修回日期: 2014-04-05
接受日期: 2014-04-14
在线出版日期: 2014-06-08
肛瘘是最常见的肛周疾病之一, 其术前评估方法多种多样, 传统方法包括查体、探针探查、Goodsall定律、亚甲蓝试验等, 尽管传统方法发挥了一定的作用, 但其对复杂性肛瘘诊断准确率低, 须与其他方法联合应用. 瘘管X线造影无法明确瘘管与括约肌的关系, CT成像技术对区分瘘管组织与周围肌肉缺乏特异性, 二者现已很少应用. 核磁共振和三维肛管直肠腔内超声已逐渐成为肛瘘术前常规的检查方法, 对指导精准手术发挥了重要作用, 但二者也存在各自的缺点. 本文将对各种肛瘘术前评估方法作一综述.
核心提示: 肛瘘术前评估的传统方法包括查体、探针探查、Goodsall定律、亚甲蓝试验等, 其对复杂性肛瘘诊断准确率低, 须与其他方法联合应用. 瘘管X线造影无法明确瘘管与括约肌的关系, 电子计算机X射线断层扫描技术(computed tomography)对区分瘘管组织与周围肌肉缺乏特异性. 核磁共振和三维肛管直肠腔内超声已逐渐成为肛瘘术前常规的检查方法, 对指导精准手术发挥了重要作用, 但二者也存在各自的缺点.
引文著录: 王永刚, 丁健华, 赵克. 肛瘘术前评估方法的研究进展. 世界华人消化杂志 2014; 22(16): 2265-2270
Revised: April 5, 2014
Accepted: April 14, 2014
Published online: June 8, 2014
Anal fistula is one of the most common perianal diseases, and methods for its preoperative assessment are diverse. Traditional methods include physical examination, probing, Goodsall's law, methylene blue test, and so on. Although traditional methods play a role, their accuracy for complex anal fistulas is low. Therefore, their application must be combined with other methods. Fistulography fails to depict the relationship of the fistula to the sphincter complex, and computed tomography lacks specificity to distinguish between fistula and surrounding muscle tissue. Both methods are rarely used now. Magnetic resonance imaging and three-dimensional anorectal endosonography have become routine preoperative examinations and play an important role for guiding precise surgery. However, they also have their own shortcomings. In this paper, we will summarize a variety of methods for preoperative assessment of anal fistula.
- Citation: Wang YG, Ding JH, Zhao K. Methods for preoperative assessment of anal fistula. Shijie Huaren Xiaohua Zazhi 2014; 22(16): 2265-2270
- URL: https://www.wjgnet.com/1009-3079/full/v22/i16/2265.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v22.i16.2265
肛瘘是最常见的肛周疾病之一, 占肛周感染性疾病的70%, 其中90%为腺源性肛瘘[1]. 根据瘘管与括约肌复合体的解剖关系将肛瘘分为[2]: 括约肌间、经括约肌、括约肌外、括约肌上肛瘘,其治疗原则是破坏内口、去除瘘管并最大限度地保留肛门括约肌. 肛瘘切开范围过大可能导致术后大便失禁, 而不适当的保留肛门括约肌又会导致肛瘘复发. 文献报道肛瘘术后不同程度肛门失禁的发生率为0-40%, 术后复发率为0-26.5%[3,4]. 导致上述情况的主要原因是未能准确定位内口、瘘管处理不彻底或遗漏了分支瘘管、对瘘管走行不了解等[5]. 因此, 肛瘘术前准确找到内口、明确是否存在分支瘘管和瘘管走行与括约肌关系, 对降低术后复发率, 避免损伤括约肌、保护肛门功能至关重要. 近年对肛瘘术前评估方面取得了长足进展, 现综述如下.
传统方法包括查体、探针探查、Goodsall定律、亚甲蓝试验.
查体包括视诊和触诊, 是肛瘘术前的基本检查方法, 有经验的外科医生通过查体可以区分是复杂性肛瘘还是简单性肛瘘, 明确简单性肛瘘瘘管的走行和内口的位置, 但其对复杂性或复发性肛瘘的内口定位和瘘管走行的准确率低[6,7].
探针探查因可造成患者明显的疼痛不适, 主要应用于手术过程中或麻醉状态下, 对于直瘘和瘘管明确的肛瘘, 其具有较高的准确率, 而瘘管狭小或瘘管屈曲的肛瘘, 因探针无法通过,不能明确瘘管走形及定位内口. 另外, 探针探查过程中过度用力, 有可能造成"假瘘管"或"假内口", 导致术后复发. 指诊和探针探查曾被认为是肛瘘术前评估的金标准, 但其准确率低, 尤其对于严重瘢痕化和复杂性肛瘘缺乏特异性[8], 已经被许多专家所质疑.
根据肛瘘外口位置来判断内口的Goodsall定律被广泛应用于肛瘘的术前评估, 对于经后位的肛瘘其内口定位准确率为88.7%, 而对经前位肛瘘内口定位准确率较低, 尤其对于女性患者, 准确率为65.1%[9]. 而且, 肛瘘的直与弯, 除与位于肛管的前、后有关系外, 与肛瘘的高位及低位、外口距肛缘的远近都有一定关系. 因此, 单纯应用Goodsall定律对患者进行术前评估, 可能造成误导, 导致术后复发, 应结合其他检查综合评估提高术前诊断准确率.
通过外口向瘘管内注射亚甲蓝溶液, 在肛管内观察内口位置, 文献报道其内口定位准确率达83%, 但对于瘢痕化严重、瘘管过于屈曲狭长或伴有脓肿存在的肛瘘, 其应用受到局限[10]. 另外, 因亚甲蓝可造成瘘管周围组织蓝染, 而无法准确定位内口.
瘘管造影是应用最早的肛瘘成像技术, 通过瘘管内注射水溶性造影剂, 在X光下可清晰显示瘘管, 对于外口明确且外口距离肛缘较远的, 尤其对于活动期的慢性肛瘘具有较高的准确率, 但不能明确瘘管与括约肌复合体的解剖关系. 另外, 瘘管造影存在电离辐射, 还可能因加压注射造影剂使细菌、对比剂进入血流分别引起菌血症、对比剂不良反应. 研究显示, 瘘管造影诊断准确率<16%[11,12]. 随着多层螺旋CT、磁共振等技术应用于肛瘘术前评估, X线造影技术已逐渐被淘汰. 多层螺旋CT的应用明显提高了对肛瘘诊断的准确率, 术前对内口、支管评价的准确率分别为62.1%、89.3%, 多层螺旋CT后处理重建技术中, 曲面重建可清晰显示瘘管的具体位置及其与肛管内外括约肌、肛提肌的关系, 容量重建能三维再现瘘管的形态和走行特点[13]. 但因瘘管组织对CT成像的衰减作用与括约肌、脂肪层类似, 对区分纤维化的瘘管与括约肌复合体和盆底肌肉缺乏特异性[8,14].
磁共振成像(magnetic resonance imaging, MRI)因具有对软组织成像清晰、分辨率高、扫描范围广泛、多层面扫描等优点而广泛应用于肛瘘的术前评估, 对于复杂性肛瘘, 其作用更为显著[15]. 肛瘘MRI表现为: 于T2WI及脂肪抑制T2WI表现高信号, T1WI为条索状略低信号影, 增强扫描瘘管壁有明显强化, 内口表现为圆点状强化[16]. 瘢痕组织及术后纤维化在脂肪抑制T1WI、T2WI图像上均呈低信号, 且增强后无强化. T2WI能够区分活动期的瘘管与周围纤维化组织, 以及描述瘘管与括约肌的关系. 静脉内注射钆进行动态对比增强, 提高了瘘管的清晰度, 尤其是对T2WI不清晰的非活动期的肛瘘, T1WI具有更高的分辨能力[17]. 通过轴位、冠状位、矢状位等多方位扫描, 精确描述瘘管与括约肌复合体的关系及瘘管走向, 特别是复杂性肛瘘的数目、瘘管走行、支管形成及内口的位置和瘘管与周围肌肉的关系、有无脓肿形成, 文献报道诊断主瘘管的准确率达88%-100%, 诊断分支瘘管的准确率达91%, 马蹄形肛瘘诊断准确率达100%, 内口定位准确率达96%[18], 而腔内MRI成像技术对主瘘管诊断的准确率达93%[19]. 国外许多文献也证实了MRI在肛瘘术前评估中的作用[20-24]. 近年, 国内也对MRI在肛瘘评估中的作用进行了报道[25]. 术前应用磁共振检查还可以降低术后复发率[21,26]. 体外相控阵线圈具有更高的分辨率, 并且避免了腔内线圈对患者所引起的不适. 包括脂肪抑制和对比增强在内的多平面、多序列扫描技术的应用改善了磁共振对肛瘘的诊断, 三维磁共振的应用进一步提高了对肛瘘诊断的准确率[27,28]. 术前行MRI检查已逐渐成为术前肛瘘诊断的金标准[29]. 但其检查费用高, 操作耗费时间相对较长, 限制了这一技术的普及和应用.
二维肛管直肠腔内超声于20年前由泌尿外科医生首次应用于临床, 因其具有简单易学、费用低、不会引起患者过多不适等优点, 被用于直肠、肛管肿瘤的分期和对肛门括约肌、盆底良性病变的评估. 其能够清晰显示瘘管走形、内口位置, 通过外口注射过氧化氢, 使瘘管呈现高回声, 明显提高对肛瘘诊断的准确率. 研究发现其诊断瘘管类型的准确率达63%-94%[30,31], 内口定位的准确率达93%[30]. 过氧化氢增强后主瘘管诊断准确率为95%[32]. 但二维肛管直肠腔内超声也有缺点: (1)内口紧贴探头表面, 受外力挤压使内口呈假性闭合状态, 影响诊断; (2)因水肿的存在使内口回声界面复杂, 呈现与内膜相似的高回声而难以判断; (3)二维图像不能轴向显示瘘管的长度及其分支的走行全貌[33]. 近年, 也有经会阴超声检查评估肛瘘的报道, 瘘管类型判断准确率为85.2%, 内口定位准确率为72.3%. 对于复杂性肛瘘、肛管畸形和怀疑有直肠阴道瘘的患者具有独特优势[34].
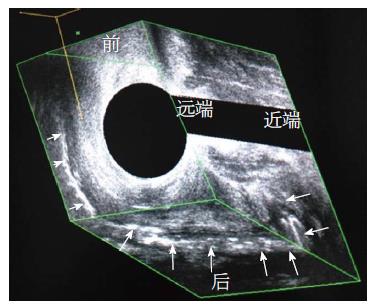
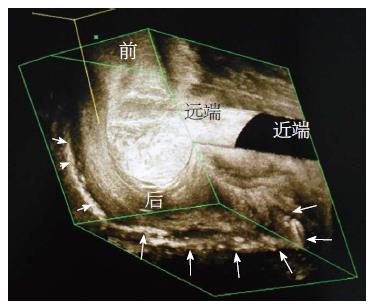
采用360度旋转的6-16 MHz高频探头, 通过软件三维重建形成立体图像, 精确地测量角度、距离、范围及容量,通过各个角度对三维图像进行旋转、倾斜、剪切, 从而获得定性和定量信息[35], 可同时从矢状面、冠状面、横断面观察肛管、直肠结构, 比二维肛管直肠腔内超声提供更加精确的信息, 进一步提高了内口及瘘管诊断的准确率[36-39]. 三维肛管直肠腔内超声能够很好地显示瘘管的走行全貌、与括约肌复合体的关系及手术可能涉及的括约肌范围[35,40]. 肛瘘内口可以为低回声型, 也可以为高回声型. 内口位置的超声诊断标准为: (1)由括约肌间瘘管形成的出芽形表现, 且与肛门内括约肌相连; (2)内括约肌缺如的出芽形表现; (3)通过内括约肌缺如部位, 连于括约肌间瘘管的皮下组织破坏的表现. 操作过程中通过外口向瘘管内注入过氧化氢产生气泡, 使瘘管走行从低回声变为高回声(图1), 可提高对肛瘘类型诊断的正确率[41,42], 通过向量渲染使瘘管显影更加清晰(图2), 同时具有实时直观等优势. 文献报道, 三维肛管直肠腔内超声所见和术中探查情况符合率达85.8%[43]. 目前, 国内也有文献报道了其在肛瘘术前评估中的重要作用[44-46]. 另外, 三维肛管直肠腔内超声还可以辨识克罗恩病合并的肛瘘是肛腺感染所致还是克罗恩病所致[47-49]. 对于克罗恩病所致肛瘘, 在超声直视下对瘘管和脓腔进行冲洗, 对预后取得了良好的效果[50]. 同时, 其操作方便灵活, 可在床旁、门诊、手术室随时检查, 检查过程中过氧化氢增强可实时动态显示内口及瘘管走行, 检查时间短、费用低、设备不昂贵便于普及. 因此, 越来越多的专家将三维肛管直肠腔内超声作为肛瘘术前标准的诊断性检查方法, 明显地提高了治愈率, 降低了术后大便失禁率.
许多研究比较了肛管直肠腔内超声与MRI评估肛瘘的准确性, 结果显示两者在发现主瘘管、分支瘘管、内口等方面的敏感性相当[8,51,52], 三维增强肛管直肠腔内超声和磁共振成像对主瘘管(81% vs 90%)、分支瘘管(67% vs 57%)、内口定位(86% vs 86%)均有较高的准确率[53]. 肛管直肠腔内超声对于肛提肌上及坐骨直肠窝脓肿特异性较低, 而磁共振成像技术因具有扫描范围广泛和多层次扫描等优点填补了肛管直肠腔内超声这一缺陷. 但三维肛管直肠腔内超声实时直观, 可三维展现瘘管走形全貌, 精确测量瘘管长度和累及括约肌长度, 对精准手术具有指导作用, 研究显示, 若二者联合应用将诊断准确率提升到100%[54].
总之, 肛瘘术前检查明确内口位置、瘘管走行及是否存在分支瘘管, 尤其是复杂性肛瘘, 对降低术后复发率和大便失禁率至关重要, 而现有的的术前检查方法各有利弊. MRI和肛管直肠腔内超声是目前主要的检查方法, 二者对肛瘘术前评估均具有较高的准确率, 且各有优缺点, 因此应根据具体情况优化选择合适的术前评估方法.
肛瘘占肛周感染性疾病的70%, 手术常比较困难, 是引起医患纠纷的常见病种之一. 主要是因为肛瘘术后容易复发和发生不同程度肛门失禁. 导致上述情况的主要原因是内口定位不准确、瘘管处理不彻底或遗漏了瘘管分支、对瘘管走行不了解等, 目前术前评估方法多种多样, 各有其优缺点.
朱亮, 副教授, 大连医科大学
MRI和肛管直肠腔内超声是目前主要的检查方法, 二者对肛瘘术前评估均具有较高的准确率, 本文重点介绍了二者的优缺点.
简明扼要并且全面地介绍各种肛瘘术前评估方法.
指导临床医生选择合适的术前评估方法, 制定合适的手术方案.
全面概括了目前所有肛瘘术前评估方法, 总体评价较好.
编辑: 郭鹏 电编:鲁亚静
| 2. | Parks AG, Gordon PH, Hardcastle JD. A classification of fistula-in-ano. Br J Surg. 1976;63:1-12. [PubMed] |
| 3. | Rosa G, Lolli P, Piccinelli D, Mazzola F, Bonomo S. Fistula in ano: anatomoclinical aspects, surgical therapy and results in 844 patients. Tech Coloproctol. 2006;10:215-221. [PubMed] [DOI] |
| 4. | Sudoł-Szopińska I, Kołodziejczak M, Szopiński TR. The accuracy of a postprocessing technique--volume render mode--in three-dimensional endoanal ultrasonography of anal abscesses and fistulas. Dis Colon Rectum. 2011;54:238-244. [PubMed] [DOI] |
| 6. | Lindsey I, Humphreys MM, George BD, Mortensen NJ. The role of anal ultrasound in the management of anal fistulas. Colorectal Dis. 2002;4:118-122. [PubMed] |
| 7. | Buchanan GN, Halligan S, Bartram CI, Williams AB, Tarroni D, Cohen CR. Clinical examination, endosonography, and MR imaging in preoperative assessment of fistula in ano: comparison with outcome-based reference standard. Radiology. 2004;233:674-681. [PubMed] [DOI] |
| 8. | Herbst F. Pelvic radiological imaging: a surgeon's perspective. Eur J Radiol. 2003;47:135-141. [PubMed] |
| 9. | Coremans G, Dockx S, Wyndaele J, Hendrickx A. Do anal fistulas in Crohn's disease behave differently and defy Goodsall's rule more frequently than fistulas that are cryptoglandular in origin? Am J Gastroenterol. 2003;98:2732-2735. [PubMed] [DOI] |
| 10. | Gonzalez-Ruiz C, Kaiser AM, Vukasin P, Beart RW, Ortega AE. Intraoperative physical diagnosis in the management of anal fistula. Am Surg. 2006;72:11-15. [PubMed] |
| 11. | Himes N, Min JY, Lee R, Brown C, Shea J, Huang X, Xiao YF, Morgan JP, Burstein D, Oettgen P. In vivo MRI of embryonic stem cells in a mouse model of myocardial infarction. Magn Reson Med. 2004;52:1214-1219. [PubMed] |
| 12. | Morris J, Spencer JA, Ambrose NS. MR imaging classification of perianal fistulas and its implications for patient management. Radiographics. 2000;20:623-35; discussion 635-7. [PubMed] [DOI] |
| 14. | Dwarkasing S, Hussain SM, Krestin GP. Magnetic resonance imaging of perianal fistulas. Semin Ultrasound CT MR. 2005;26:247-258. [PubMed] |
| 15. | Joyce M, Veniero JC, Kiran RP. Magnetic resonance imaging in the management of anal fistula and anorectal sepsis. Clin Colon Rectal Surg. 2008;21:213-219. [PubMed] [DOI] |
| 16. | Al-Khawari HA, Gupta R, Sinan TS, Prakash B, Al-Amer A, Al-Bolushi S. Role of magnetic resonance imaging in the assessment of perianal fistulas. Med Princ Pract. 2005;14:46-52. [PubMed] [DOI] |
| 17. | Schaefer O, Lohrmann C, Kreisel W, Rasenack J, Ruf G, Hopt U, Langer M. Differentiation of perianal fistulas with digital subtraction magnetic resonance fistulography. Inflamm Bowel Dis. 2005;11:383-387. [PubMed] |
| 18. | Beets-Tan RG, Beets GL, van der Hoop AG, Kessels AG, Vliegen RF, Baeten CG, van Engelshoven JM. Preoperative MR imaging of anal fistulas: Does it really help the surgeon? Radiology. 2001;218:75-84. [PubMed] [DOI] |
| 19. | Hussain SM, Stoker J, Schouten WR, Hop WC, Laméris JS. Fistula in ano: endoanal sonography versus endoanal MR imaging in classification. Radiology. 1996;200:475-481. [PubMed] [DOI] |
| 20. | Mullen R, Deveraj S, Suttie SA, Matthews AG, Yalamarthi S. MR imaging of fistula in ano: indications and contribution to surgical assessment. Acta Chir Belg. 2001;111:393-397. [PubMed] |
| 21. | George U, Sahota A, Rathore S. MRI in evaluation of perianal fistula. J Med Imaging Radiat Oncol. 2011;55:391-400. [PubMed] [DOI] |
| 22. | Yildirim N, Gökalp G, Öztürk E, Zorluoğlu A, Yilmazlar T, Ercan I, Savci G. Ideal combination of MRI sequences for perianal fistula classification and the evaluation of additional findings for readers with varying levels of experience. Diagn Interv Radiol. 2012;18:11-19. [PubMed] [DOI] |
| 23. | de Miguel Criado J, del Salto LG, Rivas PF, del Hoyo LF, Velasco LG, de las Vacas MI, Marco Sanz AG, Paradela MM, Moreno EF. MR imaging evaluation of perianal fistulas: spectrum of imaging features. Radiographics. 2012;32:175-194. [PubMed] [DOI] |
| 24. | Waniczek D, Adamczyk T, Arendt J, Kluczewska E, Kozińska-Marek E. Usefulness assessment of preoperative MRI fistulography in patients with perianal fistulas. Pol J Radiol. 2011;76:40-44. [PubMed] |
| 26. | O'Malley RB, Al-Hawary MM, Kaza RK, Wasnik AP, Liu PS, Hussain HK. Rectal imaging: part 2, Perianal fistula evaluation on pelvic MRI--what the radiologist needs to know. AJR Am J Roentgenol. 2012;199:W43-W53. [PubMed] [DOI] |
| 27. | Rofsky NM, Lee VS, Laub G, Pollack MA, Krinsky GA, Thomasson D, Ambrosino MM, Weinreb JC. Abdominal MR imaging with a volumetric interpolated breath-hold examination. Radiology. 1999;212:876-884. [PubMed] [DOI] |
| 29. | Mónica AN, Costa A, Aleluia C. [MRI evaluation of fistula in ano]. Acta Med Port. 2007;20:319-324. [PubMed] |
| 30. | Lengyel AJ, Hurst NG, Williams JG. Pre-operative assessment of anal fistulas using endoanal ultrasound. Colorectal Dis. 2002;4:436-440. [PubMed] |
| 31. | Santoro GA, Fortling B. The advantages of volume rendering in three-dimensional endosonography of the anorectum. Dis Colon Rectum. 2007;50:359-368. [PubMed] [DOI] |
| 32. | Cho DY. Endosonographic criteria for an internal opening of fistula-in-ano. Dis Colon Rectum. 1999;42:515-518. [PubMed] |
| 34. | Nevler A, Beer-Gabel M, Lebedyev A, Soffer A, Gutman M, Carter D, Zbar AP. Transperineal ultrasonography in perianal Crohn's disease and recurrent cryptogenic fistula-in-ano. Colorectal Dis. 2013;15:1011-1018. [PubMed] [DOI] |
| 35. | Garcés-Albir M, García-Botello SA, Esclapez-Valero P, Sanahuja-Santafé A, Raga-Vázquez J, Espi-Macías A, Ortega-Serrano J. Quantifying the extent of fistulotomy. How much sphincter can we safely divide? A three-dimensional endosonographic study. Int J Colorectal Dis. 2012;27:1109-1116. [PubMed] [DOI] |
| 36. | Garcés Albir M, García Botello S, Esclápez Valero P, Sanahuja Santafé A, Espí Macías A, Flor Lorente B, García-Granero E. [Evaluation of three-dimensional endoanal endosonography of perianal fistulas and correlation with surgical findings]. Cir Esp. 2010;87:299-305. [PubMed] [DOI] |
| 37. | Subasinghe D, Samarasekera DN. Comparison of preoperative endoanal ultrasonography with intraoperative findings for fistula in ano. World J Surg. 2010;34:1123-1127. [PubMed] [DOI] |
| 38. | Murad-Regadas SM, Regadas FS, Rodrigues LV, Holanda Ede C, Barreto RG, Oliveira L. The role of 3-dimensional anorectal ultrasonography in the assessment of anterior transsphincteric fistula. Dis Colon Rectum. 2010;53:1035-1040. [PubMed] [DOI] |
| 39. | Gravante G, Giordano P. The role of three-dimensional endoluminal ultrasound imaging in the evaluation of anorectal diseases: a review. Surg Endosc. 2008;22:1570-1578. [PubMed] [DOI] |
| 40. | Murad-Regadas SM, Regadas FS, Rodrigues LV, Fernandes GO, Buchen G, Kenmoti VT, Soares Gdos S, Holanda Ede C. Anatomic characteristics of anal fistula on three-dimensional anorectal ultrasonography. Dis Colon Rectum. 2011;54:460-466. [PubMed] [DOI] |
| 41. | Poen AC, Felt-Bersma RJ, Eijsbouts QA, Cuesta MA, Meuwissen SG. Hydrogen peroxide-enhanced transanal ultrasound in the assessment of fistula-in-ano. Dis Colon Rectum. 1998;41:1147-1152. [PubMed] |
| 42. | Kim Y, Park YJ. Three-dimensional endoanal ultrasonographic assessment of an anal fistula with and without H(2)O(2) enhancement. World J Gastroenterol. 2009;15:4810-4815. [PubMed] |
| 43. | Jeon HJ, Park UC, Park HS, Kim YJ, Jung SI, Park SW. Clinical usefulness of endoanal ultrasound in patients with complex anal fistula. ULTRASOUND MED BIOL. 2011;37:S14-S14. [DOI] |
| 44. | 项 晓宇, 程 遵华, 童 仙君. 经直肠超声在肛瘘诊断中的应用价值. 中华医学超声杂志(电子版). 2011;8:1064-1069. |
| 47. | Blom J, Nyström PO, Gunnarsson U, Strigård K. Endoanal ultrasonography may distinguish Crohn's anal fistulae from cryptoglandular fistulae in patients with Crohn's disease: a cross-sectional study. Tech Coloproctol. 2011;15:327-330. [PubMed] [DOI] |
| 48. | Zawadzki A, Starck M, Bohe M, Thorlacius H. A unique 3D endoanal ultrasound feature of perianal Crohn's fistula: the 'Crohn ultrasound fistula sign'. Colorectal Dis. 2012;14:e608-e611. [PubMed] [DOI] |
| 49. | Viganò C, Losco A, Caprioli F, Basilisco G. Incidence and clinical outcomes of intersphincteric abscesses diagnosed by anal ultrasonography in patients with crohn's disease. Inflamm Bowel Dis. 2011;17:2102-2108. [PubMed] [DOI] |
| 50. | Vitton V, Gascou G, Ezzedine SS, Gasmi M, Grimaud JC, Barthet M. Endoanal ultrasonography-assisted percutaneous transperineal management of anorectal sepsis. Surg Laparosc Endosc Percutan Tech. 2012;22:148-153. [PubMed] [DOI] |
| 51. | Siddiqui MR, Ashrafian H, Tozer P, Daulatzai N, Burling D, Hart A, Athanasiou T, Phillips RK. A diagnostic accuracy meta-analysis of endoanal ultrasound and MRI for perianal fistula assessment. Dis Colon Rectum. 2012;55:576-585. [PubMed] [DOI] |
| 52. | Navarro-Luna A, García-Domingo MI, Rius-Macías J, Marco-Molina C. Ultrasound study of anal fistulas with hydrogen peroxide enhancement. Dis Colon Rectum. 2004;47:108-114. [PubMed] [DOI] |
| 53. | West RL, Dwarkasing S, Felt-Bersma RJ, Schouten WR, Hop WC, Hussain SM, Kuipers EJ. Hydrogen peroxide-enhanced three-dimensional endoanal ultrasonography and endoanal magnetic resonance imaging in evaluating perianal fistulas: agreement and patient preference. Eur J Gastroenterol Hepatol. 2004;16:1319-1324. [PubMed] |
| 54. | Schwartz DA, Wiersema MJ, Dudiak KM, Fletcher JG, Clain JE, Tremaine WJ, Zinsmeister AR, Norton ID, Boardman LA, Devine RM. A comparison of endoscopic ultrasound, magnetic resonance imaging, and exam under anesthesia for evaluation of Crohn's perianal fistulas. Gastroenterology. 2001;121:1064-1072. [PubMed] |