修回日期: 2020-06-22
接受日期: 2020-06-24
在线出版日期: 2020-08-08
钛夹预防性夹闭创面对结直肠息肉切除术后迟发性出血及穿孔等不良事件的作用尚不明确, 目前关于钛夹预防作用的有效性尚未达成共识.
评价钛夹对预防结直肠息肉内镜下切除术后不良事件的疗效.
计算机检索PubMed、EMBASE、Cochrane library、万方中关于结直肠息肉术中是否使用钛夹预防术后不良事件的研究, 评价纳入研究质量, 并用Revman 5.3软件进行统计学分析.
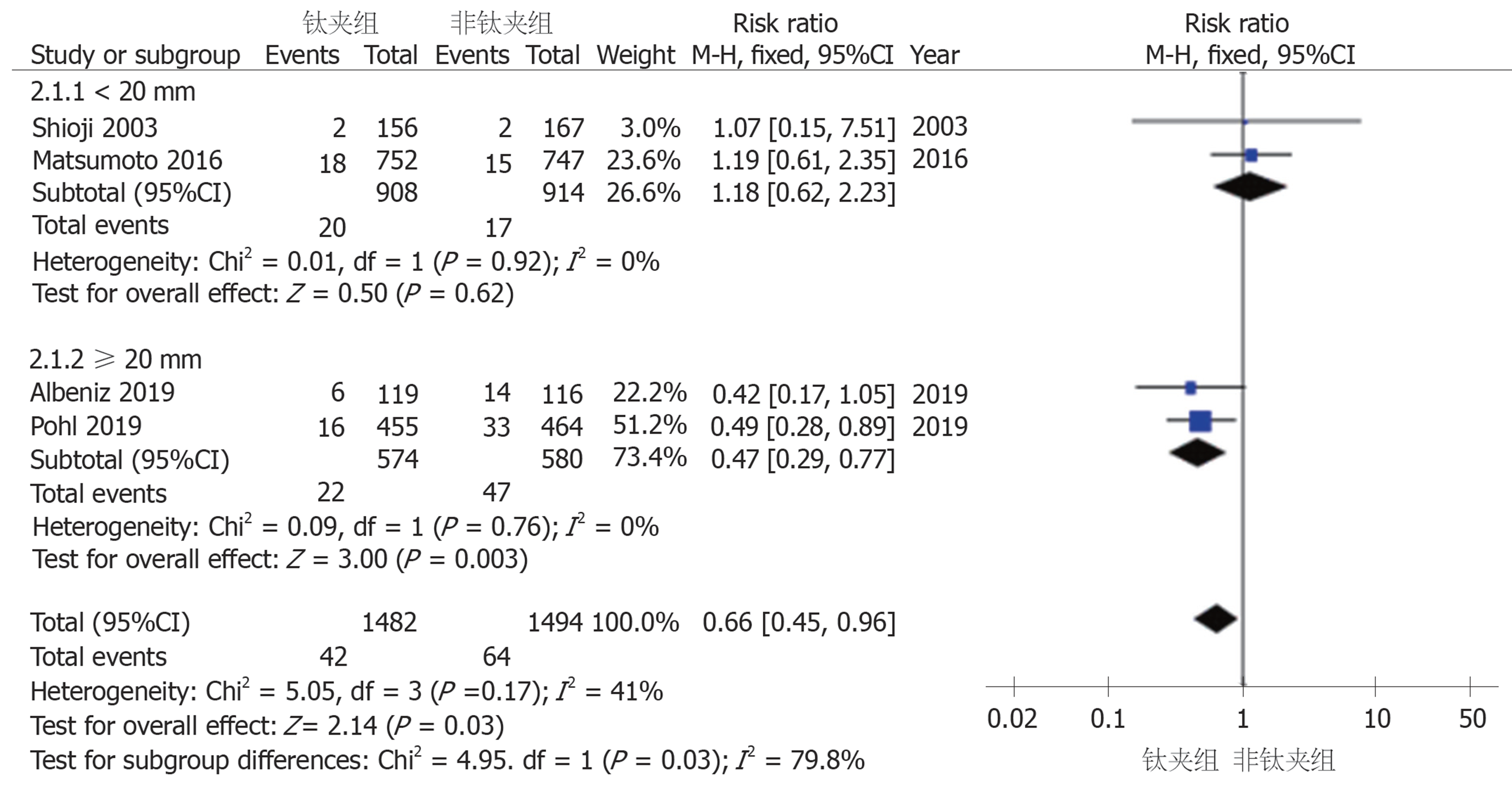
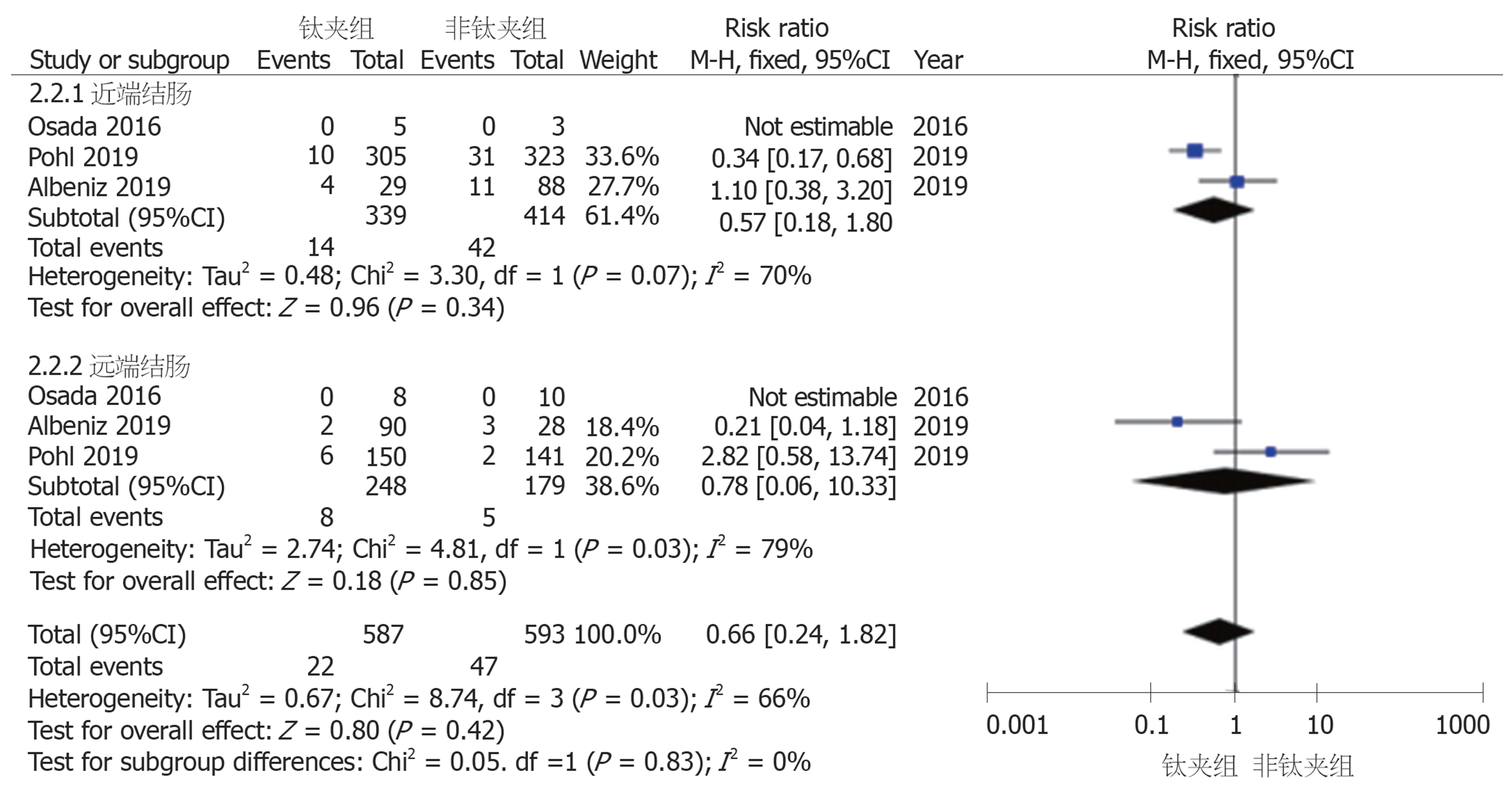
共有7项RCT纳入标准, 共计3777例患者, 1880例患者术中使用钛夹预防性夹闭创面(钛夹组), 1897例患者术中不使用钛夹夹闭创面(非钛夹组). Meta分析结果显示: 钛夹组较非钛夹组的术后迟发性出血率低, 差异具有统计学意义(2.55% vs 4.48%, P = 0.01, 95%CI: 0.40-0.80); 而钛夹组较非钛夹组的术后穿孔率无明显差异(0.66% vs 1.04%, P = 0.42, 95%CI: 0.21-1.92). 亚组分析显示, 钛夹对预防结直肠息肉术后出血的作用, 主要体现在大小≥20 mm的息肉上, 对<20 mm息肉的预防效果不佳(RR = 1.18, 95%CI: 0.62-2.23, P = 0.62; RR = 0.47, 95%CI: 0.29-0.77, P = 0.003); 钛夹对近端结肠息肉与远端结肠息肉切除术后的预防迟发性出血作用无明显差异(RR = 0.57, 95%CI: 0.18-1.80, P = 0.34; RR = 0.78, 95%CI: 0.06-10.33, P = 0.85).
钛夹可预防结直肠息肉切除术后迟发性出血的发生, 且主要体现在≥20 mm的病变中, 此外钛夹对术后穿孔的预防作用不大.
核心提要: 结直肠息肉切除术后不良事件的发生率较高, 而目前关于钛夹预防术后不良事件的有效性尚未达成共识, 本文通过合并既往分析得出结论: 钛夹可预防结直肠息肉切除术后迟发性出血的发生, 但对术后穿孔的预防作用不大.
引文著录: 高利英, 刘希樵, 黄宣. 钛夹预防结直肠息肉切除术后不良事件疗效的Meta分析. 世界华人消化杂志 2020; 28(15): 710-718
Revised: June 22, 2020
Accepted: June 24, 2020
Published online: August 8, 2020
The effect of prophylactic hemoclip placement on the risk of adverse events such as delayed bleeding and perforation after colorectal polypectomy is still unclear. Its efficiency has not been confirmed and there is no consensus on the usefulness of prophylactic clipping.
To assess the efficacy of prophylactic clipping on adverse events after endoscopic resection of colorectal polyps.
We performed a search of PubMed, EMBASE, Cochrane library, and Wanfang databases for studies comparing the effect of clipping vs no clipping on adverse events following endoscopic resection. The quality of the included studies was performed. Statistical analysis was performed using Revman5.3 software.
We identified seven eligible randomized trials from the database search, involving a total of 3777 patients, which included 1880 patients who used prophylactic hemoclips (clip group) and 1897 who did not use (no clip group). Meta-analysis results showed that the delayed bleeding rate of the clip group was significantly lower than that of the no clip group (2.55% vs 4.48%, P = 0.01, 95%CI: 0.40-0.80). There was no significant difference in postoperative perforation rate between the clip group and no clip group (0.66% vs 1.04%, P = 0.42, 95%CI: 0.21-1.92). Subgroup analysis showed that the prophylactic effect on delayed bleeding was mainly observed in polyps with a size of ≥ 20 mm, and the preventive effect in polyps less than 20 mm was poor (RR = 1.18, 95%CI: 0.62-2.23, P = 0.62; RR = 0.47, 95%CI: 0.29-0.77, P = 0.003). There was no significant difference in the effect of prophylactic hemoclips on the prevention of delayed bleeding after resection of proximal and distal colonic polyps (RR = 0.57, 95%CI: 0.18-1.80, P = 0.34; RR = 0.78, 95%CI: 0.06-10.33, P = 0.85).
Prophylactic hemoclips can prevent the occurrence of delayed bleeding after colorectal polypectomy, which is mainly observed in the lesions ≥ 20 mm. In addition, hemoclips have little preventive effect on postoperative perforation.
- Citation: Gao LY, Liu XQ, Huang X. Effect of prophylactic clipping on adverse events after colorectal endoscopic resection: A meta-analysis. Shijie Huaren Xiaohua Zazhi 2020; 28(15): 710-718
- URL: https://www.wjgnet.com/1009-3079/full/v28/i15/710.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v28.i15.710
结直肠癌(colorectal cancer, CRC)是全球第4大恶性肿瘤, 早期对结直肠息肉行内镜下治疗可以降低CRC的发生率与死亡率[1-3]. 目前认为几乎所有结直肠息肉均可通过内镜下切除来治疗, 大多数结肠息肉<10 mm, 可通过常规的圈套息肉切除术安全有效地切除; 而内镜下黏膜切除术(endoscopic mucosal resection, EMR)或内镜黏膜下剥离术(endoscopic submucosal dissection, ESD)多用于治疗≥20 mm的扁平无蒂息肉[4].
消化道息肉的内镜下治疗虽已在国内得到广泛实施, 但结肠镜下息肉切除术后仍会发生诸如出血、穿孔和感染等不良事件[5]. 出血包括术中出血与术后迟发性出血, 术中出血可内镜下凝结、机械疗法或使用稀肾上腺素注射液进行止血; 而对术后迟发性出血尚无明确预防措施. 迟发性出血是指在息肉切除术后30 d内发生的出血, 且需急诊、住院或再次介入进一步治疗[4], 据报道术后迟发性出血的发生率约为1%-6%[6-8]. 结肠穿孔亦是结肠息肉切除术后最严重的并发症之一, 虽然穿孔发生的总体风险较低, 仅为0.2%-1.2%, 但其较高的死亡率与高昂的治疗费用同样需引起我们重视[9,10]. 目前已有多项关于钛夹预防结直肠息肉术后不良事件疗效的研究, Chang等[11]认为钛夹预防性夹闭创面可加快创面愈合, 减少结直肠息肉术后不良事件的发生[12,13], 而Shioji等[14]发现钛夹对预防术后不良事件无明显作用[15,16]. 根据2017年欧洲胃肠道内窥镜学会指南, 不推荐常规钛夹钳夹或其他预防措施防止结直肠息肉切除术后迟发性出血的发生; 同时建议术后仔细检查创面, 若发现穿孔征象或存在危险因素时, 可予钛夹闭合创面以预防术后穿孔[4]. Nishizawa等[17]和Ayoub等[18]曾报道关于预防性钳夹疗效的Meta分析研究, 但二者研究结果不一致, 且近年来又有多项较高质量的RCT研究纳入[13,19,20]. 因此, 为客观公正地评价钛夹对结直肠息肉术后的不良事件发生的预防作用, 我们收集了所有与钛夹预防结直肠息肉术后不良事件相关的随机对照试验进行Meta分析.
1.1.1 纳入标准: (1)研究设计: 随机对照试验; (2)研究对象: 年龄、性别不限; (3)干预措施: 钛夹组(研究组)在结直肠息肉切除术中使用钛夹预防性夹闭创面; 非钛夹组(对照组)为术中不使用钛夹夹闭创面; (4)结局指标: 术后迟发性出血、穿孔的发生率.
1.1.2 排除标准: (1)动物实验; (2)重复发表的文献; (3)数据不完整、无法利用的文献; (4)结局指标不明确的文献; (5)非随机对照试验.
1.2.1 文献检索: 计算机和手工检索PubMed、EMBASE、Cochrane library、万方, 检索日期为建库日期至2020-04. 英文检索词包括"endoscopic mucosal resection or EMR"、"endoscopic submucosal dissection or ESD"、"endoscopic resection or polyp removal or polyp resection or polypectomy", "hemoclip or blood vessel clip or clip or titanium clip or surgical clamps", 中文检索词为"内镜下黏膜切除术"、"内镜黏膜下剥离术"、"息肉切除术"、"ESD"、"EMR"、"钛夹", 同时查阅纳入文献的参考文献, 以补充可能会遗漏的随机对照试验. 根据纳入标准和排除标准, 由其中两名研究员根据检索词分别进行独立检索, 首先删除重复文献, 再根据标题和摘要进行初筛, 排除不符合的文献, 筛选可能纳入的文献, 然后对可能纳入的文献进行全文阅读, 筛选出纳入的文献, 不确定或者存在争议的文献由第三者进行判断.
1.2.2 数据提取与质量评价: 独立提取数据, 并由另一位审阅者对其准确性进行了验证. 任何分歧均以协商一致的方式解决. 从每项研究中提取以下数据: 第一作者, 出版年, 研究设计, 国家, 研究人数, 息肉数目, 年龄, 性别, 手术方式, 息肉大小, 迟发性出血率, 穿孔发生率.
使用Cochrane风险偏倚评估工具评价纳入研究的质量, 分别由两位作者对纳入的研究进行评估. 同样, 如果双方意见不统一, 那么通过讨论来解决, 如果讨论后仍不能确定, 则请第三方介入, 投票决定意见分歧.
1.2.3 敏感性分析: 将纳入研究逐一排除后, 对剩余研究进行Meta分析, 评价汇总敏感性与特异性, 若结果变化不大, 则说明纳入研究的稳定性好; 若结果变化大, 则说明纳入研究的稳定性差.
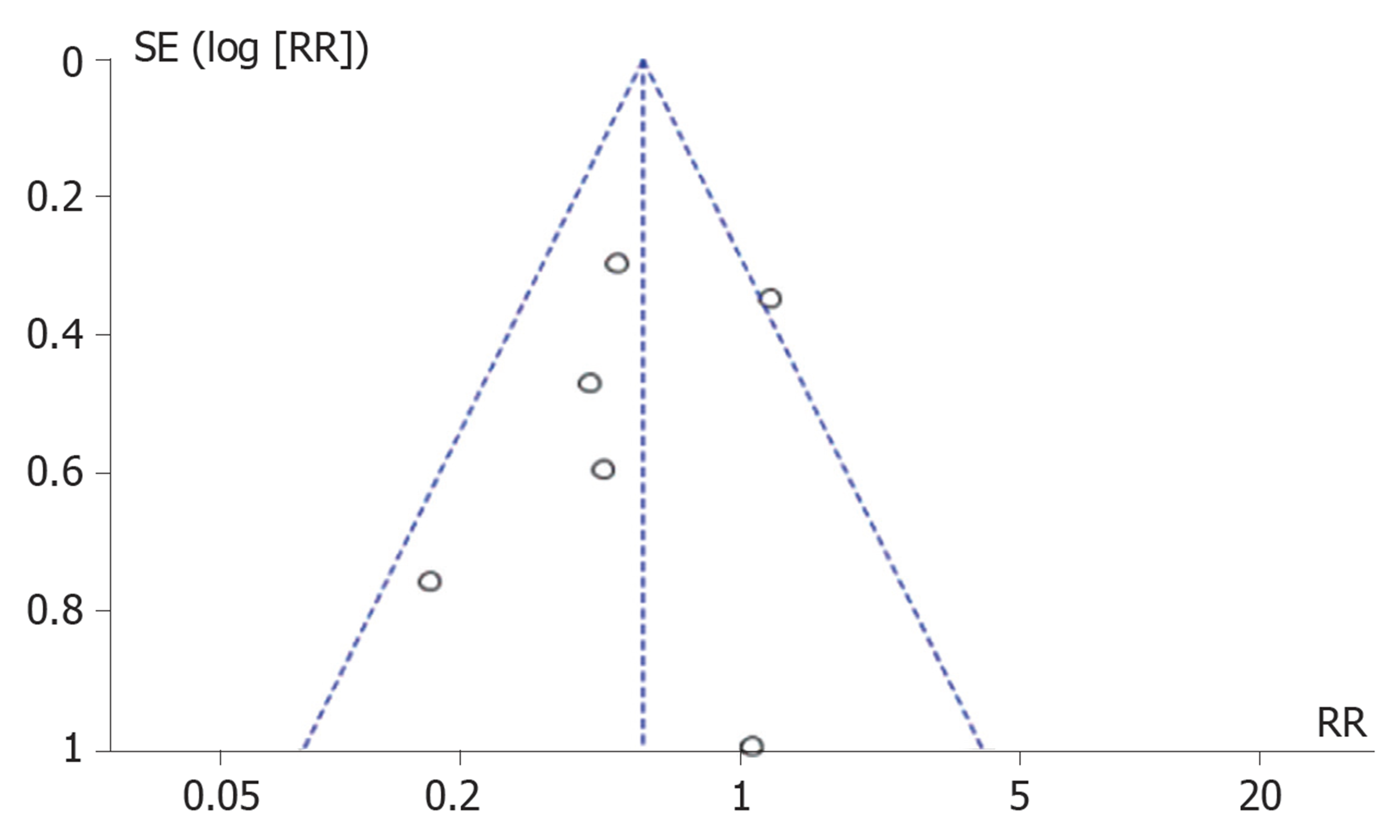
统计学处理 采用Revman 5.3软件进行Meta分析, 首先使用 I2进行异质性检验, 如果I2≥50%, 则认为存在异质性, 可采用随机效应模型. 如果I2<50%, 则认为不存在异质性, 可采用固定效应模型. 对术后迟发性出血、穿孔的发生率采用RR和95%CI进行Meta分析, 并绘制森林图. 偏倚分析: 分别以纳入Meta分析的迟发性出血、穿孔的发生率RR值为横坐标, 以SE (logRR)为纵坐标绘制漏斗图, 通过观察其对称性, 评估发表偏倚的影响.
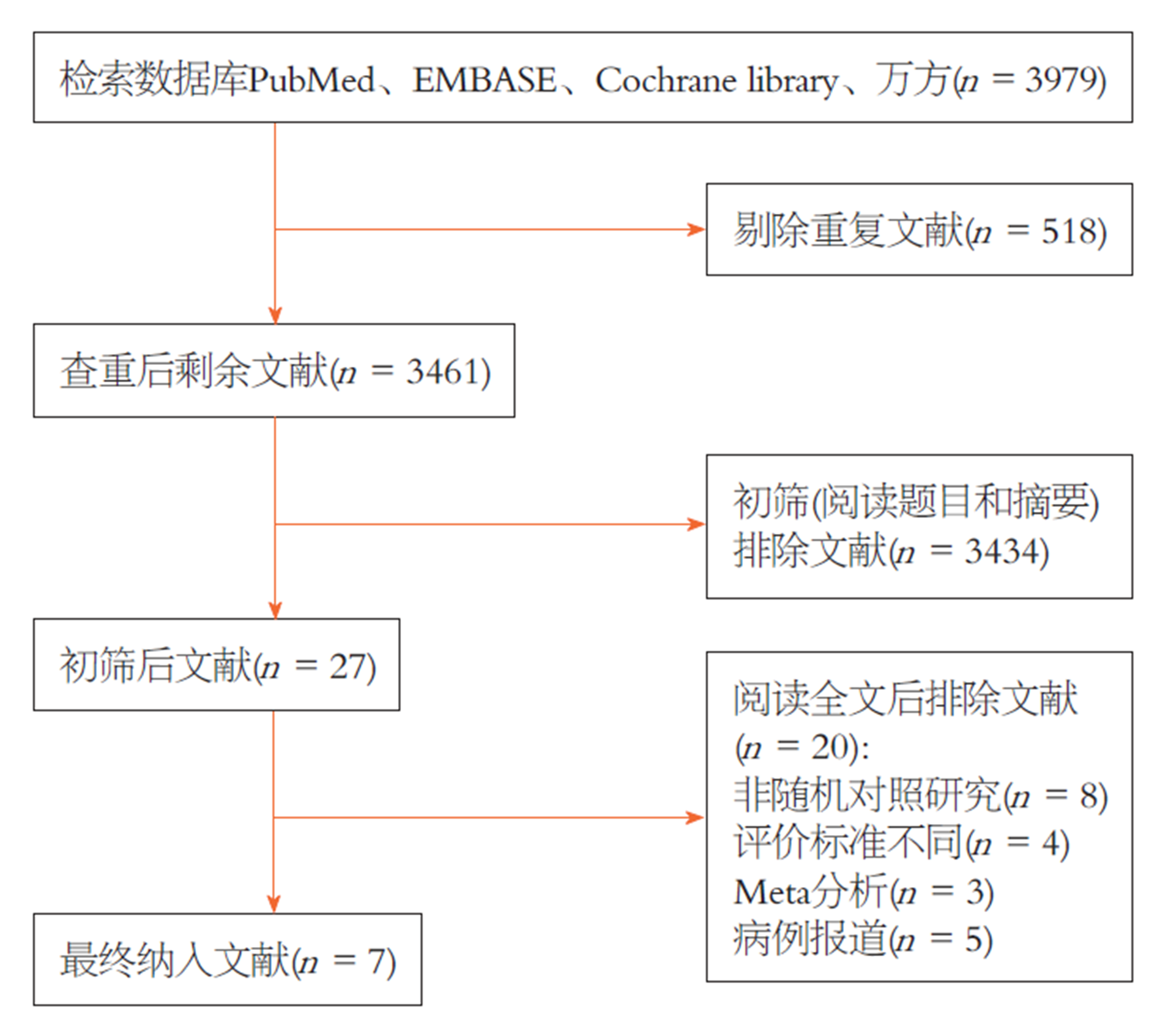
计算机检索共检索出3979篇文章, 通过阅读文献标题和摘要后排除不符合标准的文献3434篇, 重复文献518篇, 通过全文阅读剔除文献20篇, 最终纳7篇随机对照试验[12-14,20-23], 共计3777例患者, 其中1880例患者术中使用钛夹预防性夹闭创面(钛夹组), 1897例患者术中不使用钛夹夹闭创面(非钛夹组). 具体检索过程见图1, 纳入文献的特征见表1.
| Ref. | 国家 | 手术方式 | 纳入息肉的大小 | 组别 | 平均年龄 | 性别(男/女) | 参与人数 | 息肉数目 | 息肉大小(mm) | 迟发性出血 | 穿孔 |
| Shioji等[14], 2003 | 日本 | EMR | <20 mm | 钛夹组 | 64 | 118/38 | 156 | 205 | 7.8 (3.9) | 2 | |
| 非钛夹组 | 63 | 130/17 | 147 | 208 | 7.8 (4.1) | 2 | |||||
| Tominaga等[23], 2014 | 日本 | EMR | >5 mm | 钛夹组 | 67 | 151/60 | 211 | 7.7 (5-30) | 4 | ||
| 非钛夹组 | 67 | 148/68 | 216 | 8.5 (5-35) | 9 | ||||||
| Zhang等[12], 2015 | 中国 | EMR或ESD | 10-40 mm | 钛夹组 | 68 | 112/62 | 174 | 2 | 1 | ||
| 非钛夹组 | 64 | 107/67 | 174 | 12 | 1 | ||||||
| Osada等[21], 2016 | 日本 | ESD | 钛夹组 | 69 | 9/4 | 13 | 13 | 0 | 0 | ||
| 非钛夹组 | 66 | 7/6 | 13 | 13 | 0 | 0 | |||||
| Matsumoto等[22], 2016 | 日本 | EMR或息肉切除术 | <20 mm | 钛夹组 | 65 | 534/218 | 752 | 1636 | 10.7 (5.5) | 18 | |
| 非钛夹组 | 66 | 513/234 | 747 | 1728 | 9.6 (5.3) | 15 | |||||
| Pohl等[20], 2019 | 美国 | EMR | ≥20 mm | 钛夹组 | 65 | 265/190 | 455 | 490 | 30 | 16 | 3 |
| 非钛夹组 | 65 | 282/182 | 464 | 499 | 28 | 33 | 6 | ||||
| Albeniz 2019 | 西班牙 | EMR | ≥20 mm | 钛夹组 | 73 | 61/58 | 119 | 36.1 (14.3) | 6 | 1 | |
| 非钛夹组 | 71 | 73/43 | 116 | 37.3 (12.9) | 14 | 1 |
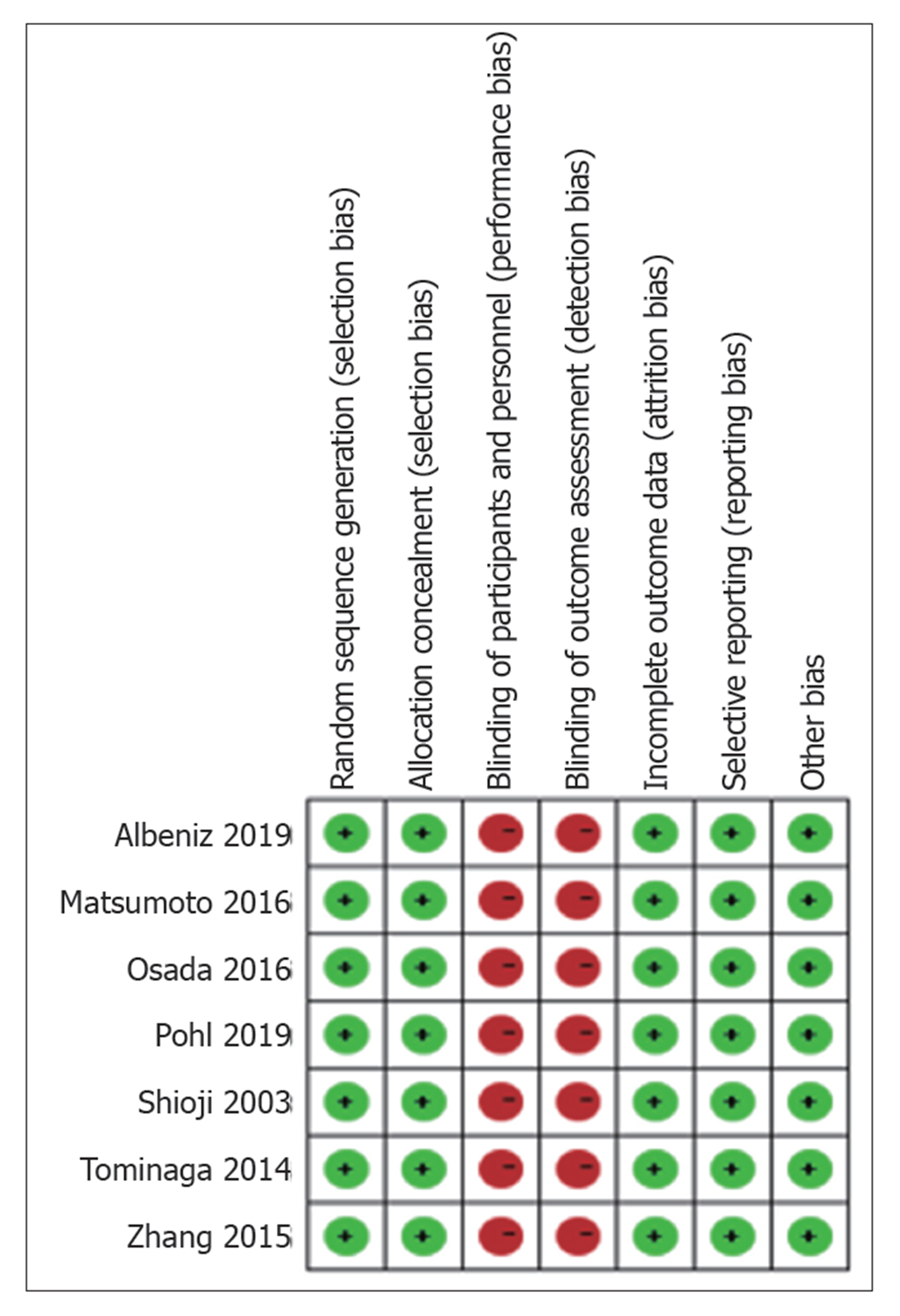
总体而言, 本次报告纳入的7项RCT研究的偏倚风险较低. 所有7项RCT研究均描述了用于随机序列产生和分配隐藏的特定方法, 7项RCT研究中的均未实施单盲或双盲, 因此实施偏倚与测量偏倚均为高风险. 此外, 所有7项RCT都可以充分评估不完整的结果, 避免选择性报告结果, 并且没有其他偏见. 具体风险偏倚结果见图2.
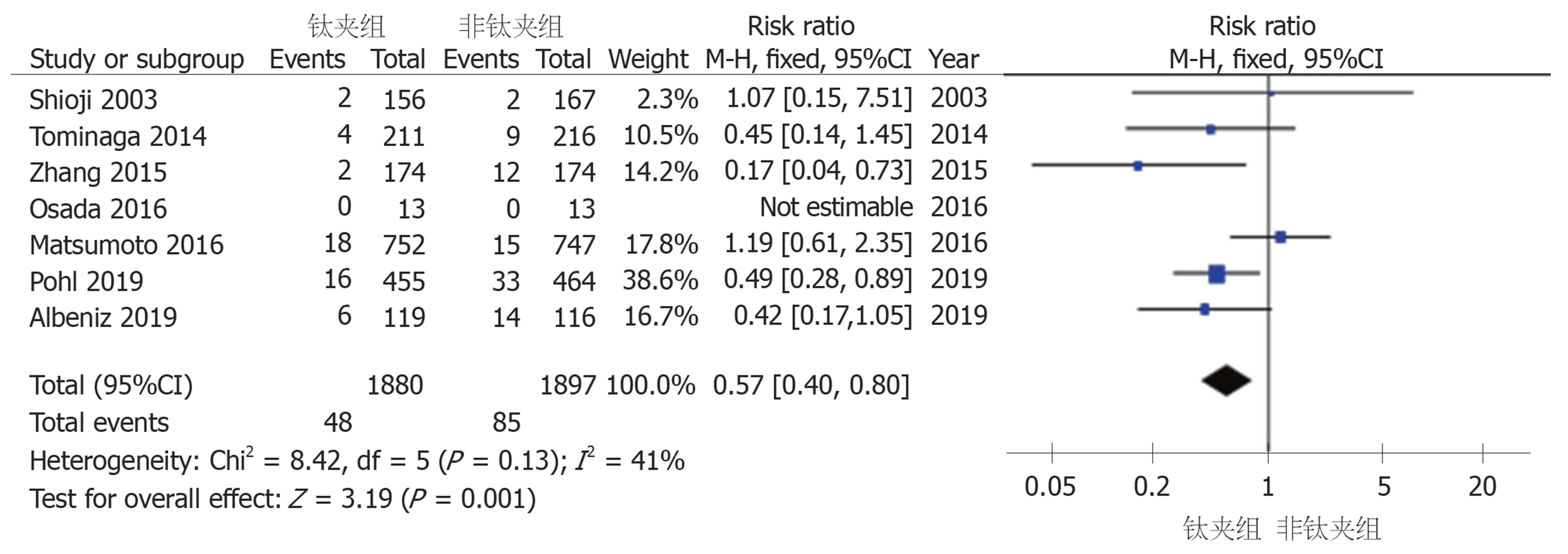
2.3.1 迟发性出血率: Albeniz 2019等7项研究均报道了迟发性出血率, 钛夹组与非钛夹组迟发性出血率分别为2.55%和4.48%, 根据Meta分析结果显示, 各研究组之间异质性较小, 采用固定效应模型进行合并, 得RR值为0.57 (95%CI: 0.40-0.80), P = 0.001, 有统计学差异, 表明使用钛夹预防性夹闭创面可减少结直肠息肉切除术后迟发性出血率, 见图3.
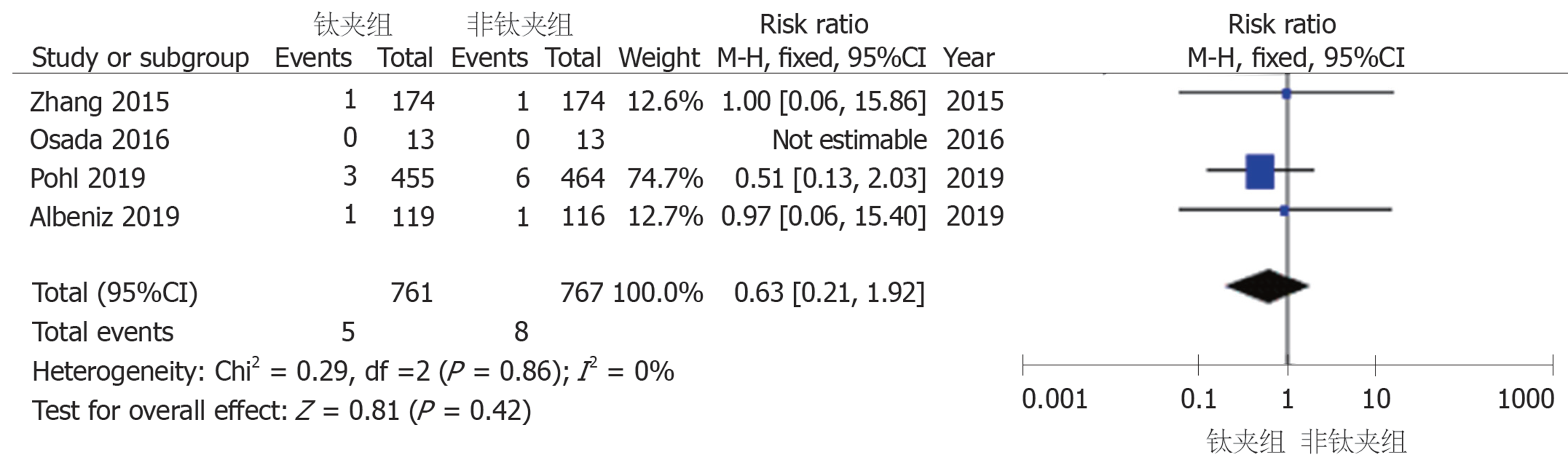
2.3.2 术后穿孔率: Albeniz 2019等4项研究报道了术后穿孔率, 钛夹组与非钛夹组术后穿孔率分别为0.66%和1.04%, 根据Meta分析结果显示, 各研究组之间不存在异质性, 采用固定效应模型进行合并, 得RR值为0.63 (95%CI: 0.21-1.92), P = 0.42, 没有统计学差异. 表明钛夹预防性夹闭创面不能减少结直肠息肉术后穿孔率, 见图4.
2.3.3 不同息肉大小对于术后迟发性出血率的亚组分析: 4项RCT研究提供了息肉大小与术后迟发性出血的可用数据, 其中Albeniz 2019等2项研究中提取到息肉<20 mm的相关数据, 包括钛夹组574例, 非钛夹组580例; Matsumoto 2016等2项研究中提取到结直肠息肉≥20 mm的相关数据, 包括钛夹组908例, 非钛夹组914例. 根据息肉的不同大小进行亚组分组(见图5, 结果表明钛夹对预防结直肠息肉术后出血的作用, 主要体现在≥20 mm的息肉上, 对<20 mm息肉的预防作用不大(RR = 1.18, 95%CI: 0.62-2.23, P = 0.62; RR = 0.47, 95%CI: 0.29-0.77, P = 0.003).
2.3.4 不同部位息肉对于术后迟发性出血的亚组分析: 将盲肠、升结肠及肝曲定义为近端结肠, 剩余为远端结肠. Albeniz 2019等3项RCT研究提供了息肉部位与术后迟发性出血的可用数据, 其中近端结肠的相关数据, 包括钛夹组339例, 非钛夹组414例; 远端结肠的相关数据, 包括钛夹组248例, 非钛夹组179例. 根据息肉的不同位置进行亚组分组(见图6), 结果表明钛夹对近端结肠息肉与远端结肠息肉切除术后的预防迟发性出血作用无明显差异(RR = 0.57, 95%CI: 0.18-1.80, P = 0.34; RR = 0.78, 95%CI: 0.06-10.33, P = 0.85).
逐一排除每一个文献后进行Meta分析, 结果显示敏感性和特异性未见明显改变, 表明纳入文献稳定性好.
迟发性出血、穿孔是结直肠息肉切除术后常见的并发症, 目前关于钛夹预防作用的有效性尚未达成共识, 本项Meta分析显示, 结直肠息肉切除术后使用钛夹夹闭创面可预防术后迟发性出血的发生, 但对结肠穿孔的预防效果不大.
理论上讲, 息肉切除术后钛夹夹闭创面可减少黏膜下组织暴露于结肠腔, 加快创面愈合, 减少出血与穿孔的发生, 但亦有钛夹掉落导致黏膜破坏引发术后出血的风险[12,24,25]. 近年来多项病例对照试验与RCT研究均试图探究钛夹对息肉切除术后的预防作用[11,13,19,20,26], 本次研究中纳入了7项RCT研究. 有研究表明, 术后迟发性出血的影响因素包括患者年龄, 基础疾病, 术前使用抗血小板或抗凝剂, 病变大小与位置等多种因素[27-29], 尤其是病变≥20 mm者[30,31], 因此本研究亚组分析了钛夹夹闭创面对不同大小与部位的息肉预防迟发性出血的效果. 同样, 术后穿孔的发生很大程度上取决于病变大小与手术技术, 其他包括患者年龄、合并症、病变的形态与位置等, 但因纳入研究的术后穿孔率很低, 故本研究未对穿孔行进一步亚组分析. 本项Meta分析发现, 钛夹预防性夹闭创面可减少结直肠息肉切除术后的迟发性出血率, 且预防作用主要体现在≥20 mm的病变中, 而对不同部位息肉的预防效果无明显差异, 此外钛夹对术后穿孔的预防作用不大.
Nishizawa等[17]曾报道了对结直肠息肉切除术后预防性钳夹疗效的Meta分析, 总纳入7项RCT, 共计3059例患者, 结果表明钛夹组(2.1%)与无钛夹组(2.7%)二者的迟发性出血率相似(OR = 0.76, 95%CI: 0.39-1.47, P = 0.41). 这与本研究分析结果不同, 分析原因Nishizawa等[17]人纳入RCT研究中所包含的息肉大小几乎均<20 mm, 且其中2项研究评价标准不同. 同样, 当本次Meta分析仅包含息肉<20 mm时, 钛夹对预防术后迟发性出血亦无效(RR = 1.18, 95%CI: 0.62-2.23, P = 0.62), 故可以解释Nishizawa等[17]人的分析结果. Ayoub等人[18]也曾报道了相关Meta分析, 总纳入6项病例对照试验, 7项RCT, 提取息肉≥20 mm相关数据, Meta分析同本研究结果一致, 表明钛夹组能降低结直肠息肉术后迟发性出血率(OR = 0.24, 95%CI: 0.12-0.50, P < 0.001); 同样提取钛夹预防术后穿孔相关数据, 结果同本研究一致, 亦无明显预防效果(OR = 1.05; 95%CI: 0.15-7.48, P = 0.96). Ayoub等人的研究纳入了病例对照试验, 且其中3项RCT研究评价标准不同, 相比其本研究新增了近年来相关RCT并剔除了不同评价标准的研究, 结果更有信服力.
这项Meta分析有几个优势, 首先该研究是仅针对RCT的Meta分析, 且在纳入文献上新纳入了近年来2项高质量RCT; 其次, 鉴于迟发性出血常出现在较大息肉切除术后, 本项研究分析了不同大小的息肉对预防性夹闭创面的效果, 并欣喜的发现钛夹对预防息肉切除术后迟发性出血的作用主要体现在≥20 mm的息肉中. 但本研究仍存在一些不足, 首现纳入研究的手术方式主要为EMR, 而EMR、ESD及常规息肉切除术三者之间有明显区别[32-34], 因此需要更多研究进一步明确; 其次, 缺乏有关患者术前抗血小板药物的使用、息肉形态的数据, 无法评价关于迟发性出血其他重要影响因素在本研究中的作用; 最后, 虽然结果表明钛夹对预防息肉切除术后出血有明显疗效, 但需考虑成本与效益关系后才能最终指导临床实践.
总之, 这项Meta分析表明, 预防性钳夹可减少结直肠息肉切除术后迟发性出血率, 且其预防作用主要体现在≥20 mm的病变中, 但对术后穿孔的预防作用不大. 但仍需要更多高质量的试验, 以进一步确息肉切除术后迟发性出血的风险因素, 并帮助实施具有成本效益的预防策略.
结直肠息肉是消化道最常见的疾病之一, 著名的"大肠腺瘤到癌顺序演变的分子遗传学模式", 表明大多数结直肠癌由腺瘤性息肉癌变而来. 因此, 通过内窥镜技术对结肠息肉的早期检出并及时治疗对防治结肠癌具有重要意义. 而目前结直肠息肉切除术后出血、穿孔等发生率仍较高, 故有必要探究降低息肉切除术后不良事件发生率的有效预防措施.
有研究提示钛夹夹闭创面可以加快创口愈合预防结直肠息肉术后不良事件的发生, 但对此尚未达成共识. 目前国内相关研究报道较少, 至今尚未有相关Meta分析的研究报道. 本研究可通过明确钛夹预防作用的有效性, 对未来临床实践提供理论依据.
通过合并既往国内外相关研究, 探究钛夹夹闭创面对预防结直肠息肉术后不良事件的疗效, 为提高结直肠息肉切除术的安全性提供临床依据.
通过检索PubMed、 EMBASE、 Cochrane library、 万方等中英文数据库, 收集钛夹预防结直肠息肉切除术后不良事件的所有文献, 应用Revman 5.3软件进行Meta分析.
本项Meta分析结果显示, 钛夹预防性夹闭创面可以减少结直肠息肉切除术后迟发性出血的发生, 其中钛夹对不同大小的息肉的疗效不同, 对预防≥20 mm的病变术后出血的效果更佳, 但钛夹对结直肠息肉术后穿孔的预防作用不大.
既往已有研究试图明确钛夹对预防结直肠息肉切除术后不良事件的疗效, 但结论并不一致. 本项研究结果显示钛夹可以预防息肉切除术后不良事件的发生, 尤其对预防术后迟发性出血有明显疗效, 这为今后指导临床实践提供重要依据.
本次的Meta分析有一些不足, 部分纳入研究数据获取不全, 质量不高, 导致部分结果存在异质性. 因此今后研究中仍需要更多高质量的文献, 以进一步确息肉切除术后不良事件的风险因素, 并帮助实施具有成本效益的预防策略.
学科分类: 胃肠病学和肝病学
手稿来源地: 浙江省
同行评议报告学术质量分类
A级 (优秀): 0
B级 (非常好): 0
C级 (良好): C, C
D级 (一般): 0
E级 (差): 0
科学编辑: 张晗 制作编辑:刘继红
| 1. | Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019;394:1467-1480. [PubMed] [DOI] |
| 2. | Song M, Emilsson L, Bozorg SR, Nguyen LH, Joshi AD, Staller K, Nayor J, Chan AT, Ludvigsson JF. Risk of colorectal cancer incidence and mortality after polypectomy: a Swedish record-linkage study. Lancet Gastroenterol Hepatol. 2020;5:537-547. [PubMed] [DOI] |
| 3. | Zauber AG, Winawer SJ, O'Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, Shi W, Bond JH, Schapiro M, Panish JF, Stewart ET, Waye JD. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687-696. [PubMed] [DOI] |
| 4. | Ferlitsch M, Moss A, Hassan C, Bhandari P, Dumonceau JM, Paspatis G, Jover R, Langner C, Bronzwaer M, Nalankilli K, Fockens P, Hazzan R, Gralnek IM, Gschwantler M, Waldmann E, Jeschek P, Penz D, Heresbach D, Moons L, Lemmers A, Paraskeva K, Pohl J, Ponchon T, Regula J, Repici A, Rutter MD, Burgess NG, Bourke MJ. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017;49:270-297. [PubMed] [DOI] |
| 5. | Sethi A, Song LM. Adverse events related to colonic endoscopic mucosal resection and polypectomy. Gastrointest Endosc Clin N Am. 2015;25:55-69. [PubMed] [DOI] |
| 6. | Burgess NG, Williams SJ, Hourigan LF, Brown GJ, Zanati SA, Singh R, Tam W, Butt J, Byth K, Bourke MJ. A management algorithm based on delayed bleeding after wide-field endoscopic mucosal resection of large colonic lesions. Clin Gastroenterol Hepatol. 2014;12:1525-1533. [PubMed] [DOI] |
| 7. | Albéniz E, Fraile M, Ibáñez B, Alonso-Aguirre P, Martínez-Ares D, Soto S, Gargallo CJ, Ramos Zabala F, Álvarez MA, Rodríguez-Sánchez J, Múgica F, Nogales Ó, Herreros de Tejada A, Redondo E, Pin N, León-Brito H, Pardeiro R, López-Roses L, Rodríguez-Téllez M, Jiménez A, Martínez-Alcalá F, García O, de la Peña J, Ono A, Alberca de Las Parras F, Pellisé M, Rivero L, Saperas E, Pérez-Roldán F, Pueyo Royo A, Eguaras Ros J, Zúñiga Ripa A, Concepción-Martín M, Huelin-Álvarez P, Colán-Hernández J, Cubiella J, Remedios D, Bessa I Caserras X, López-Viedma B, Cobian J, González-Haba M, Santiago J, Martínez-Cara JG, Valdivielso E, Guarner-Argente C; Endoscopic Mucosal Resection Endoscopic Spanish Society Group. A Scoring System to Determine Risk of Delayed Bleeding After Endoscopic Mucosal Resection of Large Colorectal Lesions. Clin Gastroenterol Hepatol. 2016;14:1140-1147. [PubMed] [DOI] |
| 8. | Levin TR, Zhao W, Conell C, Seeff LC, Manninen DL, Shapiro JA, Schulman J. Complications of colonoscopy in an integrated health care delivery system. Ann Intern Med. 2006;145:880-886. [PubMed] [DOI] |
| 9. | Amato A, Radaelli F, Dinelli M, Crosta C, Cengia G, Beretta P, Devani M, Lochis D, Manes G, Fini L, Paggi S, Passoni GR, Repici A; SIED Lombardy group. Early and delayed complications of polypectomy in a community setting: The SPoC prospective multicentre trial. Dig Liver Dis. 2016;48:43-48. [PubMed] [DOI] |
| 10. | Heldwein W, Dollhopf M, Rösch T, Meining A, Schmidtsdorff G, Hasford J, Hermanek P, Burlefinger R, Birkner B, Schmitt W; Munich Gastroenterology Group. The Munich Polypectomy Study (MUPS): prospective analysis of complications and risk factors in 4000 colonic snare polypectomies. Endoscopy. 2005;37:1116-1122. [PubMed] [DOI] |
| 11. | Chang K, Lee BS, Tekeste T, Nguyen A, Adeyemo M, Girgis A, Kwok KK, Crowson HM, Burris AO, Attam R, Chaya CT, Durbin TE, Giap AQ, Hunt GC, Iskander J, Kao KT, Lim BS. The effect of prophylactic hemoclips on the risk of delayed post-endoscopic mucosal resection bleed for upper and lower gastrointestinal lesions: a retrospective cohort study. BMC Gastroenterol. 2020;20:60. [PubMed] [DOI] |
| 12. | Zhang QS, Han B, Xu JH, Gao P, Shen YC. Clip closure of defect after endoscopic resection in patients with larger colorectal tumors decreased the adverse events. Gastrointest Endosc. 2015;82:904-909. [PubMed] [DOI] |
| 13. | Albéniz E, Álvarez MA, Espinós JC, Nogales O, Guarner C, Alonso P, Rodríguez-Téllez M, Herreros de Tejada A, Santiago J, Bustamante-Balén M, Rodríguez Sánchez J, Ramos-Zabala F, Valdivielso E, Martínez-Alcalá F, Fraile M, Elosua A, Guerra Veloz MF, Ibáñez Beroiz B, Capdevila F, Enguita-Germán M. Clip Closure After Resection of Large Colorectal Lesions With Substantial Risk of Bleeding. Gastroenterology. 2019;157:1213-1221.e4. [PubMed] [DOI] |
| 14. | Shioji K, Suzuki Y, Kobayashi M, Nakamura A, Azumaya M, Takeuchi M, Baba Y, Honma T, Narisawa R. Prophylactic clip application does not decrease delayed bleeding after colonoscopic polypectomy. Gastrointest Endosc. 2003;57:691-694. [PubMed] [DOI] |
| 15. | Dokoshi T, Fujiya M, Tanaka K, Sakatani A, Inaba Y, Ueno N, Kashima S, Goto T, Sasajima J, Tominaga M, Ito T, Moriichi K, Tanabe H, Ikuta K, Ohtake T, Kohgo Y. A randomized study on the effectiveness of prophylactic clipping during endoscopic resection of colon polyps for the prevention of delayed bleeding. Biomed Res Int. 2015;2015:490272. [PubMed] [DOI] |
| 16. | Mori H, Kobara H, Nishiyama N, Fujihara S, Matsunaga T, Ayaki M, Chiyo T, Masaki T. Simple and reliable treatment for post-EMR artificial ulcer floor with snare cauterization for 10- to 20-mm colorectal polyps: a randomized prospective study (with video). Surg Endosc. 2015;29:2818-2824. [PubMed] [DOI] |
| 17. | Nishizawa T, Suzuki H, Goto O, Ogata H, Kanai T, Yahagi N. Effect of prophylactic clipping in colorectal endoscopic resection: A meta-analysis of randomized controlled studies. United European Gastroenterol J. 2017;5:859-867. [PubMed] [DOI] |
| 18. | Ayoub F, Westerveld DR, Forde JJ, Forsmark CE, Draganov PV, Yang D. Effect of prophylactic clip placement following endoscopic mucosal resection of large colorectal lesions on delayed polypectomy bleeding: A meta-analysis. World J Gastroenterol. 2019;25:2251-2263. [PubMed] [DOI] |
| 19. | Soh JS, Seo M, Kim KJ. Prophylactic clip application for large pedunculated polyps before snare polypectomy may decrease immediate postpolypectomy bleeding. BMC Gastroenterol. 2020;20:68. [PubMed] [DOI] |
| 20. | Pohl H, Grimm IS, Moyer MT, Hasan MK, Pleskow D, Elmunzer BJ, Khashab MA, Sanaei O, Al-Kawas FH, Gordon SR, Mathew A, Levenick JM, Aslanian HR, Antaki F, von Renteln D, Crockett SD, Rastogi A, Gill JA, Law RJ, Elias PA, Pellise M, Wallace MB, Mackenzie TA, Rex DK. Clip Closure Prevents Bleeding After Endoscopic Resection of Large Colon Polyps in a Randomized Trial. Gastroenterology. 2019;157:977-984.e3. [PubMed] [DOI] |
| 21. | Osada T, Sakamoto N, Ritsuno H, Murakami T, Ueyama H, Matsumoto K, Shibuya T, Ogihara T, Watanabe S. Closure with clips to accelerate healing of mucosal defects caused by colorectal endoscopic submucosal dissection. Surg Endosc. 2016;30:4438-4444. [PubMed] [DOI] |
| 22. | Matsumoto M, Kato M, Oba K, Abiko S, Tsuda M, Miyamoto S, Mizushima T, Ono M, Omori S, Takahashi M, Ono S, Mabe K, Nakagawa M, Nakagawa S, Kudo T, Shimizu Y, Sakamoto N. Multicenter randomized controlled study to assess the effect of prophylactic clipping on post-polypectomy delayed bleeding. Dig Endosc. 2016;28:570-576. [PubMed] [DOI] |
| 23. | Tominaga N, Tanaka Y, Higuchi T. The effect of hemostasis clipping post endoscopic mucosal resection of colorectal polyps. Gastroenterol Endosc. 2014;56:15-20. |
| 24. | Turan AS, Ultee G, Van Geenen EJM, Siersema PD. Clips for managing perforation and bleeding after colorectal endoscopic mucosal resection. Expert Rev Med Devices. 2019;16:493-501. [PubMed] [DOI] |
| 25. | Ponugoti PL, Rex DK. Clip retention rates and rates of residual polyp at the base of retained clips on colorectal EMR sites. Gastrointest Endosc. 2017;85:530-534. [PubMed] [DOI] |
| 26. | Feagins LA, Smith AD, Kim D, Halai A, Duttala S, Chebaa B, Lunsford T, Vizuete J, Mara M, Mascarenhas R, Meghani R, Kundrotas L, Dunbar KB, Cipher DJ, Harford WV, Spechler SJ. Efficacy of Prophylactic Hemoclips in Prevention of Delayed Post-Polypectomy Bleeding in Patients With Large Colonic Polyps. Gastroenterology. 2019;157:967-976.e1. [PubMed] [DOI] |
| 27. | Park SK, Seo JY, Lee MG, Yang HJ, Jung YS, Choi KY, Kim H, Kim HO, Jung KU, Chun HK, Park DI. Prospective analysis of delayed colorectal post-polypectomy bleeding. Surg Endosc. 2018;32:3282-3289. [PubMed] [DOI] |
| 28. | Jaruvongvanich V, Prasitlumkum N, Assavapongpaiboon B, Suchartlikitwong S, Sanguankeo A, Upala S. Risk factors for delayed colonic post-polypectomy bleeding: a systematic review and meta-analysis. Int J Colorectal Dis. 2017;32:1399-1406. [PubMed] [DOI] |
| 29. | Gimeno-García AZ, de Ganzo ZA, Sosa AJ, Pérez DN, Quintero E. Incidence and predictors of postpolypectomy bleeding in colorectal polyps larger than 10 mm. Eur J Gastroenterol Hepatol. 2012;24:520-526. [PubMed] [DOI] |
| 30. | Sawhney MS, Salfiti N, Nelson DB, Lederle FA, Bond JH. Risk factors for severe delayed postpolypectomy bleeding. Endoscopy. 2008;40:115-119. [PubMed] [DOI] |
| 31. | Fujiya M, Sato H, Ueno N, Sakatani A, Tanaka K, Dokoshi T, Fujibayashi S, Nomura Y, Kashima S, Gotoh T, Sasajima J, Moriichi K, Watari J, Kohgo Y. Efficacy and adverse events of cold vs hot polypectomy: A meta-analysis. World J Gastroenterol. 2016;22:5436-5444. [PubMed] [DOI] |
| 32. | Ma MX, Bourke MJ. Complications of endoscopic polypectomy, endoscopic mucosal resection and endoscopic submucosal dissection in the colon. Best Pract Res Clin Gastroenterol. 2016;30:749-767. [PubMed] [DOI] |
| 33. | Chen WC, Wallace MB. Endoscopic management of mucosal lesions in the gastrointestinal tract. Expert Rev Gastroenterol Hepatol. 2016;10:481-495. [PubMed] [DOI] |
| 34. | Amato A, Radaelli F, Correale L, Di Giulio E, Buda A, Cennamo V, Fuccio L, Devani M, Tarantino O, Fiori G, De Nucci G, De Bellis M, Hassan C, Repici A; Bowell Group. Intra-procedural and delayed bleeding after resection of large colorectal lesions: The SCALP study. United European Gastroenterol J. 2019;7:1361-1372. [PubMed] [DOI] |