Copyright
©The Author(s) 2018.
World J Hepatol. Sep 27, 2018; 10(9): 571-584
Published online Sep 27, 2018. doi: 10.4254/wjh.v10.i9.571
Published online Sep 27, 2018. doi: 10.4254/wjh.v10.i9.571
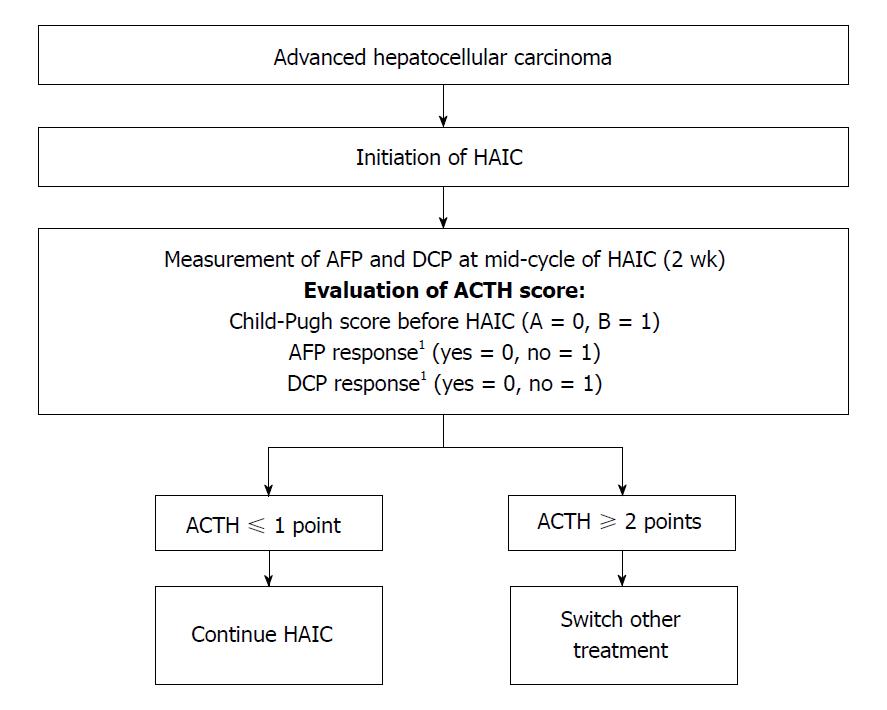
Figure 1 Treatment strategy for advanced hepatocellular carcinoma according to the hepatic arterial infusion chemotherapy score to assess continuous treatment.
The score (range, 0-3) was calculated as follows: Child-Pugh score before hepatic arterial infusion chemotherapy (HAIC) (A = 0, B = 1), alpha-fetoprotein (AFP) response (yes = 0, no = 1), and des-gamma-carboxy prothrombin (DCP) response (yes = 0, no = 1). For patients with a score ≤ 1, HAIC treatment would be continued, while for patients with a score ≥ 2, a second-line therapy such as sorafenib and/or participation in a new clinical trial would be a better option. 1The AFP and DCP responses were assessed 2 wk after HAIC induction; a positive response is defined as a reduction of ≥ 20% from baseline. ACTH: Arterial infusion chemotherapy.
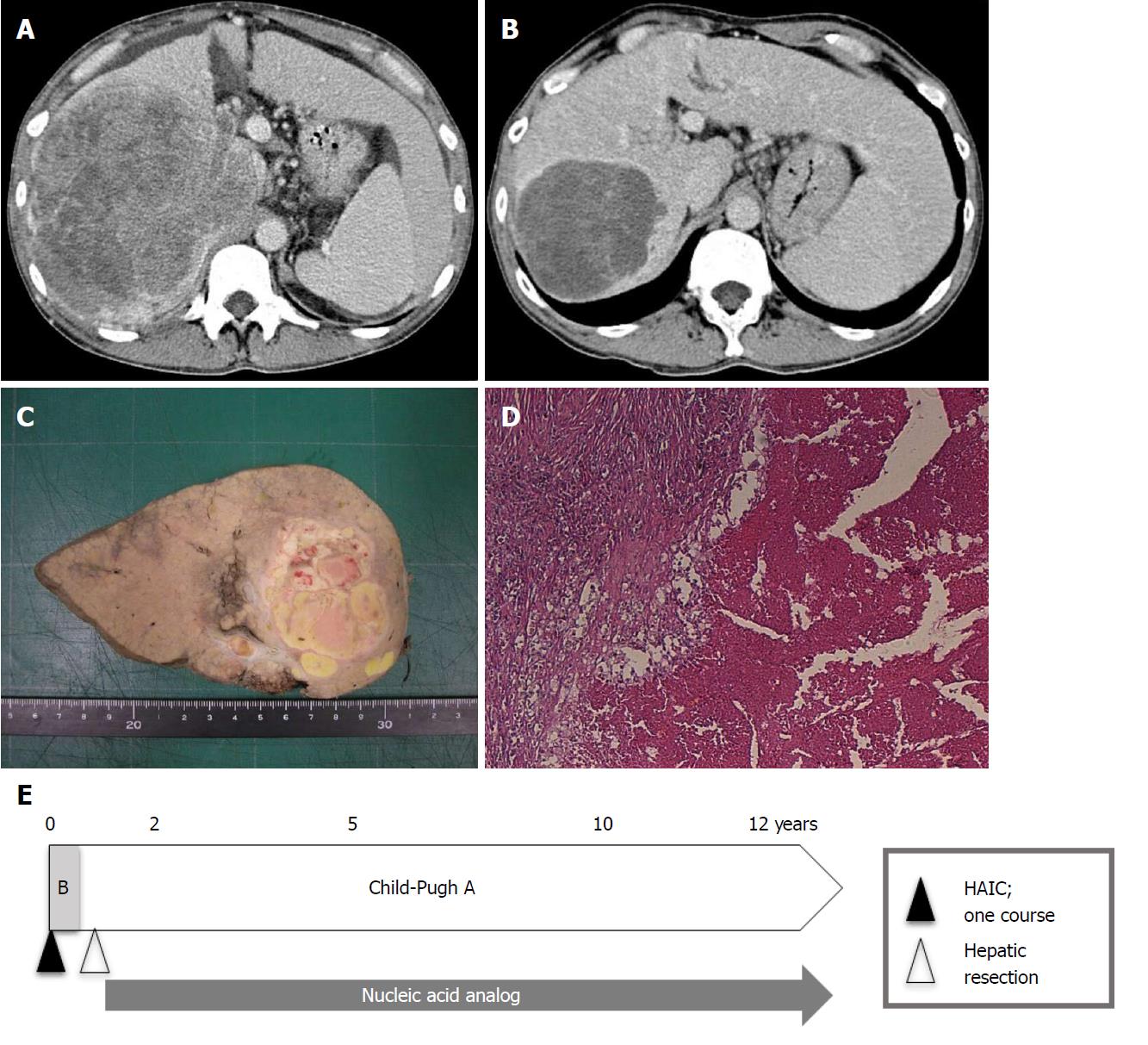
Figure 2 Patient with complete response treated with hepatic arterial infusion chemotherapy using low-dose cisplatin combined with a 5-fluorouracil (low-dose FP)-based regimen.
A: This 44-year-old man had massive hepatocellular carcinoma (HCC) (16 cm in diameter) with tumor thrombosis in the right portal vein (Vp3) and the inferior vena cava (Vv3) on dynamic computed tomography; B: After one course of hepatic arterial infusion chemotherapy (HAIC), the liver tumor markedly decreased; however, as slight tumor vascularity remained, the patient was assessed as having partial response at that time; C, D: Three tumor markers [alpha-fetoprotein (AFP), des-γ-carboxyprothrombin (DCP), and AFP L3] decreased after HAIC (AFP from 7145 ng/mL to 12.7 ng/mL, DCP from 233460 mAU/mL to 51 mAU/mL, AFP L3 from 58.1% to 3.1%). The patient’s Child-Pugh classification improved from B (8 points) to A (5 points). Thus, hepatic resection was performed, and histological findings showed no viable tumor cells (C, D). Finally, the patient was considered to have a complete response; E: The patient has been treated with nucleic acid analogs after the operation, and Child-Pugh A has been maintained. The patient is alive without HCC recurrence 148 mo after HAIC treatment.
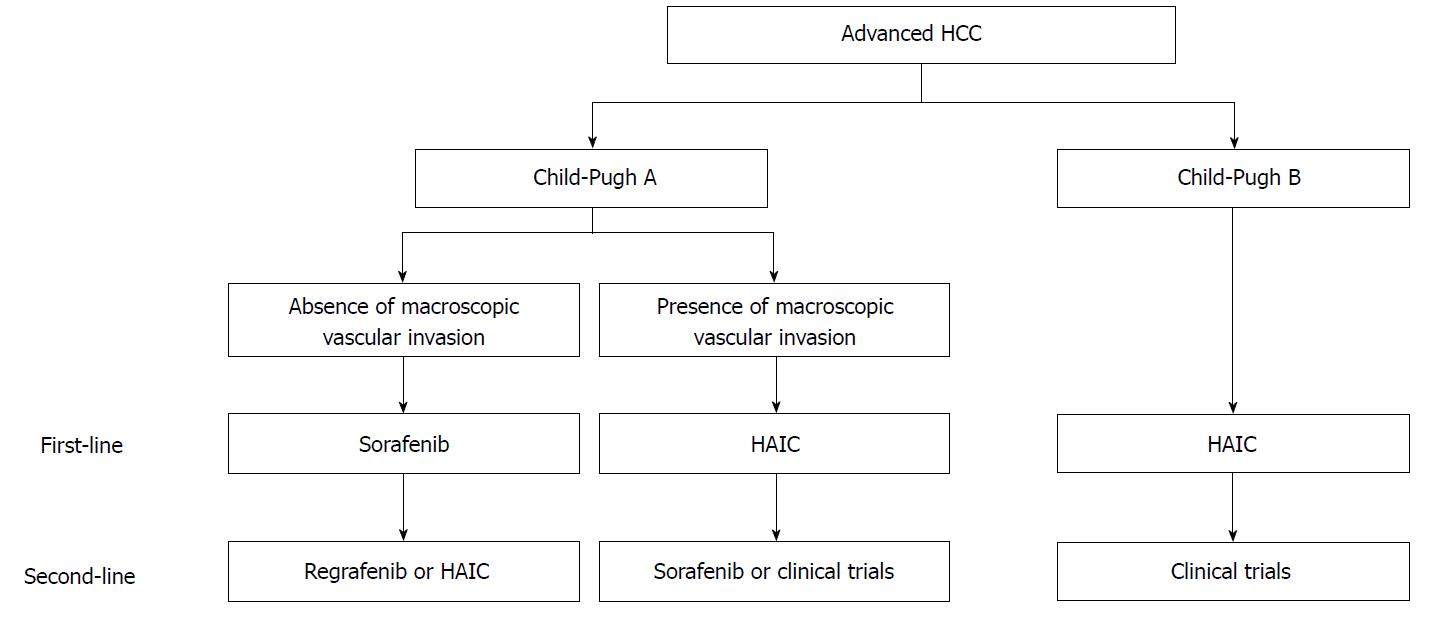
Figure 3 Draft proposal of a treatment strategy for advanced hepatocellular carcinoma.
(1) For advanced hepatocellular carcinoma (HCC) patients without macroscopic vascular invasion and Child-Pugh A, the first-line treatment should be sorafenib, while second-line treatments should be either regorafenib or hepatic arterial infusion chemotherapy (HAIC); (2) For advanced HCC patients with macroscopic vascular invasion and Child-Pugh A, the first-line treatment should be HAIC, and the second-line treatments should be either sorafenib or experimental treatment in clinical trials; (3) For advanced HCC patients with Child-Pugh B, the first-line treatment should be HAIC, and the second-line treatment should be clinical trials.
- Citation: Saeki I, Yamasaki T, Maeda M, Hisanaga T, Iwamoto T, Fujisawa K, Matsumoto T, Hidaka I, Marumoto Y, Ishikawa T, Yamamoto N, Suehiro Y, Takami T, Sakaida I. Treatment strategies for advanced hepatocellular carcinoma: Sorafenib vs hepatic arterial infusion chemotherapy. World J Hepatol 2018; 10(9): 571-584
- URL: https://www.wjgnet.com/1948-5182/full/v10/i9/571.htm
- DOI: https://dx.doi.org/10.4254/wjh.v10.i9.571