Copyright
©The Author(s) 2020.
World J Hepatol. Sep 27, 2020; 12(9): 574-595
Published online Sep 27, 2020. doi: 10.4254/wjh.v12.i9.574
Published online Sep 27, 2020. doi: 10.4254/wjh.v12.i9.574
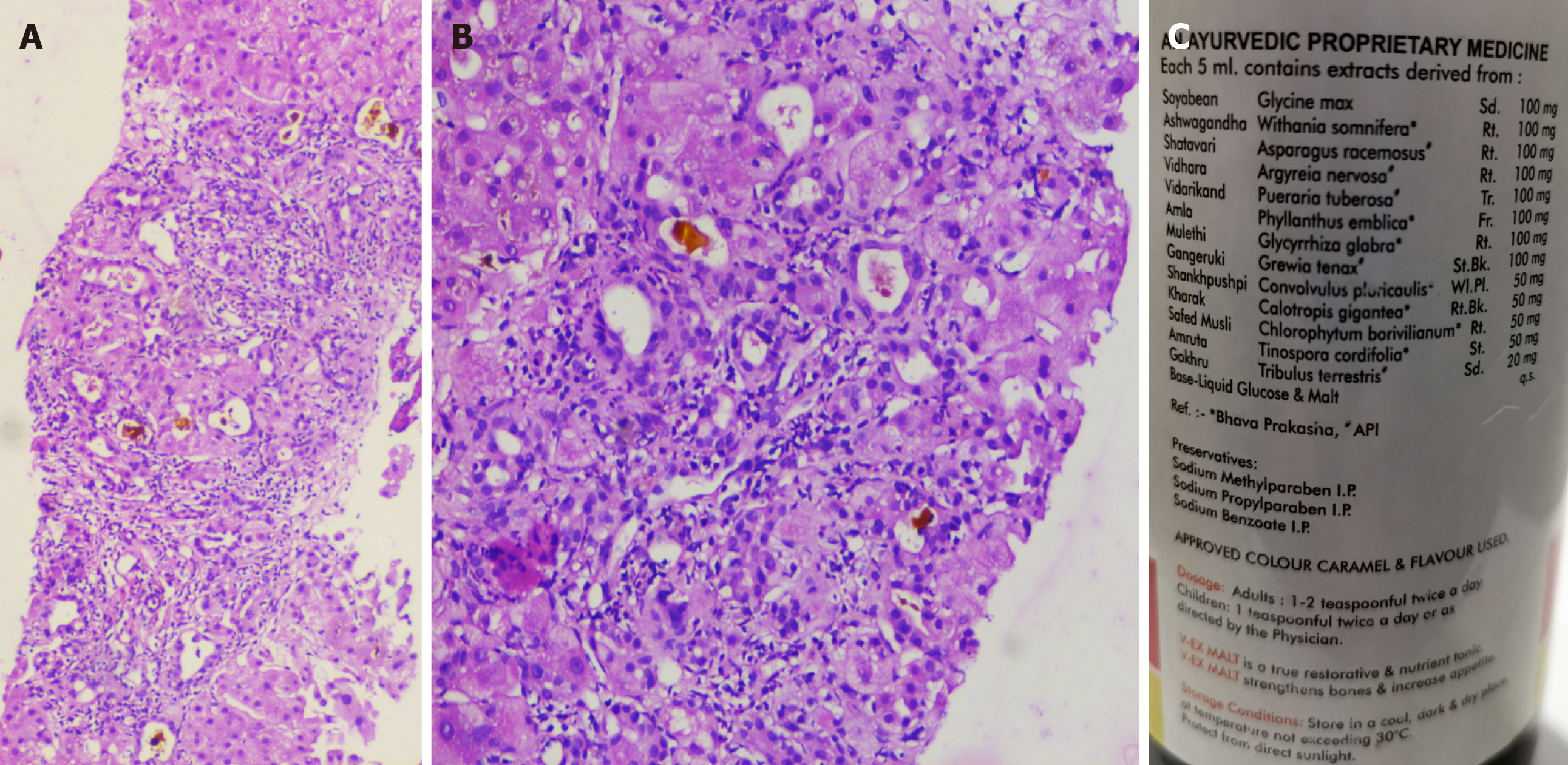
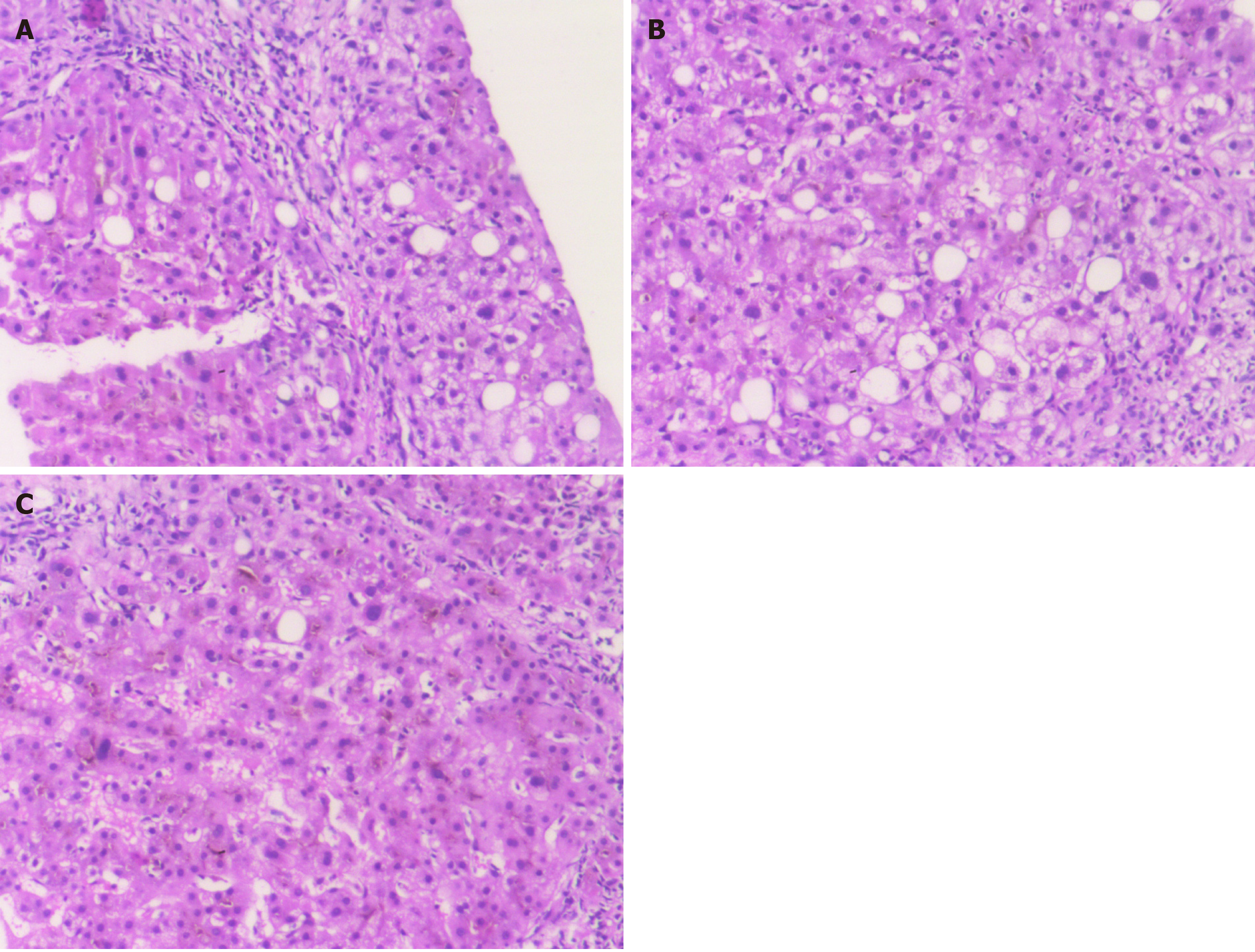
Figure 1 Liver histopathology of acute liver injury in a patient ingesting Ashwagandha.
A and B: Percutaneous liver biopsy revealed severe canalicular cholestasis along with moderate portal inflammation [A, hematoxylin and eosin stain (H&E), 40 × and B, H&E stain, 400 ×)]; C: The polyherbal formulation containing Ashwagandha, retrieved from the patient is shown in C. The patient had an uneventful course with resolution of symptoms and normalization of liver tests at 2 mo.
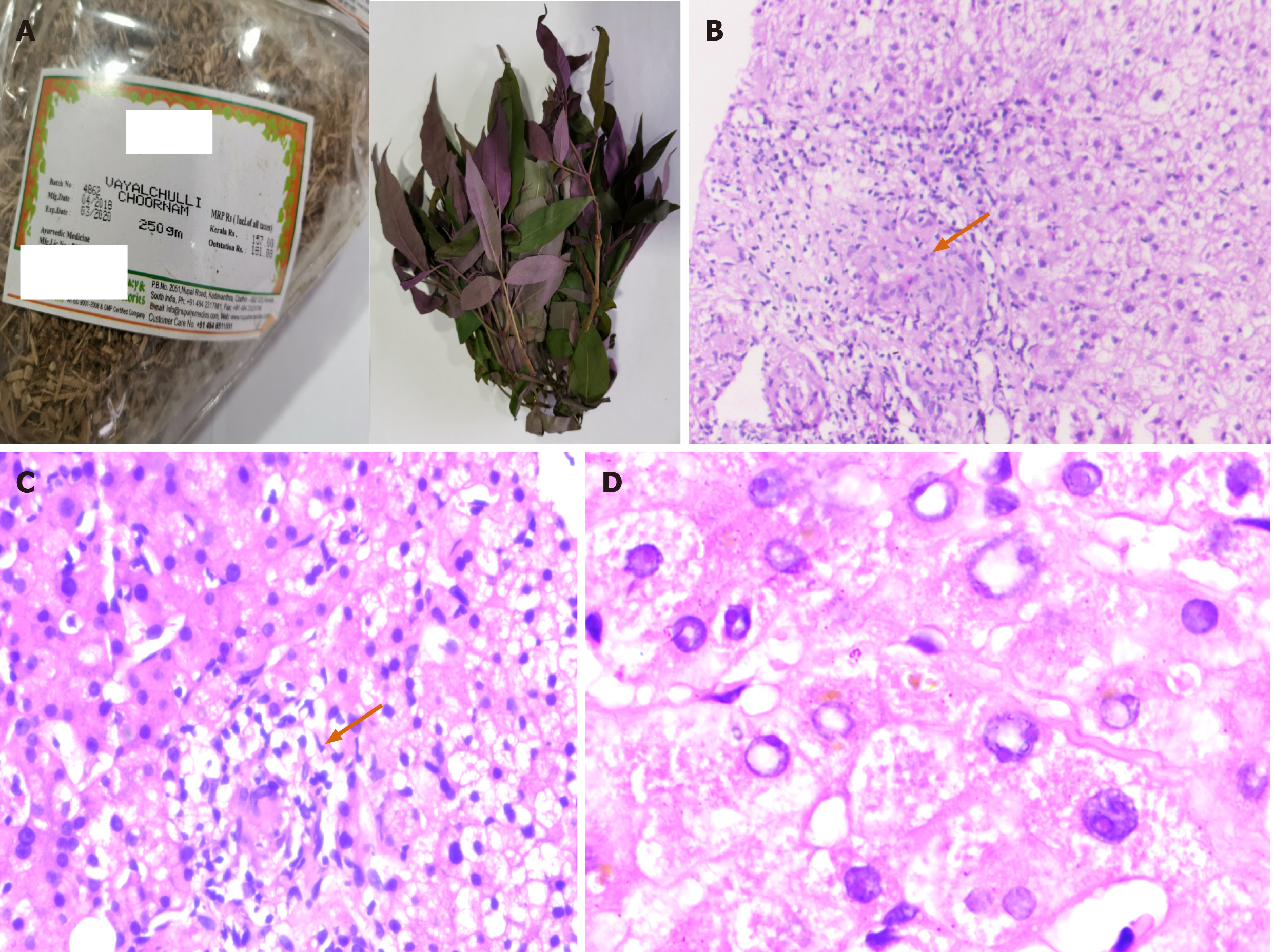
Figure 2 Granulomatous hepatitis in a patient consuming multiple Ayurvedic herbs.
The retrieved herbs implicated in acute liver injury with granulomatous hepatitis are shown in A (Hygrophila auriculate, also called the Marsh Barbel and an unknown coloured herb). Transjugular liver biopsy was performed in view of ascites in this patient. The liver histology revealed large vague as well as well-formed lobular and portal based granulomas and associated eosinophilic and lymphocytic inflammation within the sinusoids [B and C; hematoxylin and eosin (H&E), 100 × and 400 × respectively]; severe feathery degeneration of hepatocytes associated with hepatocellular cholestasis was also notable (D, H&E, 400 ×). This patient died after 6 mo follow-up due to portal hypertensive events complicated by septic shock.
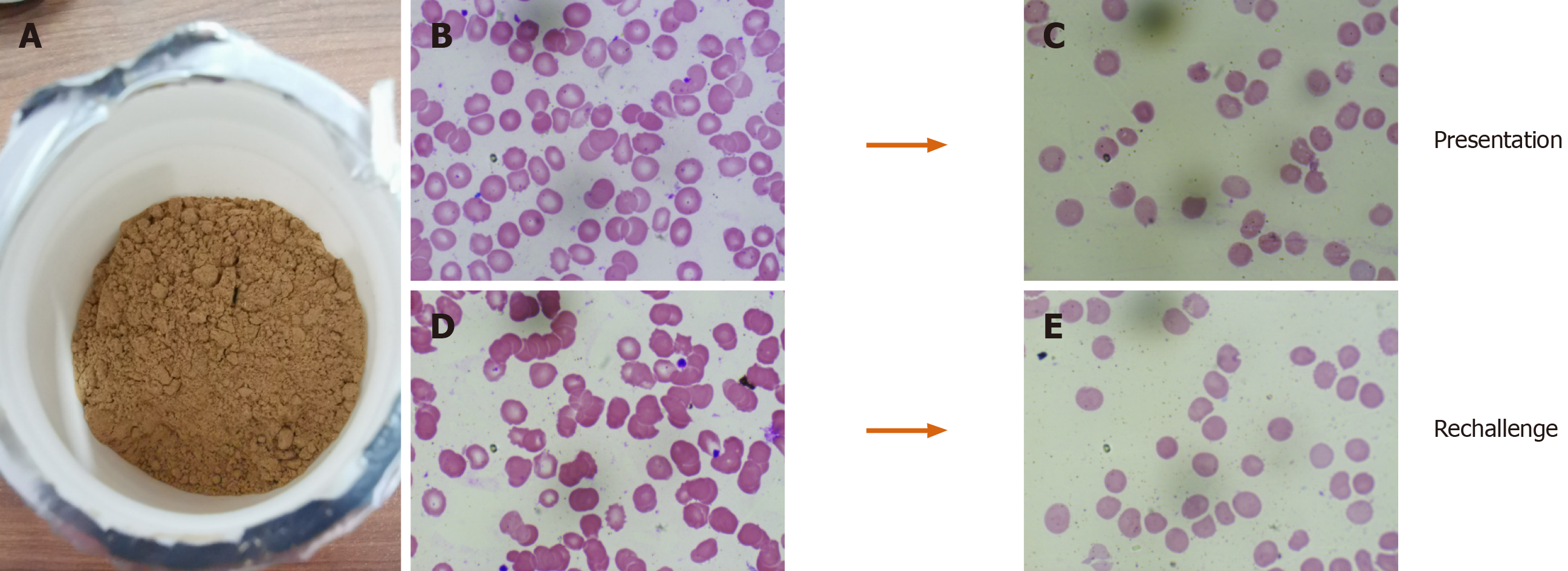
Figure 3 Turmeric-induced spur cell anemia in a patient with compensated cirrhosis.
The retrieved turmeric powder supplement is shown in A; B and C (Wright Giemsa stain, 40 ×) shows the presence of spur cells and resolution of spur cells on turmeric withdrawal. On rechallenge (D and E; Wright-Giemsa stain, 40 ×) with turmeric supplement, spur cells reappeared without the need for blood transfusion, only to resolve after withdrawing the offending agent again.
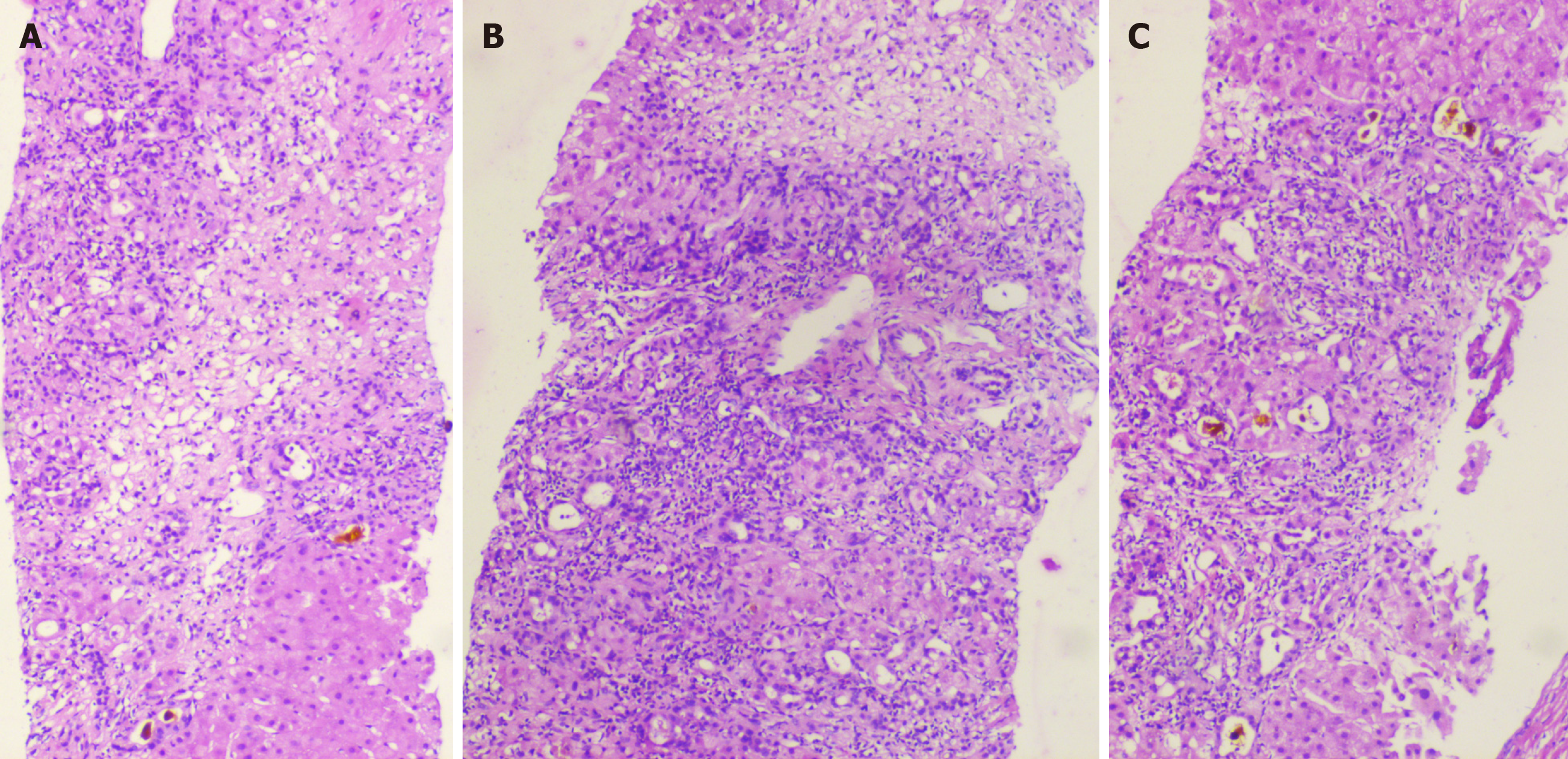
Figure 4 Guggul-related liver toxicity.
The liver histopathology showed zone 3 necrosis extending to the portal region [A, hematoxylin and eosin (H&E) stain, 40 ×] with mixed neutrophilic and eosinophilic inflammation of the portal region associated with severe ductular reaction and early fibrosis (B, H&E stain, 100 ×). Associated moderate to severe canalicular cholestasis is also noted (C, H&E stain, 40 ×).
Figure 5 Aloe vera-induced liver injury in a middle-aged diabetic woman.
The percutaneous liver histopathology showed porto-portal bridging necrosis [A, hematoxylin and eosin (H&E) stain, 200 ×] associated with moderate to severe ballooning of hepatocytes, hepatocyte fall out and neutrophilic satellitosis (B, H&E stain, 400 ×). Severe intrahepatic and canalicular cholestasis is also noted (C, H&E stain, 400 ×).
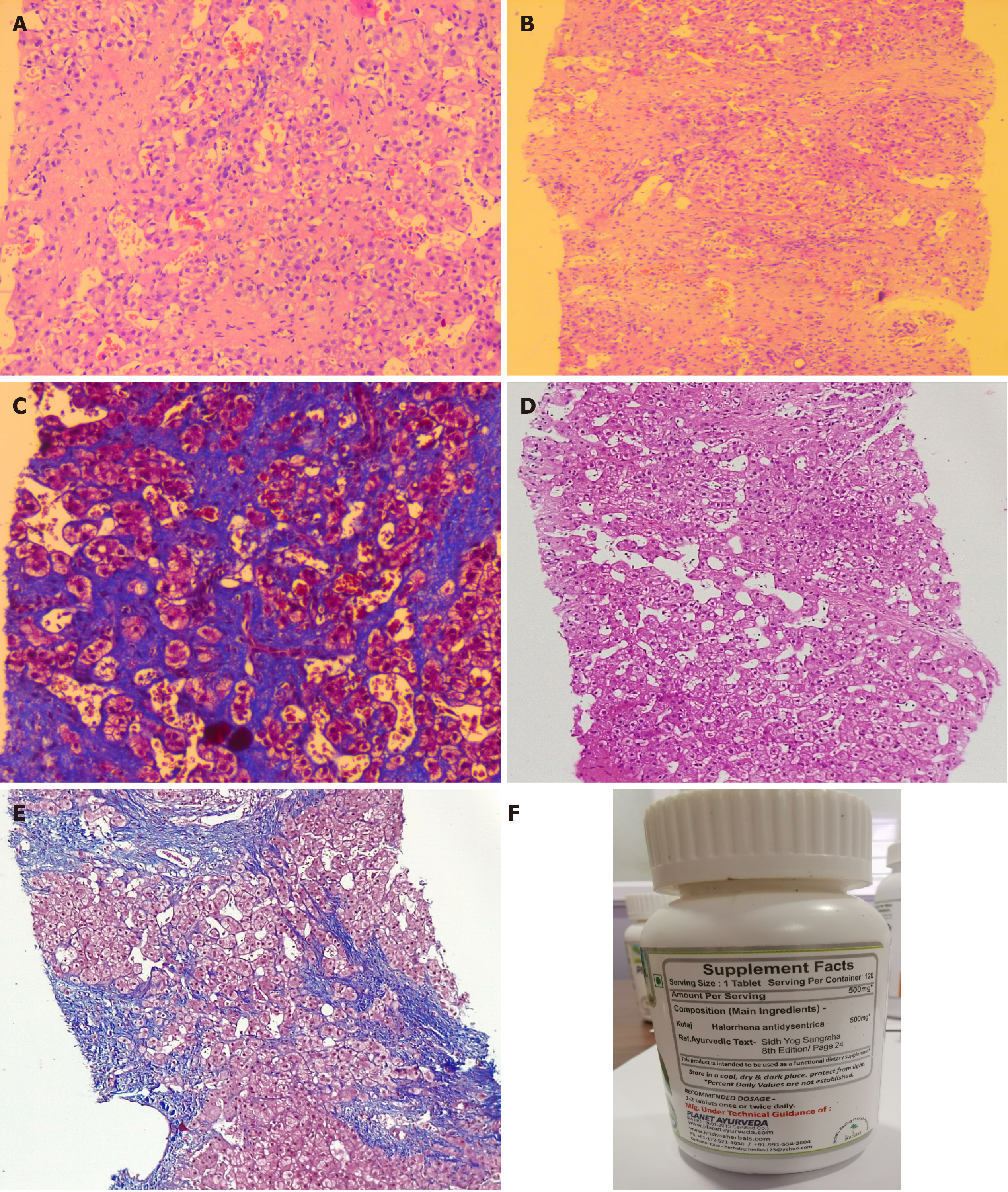
Figure 6 Hepatic sinusoidal obstruction syndrome in a young male who consumed Holarrhena antidysenterica, known to contain pyrrolizidine alkaloids.
Transjugular liver biopsy was performed in view of ascites. The liver histology showed fairly preserved portal areas with extensive sinusoidal dilatation in all zones associated with early sinusoidal and peri-sinusoidal fibrosis [A and B, hematoxylin and eosin (H&E) stain, 400 ×]; the sinusoidal fibrosis is quite evident on Masson-trichrome stain (C, 400 ×); after one year follow-up, in view of recurrence of ascites and acute variceal bleeding, a repeat liver biopsy was performed which revealed prominent sinusoidal dilatation with sinusoidal and portal fibrosis (D, H&E stain, 200 ×) and cirrhosis changes with bridging fibrosis and partial nodule formation (E, Masson-trichrome stain, 200 ×). The retrieved over-the-counter herbal supplement is shown (F).
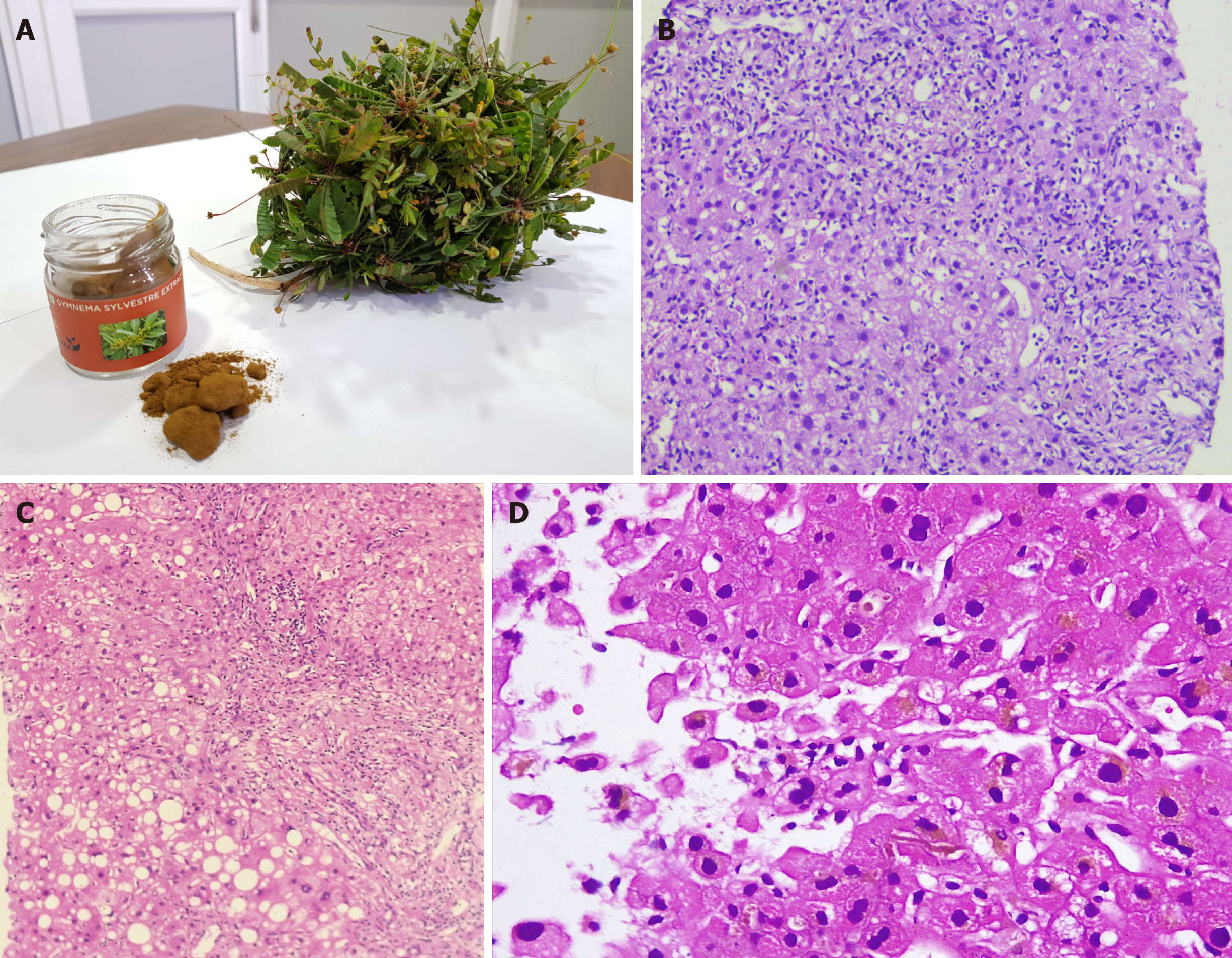
Figure 7 Acute cholestatic hepatitis due to Gymnema sylvestre (gurmar or sugar destroyer) herb.
The retrieved herbal supplement and an unknown herb is shown in A. Liver biopsy revealed moderate to severe neutrophil predominant interface hepatitis [B, hematoxylin and eosin (H&E) stain, 200 ×]; micro and macrovesicular steatosis, lobular inflammation and severe ductular reaction (C, H&E stain, 200 ×) and intrahepatic cholestasis with eosinophilic degeneration of hepatocytes (D, H&E stain, 400 ×).
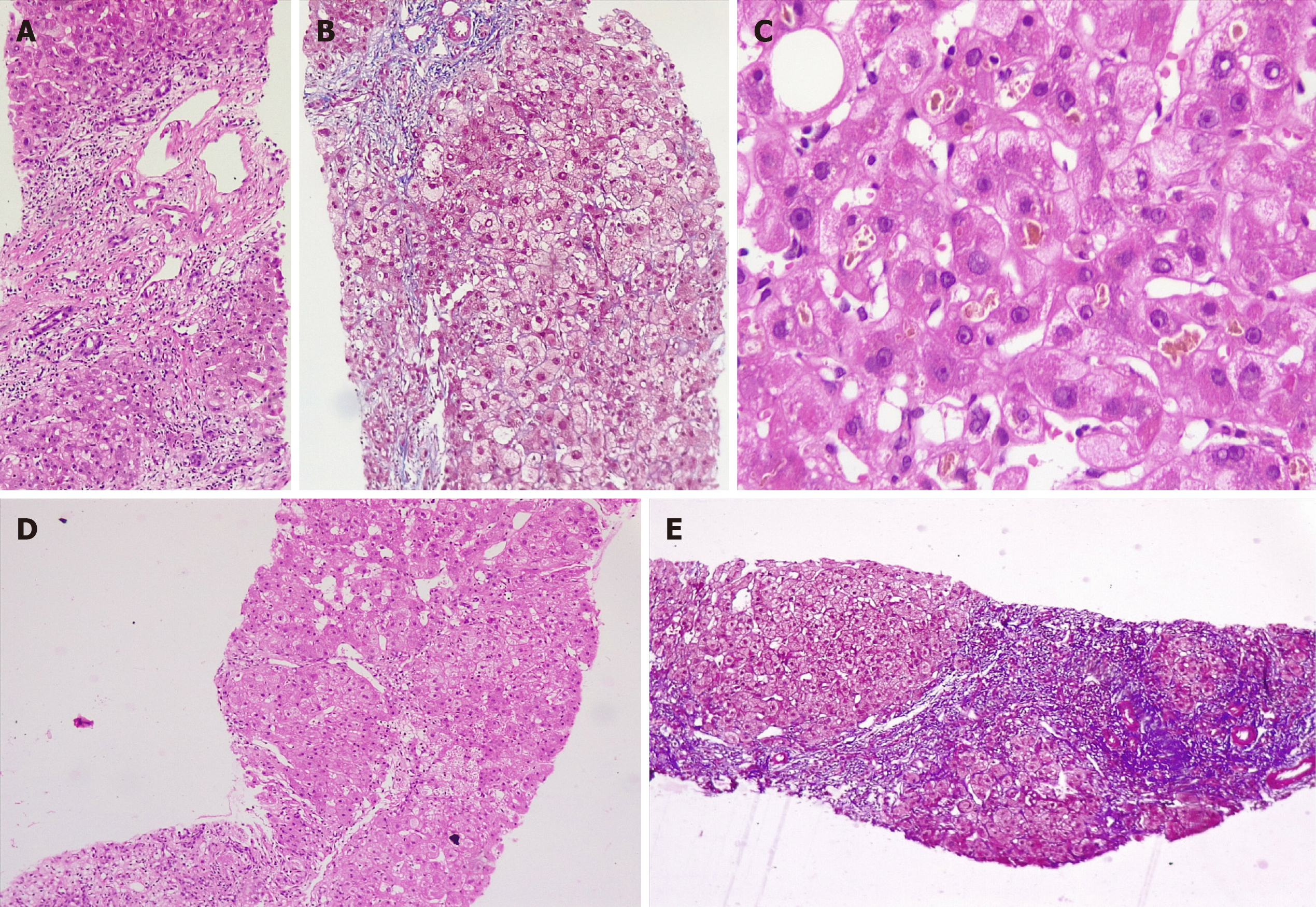
Figure 8 Development of acute severe cholestatic hepatitis leading to chronic herb-induced liver injury resulting in cirrhosis in a young female, after ingestion of Valerian (Tagara®).
Percutaneous liver biopsy performed in August 2019 (A-C) revealed portal and periportal necrosis with mixed lobular inflammation [A, hematoxylin and eosin (H&E) stain, 100 ×], pale blue staining in the regions of necrosis and hepatocyte loss is notable on Masson-trichrome staining (B, 200 ×); hepatocellular and canalicular cholestasis is notable (C, H&E, 400 ×); on follow-up, liver biopsy showed progression of fibrosis with vague hepatocyte nodule formation (D, H&E, 200 ×) with central to central and central to portal bridging fibrosis suggestive of cirrhosis and nodule formation on Masson-trichrome stain (E, 100 ×).
- Citation: Philips CA, Ahamed R, Rajesh S, George T, Mohanan M, Augustine P. Comprehensive review of hepatotoxicity associated with traditional Indian Ayurvedic herbs. World J Hepatol 2020; 12(9): 574-595
- URL: https://www.wjgnet.com/1948-5182/full/v12/i9/574.htm
- DOI: https://dx.doi.org/10.4254/wjh.v12.i9.574