Copyright
©The Author(s) 2020.
World J Hepatol. Oct 27, 2020; 12(10): 870-879
Published online Oct 27, 2020. doi: 10.4254/wjh.v12.i10.870
Published online Oct 27, 2020. doi: 10.4254/wjh.v12.i10.870
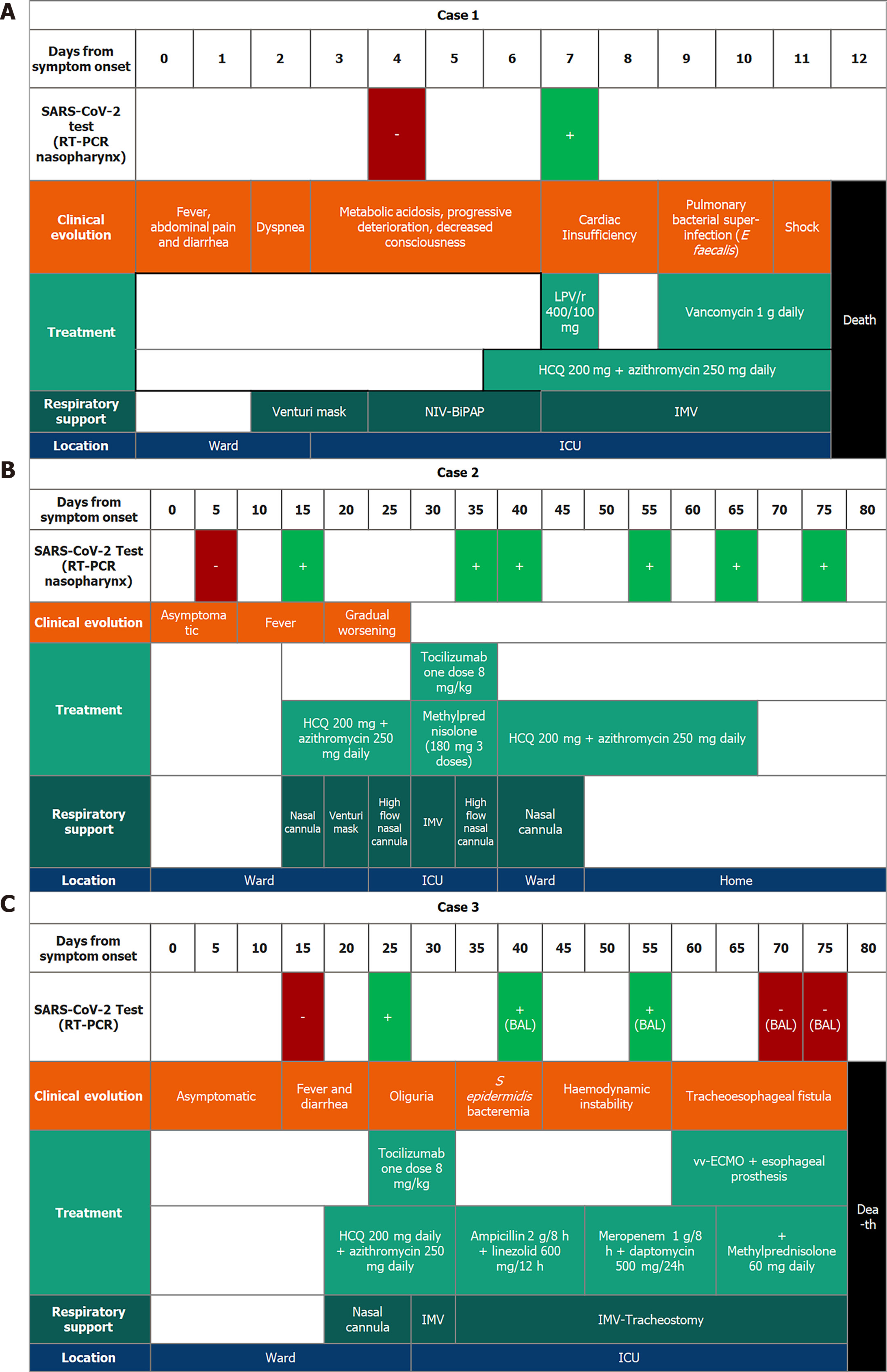
Figure 1 Clinical evolution of each case in a chronological perspective.
A: (Case 1) Although the first reverse transcription polymerase chain reaction of severe acute respiratory syndrome coronavirus 2 was negative for the first few days, dyspnea became worse requiring intensive care unit admission. A single dose of lopinavir/ritonavir was administered on day 7; B: (Case 2) A dose of tocilizumab was administered on day 33. The patient improved progressively until he was discharged home; and C: (Case 3) A dose of tocilizumab was administered on day 28. The patient suffered a progressive worsening. A tracheoesophageal fistula was detected and an oesophageal prosthesis was placed. In addition, a venovenous extracorporeal membrane oxygenation was implemented to improve the patient's oxygenation. BAL: Bronchoalveolar lavage; ICU: Intensive care unit; IMV: Invasive mechanical ventilation; LPV/r: Lopinavir/ritonavir; NIV: Non-invasive ventilation; RT-PCR: Reverse transcription polymerase chain reaction; vv-ECMO: Venovenous extracorporeal membrane oxygenation.
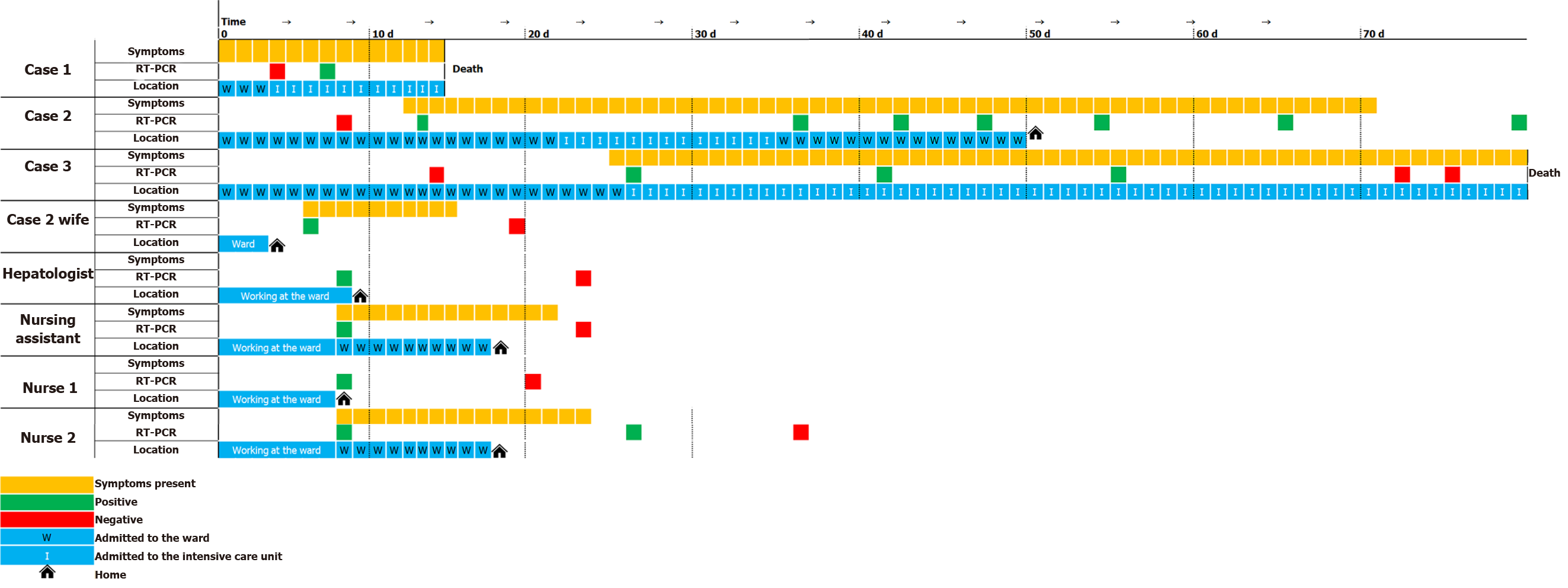
Figure 2 Epidemiological evolution of severe acute respiratory syndrome coronavirus 2 outbreak in our transplant division, according to the presence or absence of symptoms, the positivity of the reverse transcription polymerase chain reaction, and the patients’ locations each day from symptoms onset.
In orange, when suggestive symptomatology of novel coronavirus 2019 was present. In green, when the reverse transcription polymerase chain reaction of severe acute respiratory syndrome coronavirus 2 was positive. In red, when reverse transcription polymerase chain reaction was performed but was negative. W: Admitted to the ward; I: Admitted to the intensive care unit.
- Citation: Alconchel F, Cascales-Campos PA, Pons JA, Martínez M, Valiente-Campos J, Gajownik U, Ortiz ML, Martínez-Alarcón L, Parrilla P, Robles R, Sánchez-Bueno F, Moreno S, Ramírez P. Severe COVID-19 after liver transplantation, surviving the pitfalls of learning on-the-go: Three case reports. World J Hepatol 2020; 12(10): 870-879
- URL: https://www.wjgnet.com/1948-5182/full/v12/i10/870.htm
- DOI: https://dx.doi.org/10.4254/wjh.v12.i10.870