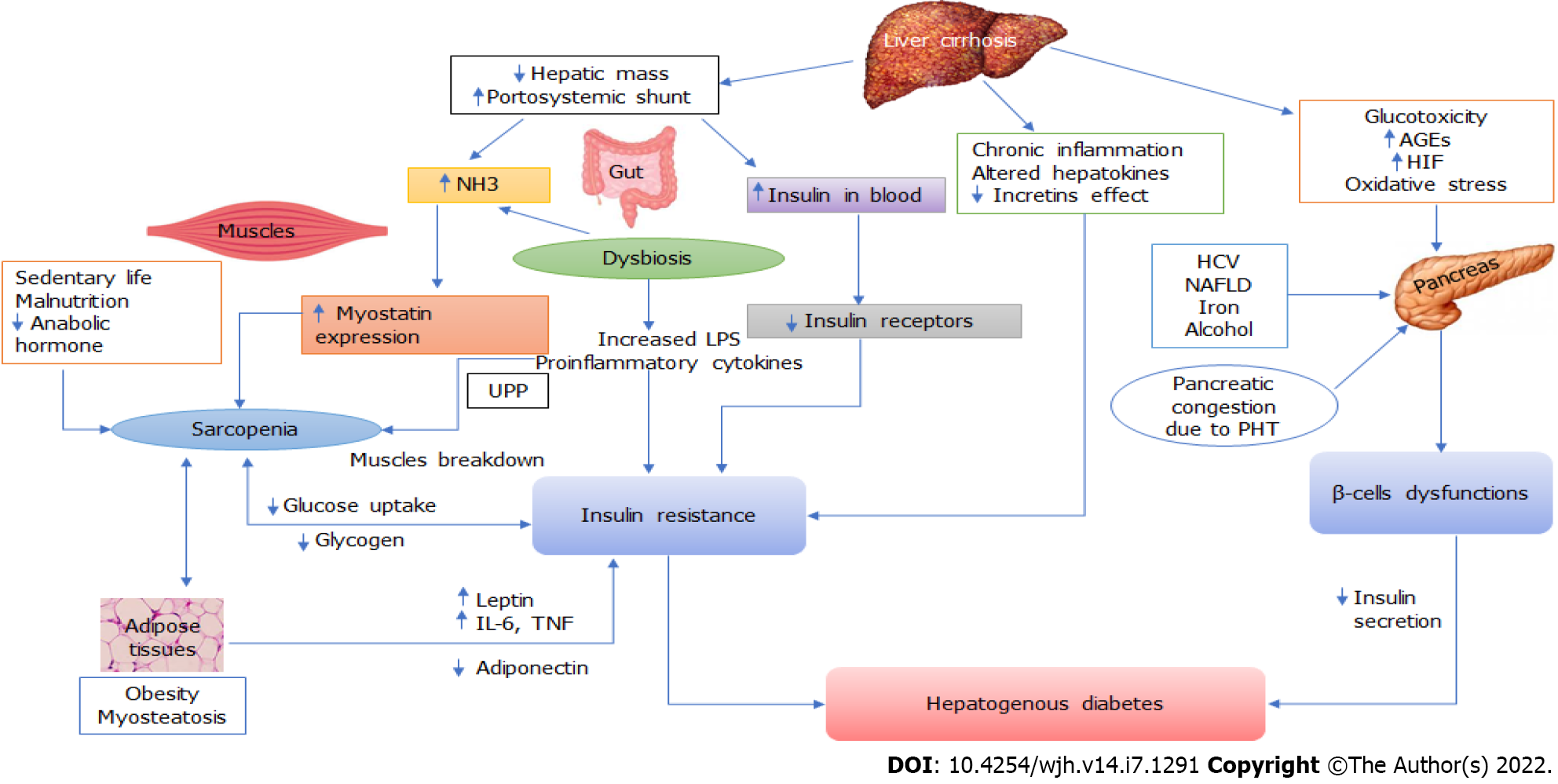
Figure 2 Complex pathophysiological mechanisms likely to play important roles in the development of hepatogenous diabetes.
Neurohormonal alterations, endotoxemia, and chronic inflammation induced by cirrhosis and portal hypertension all contribute to the development of insulin resistance and β-cell dysfunction. These changes may be further modulated by other concomitant abnormalities, such as gut dysbiosis, hyperammonemia, sarcopenia, adiposity, and myosteatosis. NH3: Ammonia; AGE: Advanced glycation end products; HIF: Hypoxia inducible factor; HCV: Hepatitis C virus; NAFLD: Non-alcoholic fatty liver disease; LPS: Lipopolysaccharides; IL-6: Interleukin-6; TNF: Tumour necrosis factor; UPP: Ubiquitin proteasome pathways.
- Citation: Kumar R, García-Compeán D, Maji T. Hepatogenous diabetes: Knowledge, evidence, and skepticism. World J Hepatol 2022; 14(7): 1291-1306
- URL: https://www.wjgnet.com/1948-5182/full/v14/i7/1291.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i7.1291