Copyright
©The Author(s) 2019.
World J Hepatol. Nov 27, 2019; 11(11): 743-751
Published online Nov 27, 2019. doi: 10.4254/wjh.v11.i11.743
Published online Nov 27, 2019. doi: 10.4254/wjh.v11.i11.743
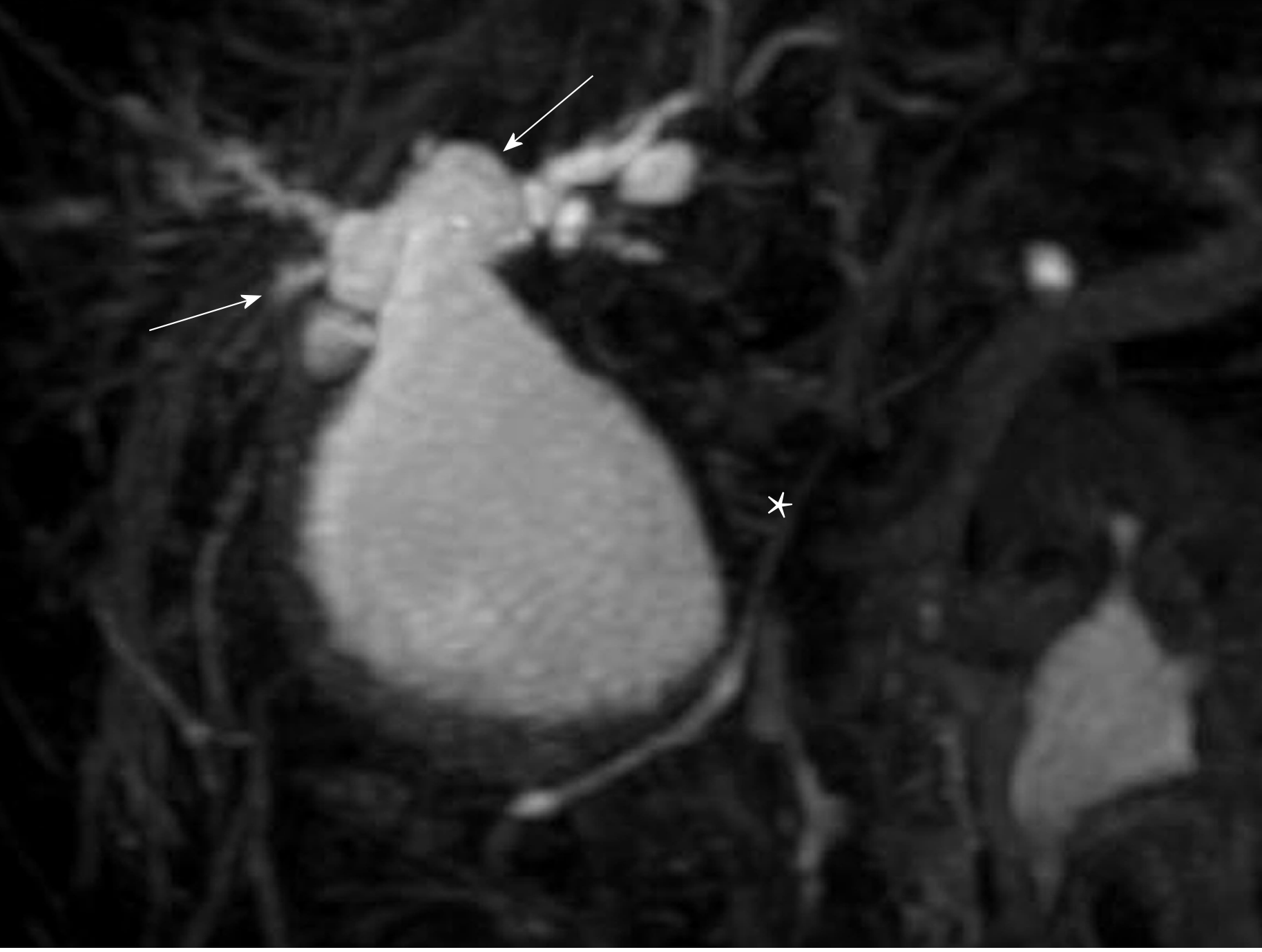
Figure 1 3D-reconstruction of magnetic resonance cholangiopancreatography shows an abnormally dilated common bile duct (white star).
Both right and left hepatic ducts also show intrahepatic dilatations (white arrows).
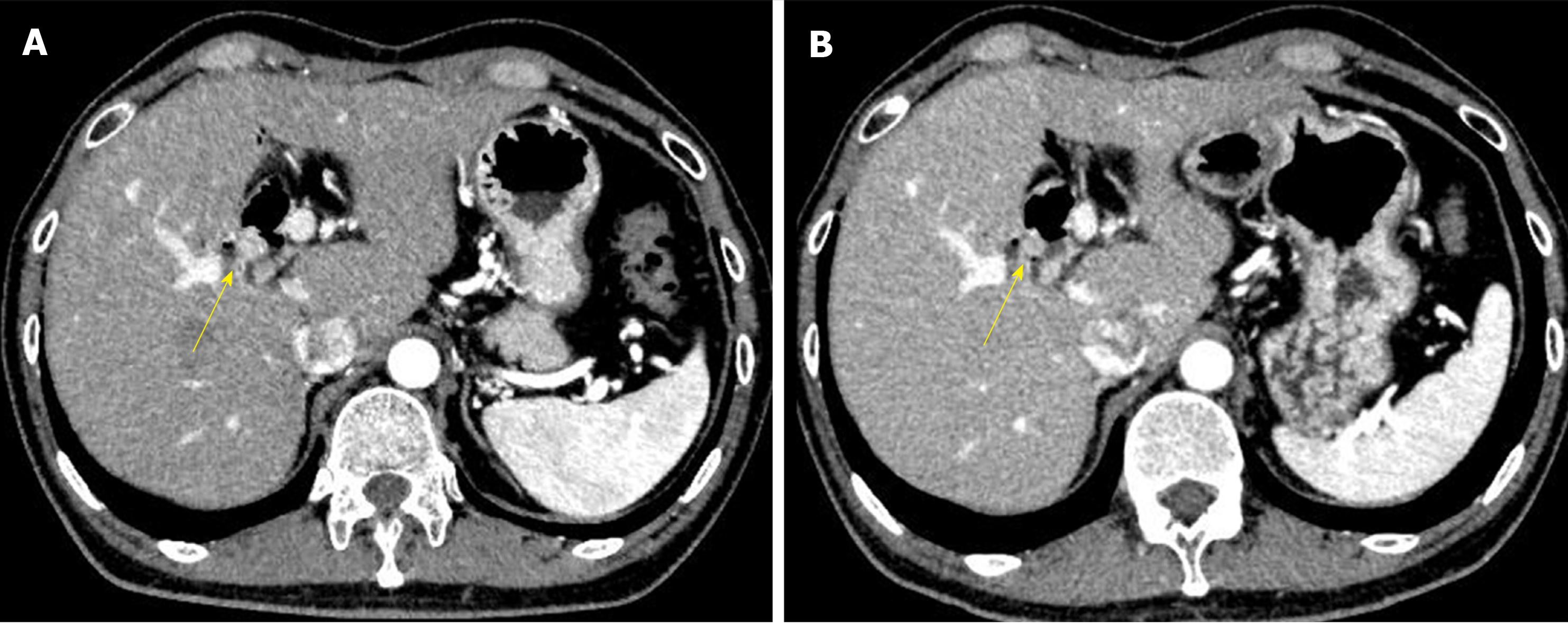
Figure 2 Abdominal CT images with contrast.
A: Five and a half years after his first operation; B: Six years after his first operation. The images show a gradually growing nodule with contrast over a half a year (yellow arrow).
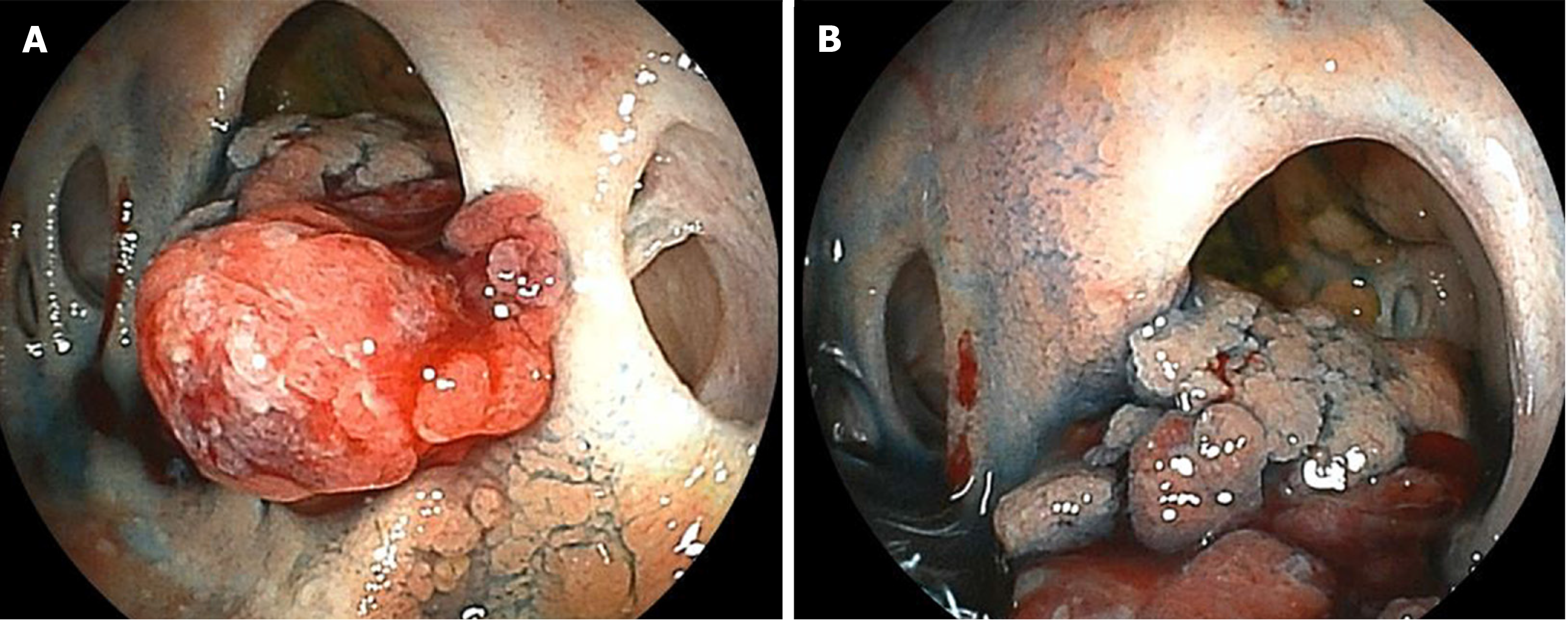
Figure 3 Double balloon enteroscopy shows the cholangiojejunostomy directly.
A: There are four-hole anastomoses: Anterior hole, posterior hole, B2 plus B3 hole, and B4 hole, from right to left. A reddish and hemorrhagic tumor protrudes from the posterior hole; B: The tumor extends inside the posterior branch.
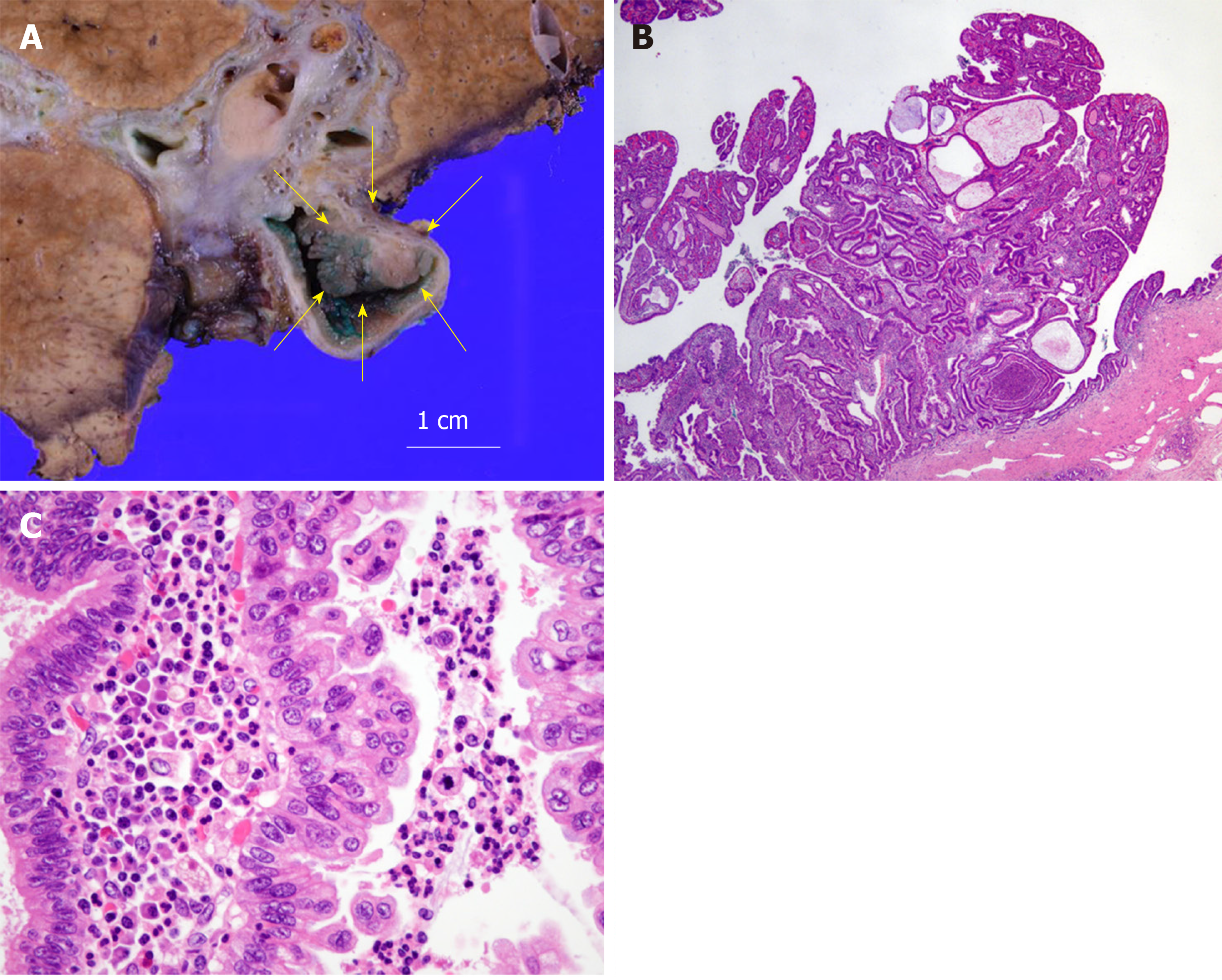
Figure 4 Histological analysis of the tumor.
A: Macroscopic findings; B: Hematoxylin and eosin (HE) staining, × 20; C: HE staining, ×400. Histological studies show papillary growth and fibrovascular cores in the macroscopically nodular area (yellow arrow), comprising high-grade atypical epithelial cells. There is no invasive carcinoma associated with the intraductal neoplasm.
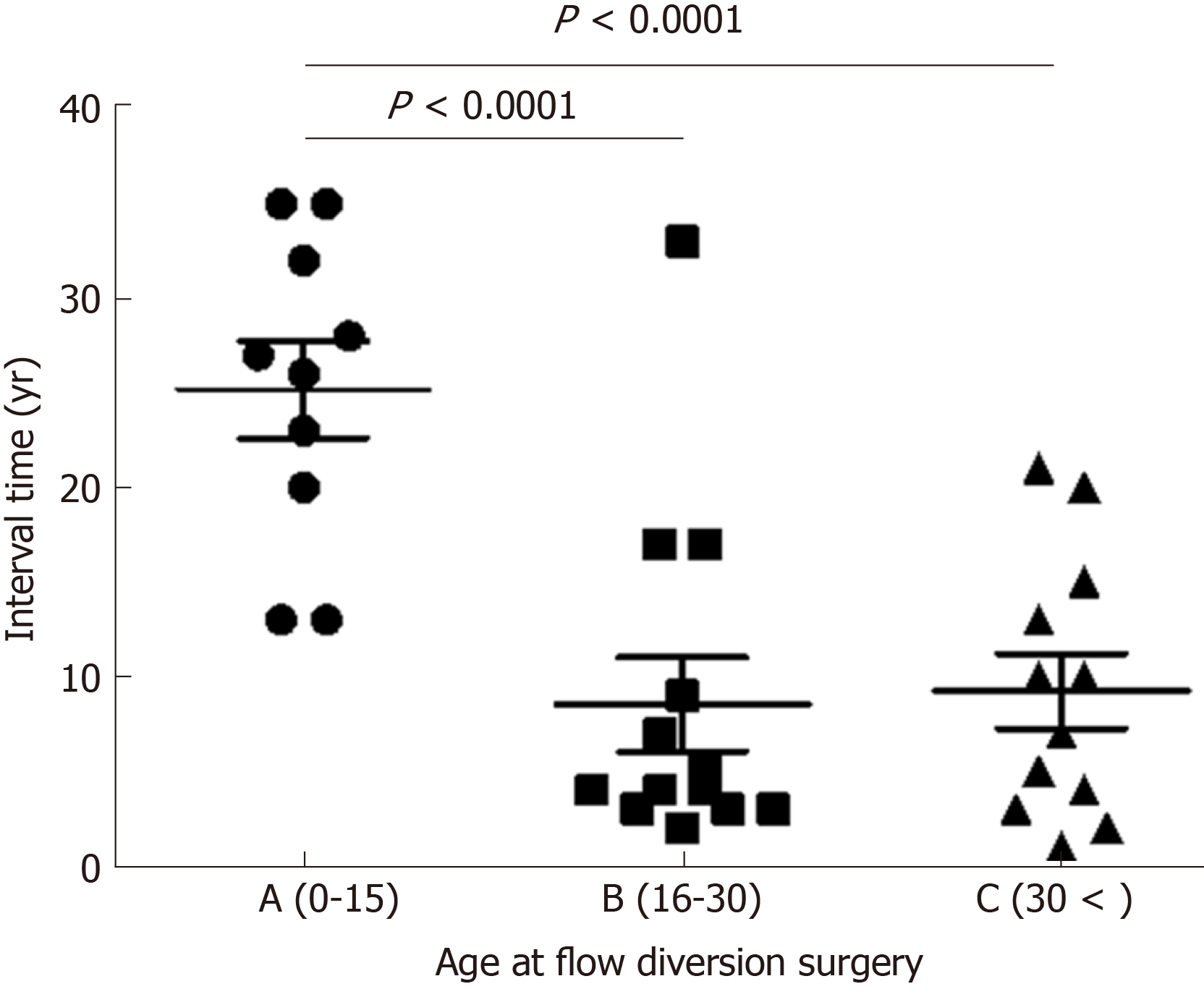
Figure 5 The graph shows the relationship between age at diversion surgery and interval time.
Data represent means and standard deviation. P < 0.0001, one-way analysis of variance and Bonferroni’s multiple comparison test.
- Citation: Ataka R, Ito T, Masui T, Seo S, Ishii T, Ogiso S, Yagi S, Taura K, Uemoto S. Cholangiocarcinoma after flow diversion surgery for congenital biliary dilatation: A case report and review of literature. World J Hepatol 2019; 11(11): 743-751
- URL: https://www.wjgnet.com/1948-5182/full/v11/i11/743.htm
- DOI: https://dx.doi.org/10.4254/wjh.v11.i11.743