修回日期: 2008-01-14
接受日期: 2008-01-21
在线出版日期: 2008-02-18
目的: 评价腹膜活检在结核性腹膜炎诊断中的临床实用性.
方法: 152例腹水原因待查患者, 采用超声穿刺探头引导下经皮于增厚的腹膜处进行活检, 活检组织行病理学检查, 所有患者均进行PPD、血沉、血清C反应蛋白(CRP)和腹水乳酸脱氢酶(LDH)、腹部X线检查.
结果: 腹膜活检的成功率为96.05%, 结核性腹膜炎64例, 占腹膜活检者的42.11%. 152例腹膜活检患者中, 诊断为结核性腹膜炎者64例, 占总不明原因腹水42.11%, 腹膜活检阳性率明显高于目前用于临床提示结核性腹膜炎的一般性辅助检查包括血沉增快(χ2 = 1.265, P = 0.261)、PPD阳性(χ2 = 26.669, P = 0.000)、CRP升高(χ2 = 8.125, P = 0.004), 腹水LDH增高(χ2 = 20.403, P = 0.000)、腹部X线检查阳性所见(χ2 = 7.169, P = 0.007), 统计处理差异显著. 腹膜活检病理组织内可见结核的病理改变: 干酪样坏死, 朗罕氏细胞、类上皮细胞及多核巨细胞, 组织内有大量纤维脂肪组织.
结论: 经皮腹膜穿刺活检可以确诊结核性腹膜炎, 安全可靠, 使用限制少, 是一种最具有临床实用价值的检查手段.
引文著录: 刘东屏, 贺庆娟, 王学梅, 孙明军. 经皮超声引导下腹膜穿刺活检诊断结核性腹膜炎的临床实用性分析. 世界华人消化杂志 2008; 16(5): 567-569
Revised: January 14, 2008
Accepted: January 21, 2008
Published online: February 18, 2008
AIM: To evaluate the clinical practical value of epiploon biopsy in the diagnosis of tuberculous peritonitis.
METHODS: A total of 152 ascetic patients with uncertain diagnosis were selected to puncture the thickened peritoneum under the guidance of ultrasonic puncture probe. Biopsy tissue was sent for pathological examination. Serum PPD, ESR and CRP were and LDH in ascites were detected. Abdomen was examined by X-rays.
RESULTS: The success rate of epiploon biopsy was 96.05%. Of the 152 patients, 64 were diagnosed as tuberculous peritonitis, accounting for 42.11% of ascetic patients with uncertain diagnosis. The positive rate of epiploon biopsy was obviously higher than that of traditional clinical examinations. Serum ESR (χ2 = 1.265, P = 0.261), PPD (χ2 = 26.669, P = 0.000), CRP (χ2 = 8.125, P = 0.004) and LDH in ascites (χ2 = 20.403, P = 0.000) and positive findings of abdominal X-ray findings (χ2 = 7.169, P = 0.007) were increased in tuberculous peritonitis patients with a significantly statistical difference (P < 0.05). Following pathologic findings of TB were observed in peritoneal tissue samples: cheese necrosis, Langhan's cells-like and epithelial cells-like multinucleated giant cells, a large number of fibers within adipose tissue.
CONCLUSION: Percutaneous biopsy can be confirmed tuberculosis peritonitis, secure, reliable, less restriction on the use, is one of the most practical clinical means of inspection.
- Citation: Liu DP, He QJ, Wang XM, Sun MJ. Clinical outcome analysis of epiploon biopsy in the diagnosis of patients with tuberculous peritonitis. Shijie Huaren Xiaohua Zazhi 2008; 16(5): 567-569
- URL: https://www.wjgnet.com/1009-3079/full/v16/i5/567.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v16.i5.567
结核性腹膜炎起病隐匿, 临床缺乏特异性表现及特异性检查指标, 极易和恶性腹水相混淆, 二者的鉴别一直是临床医生面临的一大难题, 尽管临床影像、腹水细胞学检测和内镜等检查可以使一些腹水的病因得到明确, 但仍有相当一部分病例腹水原因不明. 结核性腹膜炎的治疗、预后和恶性腹水截然不同, 因此两者的鉴别极为重要. 腹膜穿刺活检是近年来国内外开展的一种用于诊断原因不明的腹水的一种特殊手段[1-3]. 我们总结了近5年来我院开展的152例经皮超声引导下腹膜穿刺活检病例, 分析比较了腹膜活检在结核性腹膜炎诊断中的临床实用性.
152例腹水原因待查患者, 男性82例, 女性70例, 年龄在22-68岁, 平均44.5岁, 为2001-01/2006-03我院住院患者, 经B超检查均有不同程度不同部位的腹膜增厚, 腹膜厚度在1.2-3.5 cm, 平均厚度在1.68 cm.
检查前所有患者均测定出凝血时间、血小板计数、凝血酶原时间, 腹膜活检采用在超声穿刺探头引导下于增厚的腹膜处进行活检, 穿刺针规格为14-18 G, 采用半自动活检枪, 嘱患者短暂屏气, 触发活检枪瞬间活检, 每例活检1-3次, 活检组织置于950 mL/L乙醇中固定送检, 术中按压伤口10 min, 组织石蜡包埋, HE染色后作病理学诊断. 血沉正常范围: 男性0-15/1 h末, 女性0-20/1 h末. PPD判断标准: 硬结平均直径如小于5 mm为阴性, 大于等于5 mm小于20 mm为阳性反应, 其中5-9 mm为弱阳性(+), 10-19 mm为阳性(++), 20 mm以上或局部有水疱、坏死、淋巴管炎均为强阳性(+++). 血清CRP浓度测定采用免疫散射速率比浊法, 正常范围是0-0.8 mg/dL, 用美国BECKMAN公司IMMAGE全自动免疫分析仪测定, 试剂购自美国BECKMAN公司, 腹水LDH检测为酶学速率法, 正常值为82-268 U/L, 用日立7600自动生化分析仪, 试剂购于日本第一化学株式会社, 腹部X线阳性所见为腹部有结核钙化灶.
统计学处理 统计学处理采用统计分析软件SPSS11.5, 对资料行χ2检验. P<0.05差异显著.
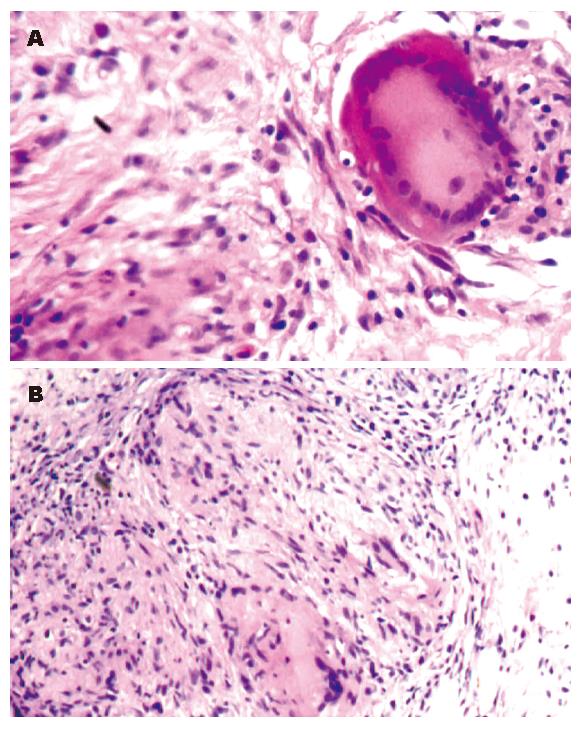
152例腹膜活检病例中, 有6例病理回报为平滑肌组织和无成分组织, 腹膜活检的成功率为96.05%, 结核性腹膜炎64例, 占腹膜活检者的42.11%. 152例腹膜活检的患者中, 有57例在活检后24 h内, 有轻微可以忍受的疼痛, 未予处置自行缓解, 无出血, 无脏器穿孔等并发症. 64例结核性腹膜炎患者的临床辅助检查与腹膜活检阳性率比较(表1). 结核性腹膜炎腹膜活检病理改变见图1.
| 项目 | 总体阳性率 | 结腹阳性率 | χ2 | P |
| 血沉增快 | 88.82(135/152) | 92.19(59/64) | 1.265 | 0.261 |
| PPD≥(++) | 38.82(59/152) | 64.06(41/64) | 26.669 | 0.000 |
| 腹部X线阳性所见 | 17.76(27/152) | 28.13(18/64) | 8.125 | 0.004 |
| 腹水LDH增高 | 51.98(79/152) | 73.44(47/64) | 20.403 | 0.000 |
| 血CRP增高 | 35.53(54/152) | 54.69(35/64) | 7.169 | 0.007 |
结核性腹膜炎是临床一种常见病, 结核性腹膜炎的腹水常规和生化学检测无诊断意义[1-4], 以往诊断上缺乏病理学的确切依据, 临床上仅靠试验性抗结核治疗来证实结核性腹膜炎的诊断[5], 随着结核耐药菌的增多, 试验性抗结核治疗疗效不显著, 同时抗结核药物对肝肾功能的损伤, 使试验性抗结核治疗的实际应用受到限制. 自从腹腔镜开展以来, 结核性腹膜炎可以靠此手段确诊[6-7], 但需要全身麻醉, 费用较高. 腹膜活检是近年用于诊断和鉴别结核性腹膜炎腹水和恶性腹水的一种临床检查方法[8-11]. 本研究结果显示腹膜活检的阳性率是96.05%(146/152), 结核性腹膜炎占活检总数的43.84%, 同步进行的临床常用的辅助检查, 任何单项检测血沉增快、血CRP增高、腹水LDH增高、PPD阳性、腹部X线阳性所见对临床诊断的实用价值都明显低于腹膜穿刺活检, 我们所采用的全自动组织切割腹膜活检, 使腹膜活检瞬间完成, 不易造成腹腔内器官的损伤和腹膜出血, 安全可靠, 使用限制小[12-14]. 活检病理可直接给出诊断金标准-病理诊断, 腹膜穿刺活检的病理可以见到典型的结核病理改变: 干酪样坏死、朗罕氏巨细胞、类上皮细胞和大量纤维脂肪细胞. 对于原因不明的腹水当临床疑诊结核性腹膜炎时, 尽管腹膜穿刺活检为有创性检查, 但鉴于结核性腹膜炎目前缺乏临床确诊的手段, 而腹膜穿刺活检可以达到确诊结核性腹膜炎的目的, 且无明显并发症[15], 故在有条件的医院, 经皮腹膜穿刺活检是一种确诊结核性腹膜炎最有临床实用价值的检查手段.
结核性腹膜炎是临床的常见疾病, 临床上常靠试验性抗结核治疗诊断, 常和恶性腹水相混淆, 容易误诊, 近年来开展的超声引导下经腹壁穿刺腹膜活检, 可以达到确诊结核性腹膜炎的目的.
唐晓鹏, 教授, 中南大学肝病研究所, 中南大学湘雅二医院感染科
鉴于结核性腹膜炎目前缺乏临床确诊的手段, 腹膜穿刺活检可以达到确诊结核性腹膜炎的目的, 故经皮腹膜穿刺活检是目前最有临床实用价值的检查手段.
本文表述较清晰, 文笔较流畅, 立题有一定新颖性, 设计合理, 研究内容立足临床, 实用性较强, 有较好的学术价值.
编辑: 程剑侠 电编: 郭海丽
| 1. | Chow KM, Chow VC, Szeto CC. Indication for peritoneal biopsy in tuberculous peritonitis. Am J Surg. 2003;185:567-573. [PubMed] [DOI] |
| 2. | Barutcu O, Erel HE, Saygili E, Yildirim T, Torun D. Abdominopelvic tuberculosis simulating disseminated ovarian carcinoma with elevated CA-125 level: report of two cases. Abdom Imaging. 2002;27:465-470. [PubMed] [DOI] |
| 3. | Hiller N, Lioubashevsky N. Tuberculous peritonitis: a diagnostic challenge. Abdom Imaging. 2001;26:319-322. [PubMed] [DOI] |
| 4. | Li CP, Huang TS, Chao Y, Chang FY, Whang-Peng J, Lee SD. Advantages of assaying telomerase activity in ascites for diagnosis of digestive tract malignancies. World J Gastroenterol. 2004;10:2468-2471. [PubMed] [DOI] |
| 7. | Rai S, Thomas WM. Diagnosis of abdominal tuberculosis: the importance of laparoscopy. J R Soc Med. 2003;96:586-588. [PubMed] [DOI] |
| 8. | Sun XM, Dong WG, Yu BP, Luo HS, Yu JP. Detection of type IV collagenase activity in malignant ascites. World J Gastroenterol. 2003;9:2592-2595. [PubMed] |
| 9. | Ho LM, Thomas J, Fine SA, Paulson EK. Usefulness of sonographic guidance during percutaneous biopsy of mesenteric masses. AJR Am J Roentgenol. 2003;180:1563-1566. [PubMed] [DOI] |
| 14. | Caspi B, Wolach V, von der Walde J, Weiss Y, Appelman Z, Hagay Z. Diagnosis of abdominal tuberculosis by transabdominal ultrasound-guided needle biopsy. Ultrasound Obstet Gynecol. 2000;16:569-570. [PubMed] [DOI] |
| 15. | Vardareli E, Kebapci M, Saricam T, Pasaoglu O, Açikalin M. Tuberculous peritonitis of the wet ascitic type: clinical features and diagnostic value of image-guided peritoneal biopsy. Dig Liver Dis. 2004;36:199-204. [PubMed] [DOI] |