修回日期: 2005-11-15
接受日期: 2005-11-26
在线出版日期: 2005-12-15
目的: 探讨载脂蛋白B(Apo B)基因Xba I位点多态性和血脂水平与慢性丙型肝炎之间的关系.
方法: 通过病例对照研究设计, 采用聚合酶链式反应-限制性片段长度多态性技术(PCR-RFLP)技术观察77例慢性丙型肝炎患者和62例健康对照者的Apo B基因Xba I位点的多态性, 采用全自动生化分析仪进行肝功、血脂水平的分析比较.
结果: 慢性丙型肝炎组和对照组Apo B基因Xba I位点X+X-, X-X-基因型构成不等, 慢性丙型肝炎组X+等位基因频率低于对照组(0.071 vs 0.121, P = 0.136), 且病例组中肝硬化组X+等位基因频率低于慢性肝炎组, 但未显示统计学的显著差异. 病例组中不同病毒载量组间Apo B基因Xba I位点基因型分布存在显著差异, HCV RNA≥80 000 copies/L组X+等位基因频率低于HCV RNA<80 000 copies/L组(0.048 vs 0.179, P = 0.035). 病例组中X+X-基因型的血清胆固醇 (CHO)水平、低密度脂蛋白(LDL)水平及Apo B水平均高于X-X-组, 而且Apo B水平的差异具统计学显著性 (P = 0.019); 血清高密度脂蛋白(HDL)水平低于X-X-组, 但无统计学差异. 慢性丙型肝炎患者血清Apo B水平和LDL水平与血清HCV RNA水平之间均呈直线负相关关系 (分别为r = -0.538, P = 0.005; r = -0.460, P = 0.016), 但与谷丙转氨酶(ALT)水平无相关性.
结论: Apo B基因Xba I位点的多态性与我国人群对HCV的易感性没有直接联系, 但与慢性丙型肝炎患者的病毒载量有关. X+等位基因频率可影响慢性丙型肝炎患者Apo B水平. 慢性丙型肝炎患者血清LDL水平和Apo B水平与血清HCV RNA水平显著相关.
引文著录: 李雁, 刘正稳, 韩群英, 李晗. 载脂蛋白B基因多态性及血脂水平与慢性丙型肝炎的相关性. 世界华人消化杂志 2005; 13(23): 2736-2741
Revised: November 15, 2005
Accepted: November 26, 2005
Published online: December 15, 2005
AIM: To investigate the Xba I locus polymorphisms of apolipoprotein B (Apo B) gene and their internal correlations with chronic hepatitis C virus infection and serum lipid metabolism.
METHODS: Polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) technique was used to analyze the genotype of the Apo B gene in 77 patients and 62 controls, according to the design of case control study. Meanwhile, the blood samples were analyzed for hepatic function and serum lipid by automatic biochemistry analyzer.
RESULTS: The frequencies of X+X- and X-X- of Xba I locus polymorphism were different between the patients and the controls and the frequency of X+ allele in the patients was lower than that in the controls (0.071 vs 0.121, P = 0.136), but no statistical significance was not found. The frequency of X+ allele in patients with HCV RNA≥80 000 copies/L was significantly lower than that with HCV RNA<80 000 copies/L (0.048 vs 0.179, P = 0.035). Furthermore, the levels of Apo B in the patients of X+X- genotype were significantly higher than those in the patients of X-X- genotype (P = 0.019). The serum levels of low density lipoprotein (LDL) and Apo B were negatively correlated with serum HCV RNA levels in patients with chronic hepatitis C (r = -0.460, P = 0.016; r = -0.538, P = 0.005, respectively), and the correlation with serum alanine aminotransferase (ALT) levels was not found.
CONCLUSION: The Xba I locus polymorphism of Apo B gene is not correlated with susceptibility of Chinese people to HCV, but it may affect the HCV viral load in patients with chronic hepatitis C. The variation of X+ allele may affect serum Apo B levels in patients with chronic HCV infection. The serum levels of LDL and Apo B are closely correlated with serum HCV RNA levels in patients with chronic hepatitis C.
- Citation: Li Y, Liu ZW, Han QY, Li H. Correlations of chronic hepatitis C virus infection with Xba I polymorphism of apolipoprotein B gene and serum lipid metabolism. Shijie Huaren Xiaohua Zazhi 2005; 13(23): 2736-2741
- URL: https://www.wjgnet.com/1009-3079/full/v13/i23/2736.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v13.i23.2736
丙型肝炎是丙型肝炎病毒 (HCV) 引起的一种常见传染病. 我国目前一般人群的感染率达3.2%, 是丙型肝炎的高流行区[1]. HCV感染不仅可引起急、慢性肝炎, 而且与肝纤维化和肝细胞癌的发生及发展密切相关[2], 严重危害人民的生命健康. 近年来发现HCV感染与脂蛋白转运系统有密切的联系[3,5,10,12].大量研究证实低密度脂蛋白受体(LDL-R)可能是HCV感染靶细胞的重要受体分子[11-14]. 载脂蛋白B 既是低密度脂蛋白(LDL)的主要载脂蛋白又是细胞表面LDL-R的配体, 因此在HCV感染肝细胞的过程中扮演着重要的角色[4,6,17,18]. 单采浆血浆分离置换法被认为是安全清除载脂蛋白B的一种快速而有效的方法, 国外一些研究[19-21]发现, 此法能有效降低HCV患者体内的病毒负荷. 目前, 载脂蛋白B基因结构已充分阐明, 研究证实其具有多个多态性位点, 有些位点的多态性与血脂变化及LDL受体结合相关, Xba I位点就是其中具代表性的一个[22-24], 一些研究证实其与冠心病、胆结石病的易感性有关[27-30], 但其与慢性丙型肝炎的关系尚未见报道. 我们采用病例对照研究设计, 应用聚合酶链式反应(PCR)和限制性片段长度多态性(RFLP)技术, 探索载脂蛋白B基因Xba I位点多态性及血脂成分与慢性丙型肝炎之间的关系.
慢性丙型肝炎患者77例, 来自2002-10/2004-04在西安交通大学第一医院就诊的患者, 其中男性46例, 女性31例, 平均年龄43.6±14.1岁. 所有患者均排除合并有肾功能损害者以及合并其他慢性肝脏疾病(甲型、乙型、戊型病毒性肝炎, 药物性肝炎, 酒精性肝炎, 自身免疫性肝炎, Wilson's病)和可引起脂代谢性紊乱的其他疾病(包括糖尿病, 获得性免疫缺陷综合征及甲状腺功能亢进). 按照2000年病毒性肝炎防治方案的临床分类和诊断标准, 慢性丙型肝炎65例, HCV相关肝硬化12例. 健康对照者62例, 来自西安市健康献血员及本院健康工作人员其中男性37例, 女性25例, 平均年龄40.0±9.8岁.
研究对象均为中国汉族人, 且均为随机选择, 无血缘关系. 经统计学分析, 病例组与对照组性别、年龄均无显著性差异.
1.2.1 基因组DNA抽提: 采用美国Geture公司生产、深圳晶美试剂公司提供的人全血DNA提取试剂盒.
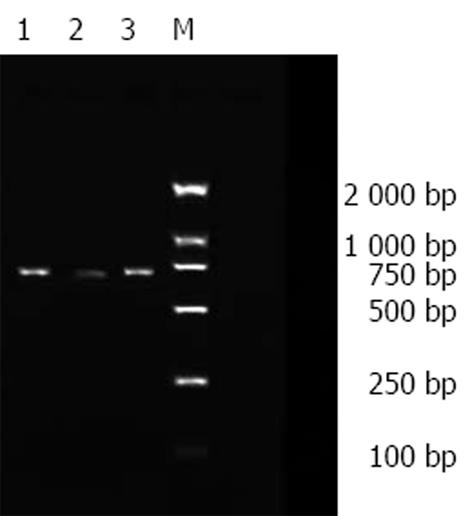
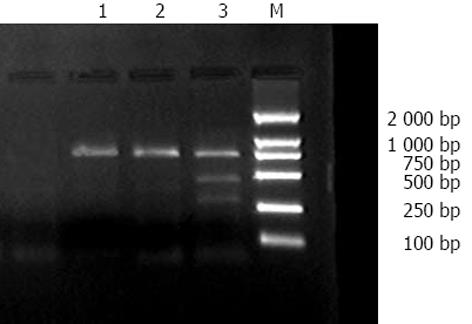
1.2.2 基因多态性检测: 均采用聚合酶链式反应-限制性片段长度多态性(PCR-RFLP)分析. 按文献[31]的报道由上海宝信生物公司合成引物, 其上游引物序列为5' -GGAGACTATTCAGAAGCTAA-3', 下游引物序列为5'-GAAGAGCCTGAAGACTGACT-3'. 预计扩增片段全长为710 bp. 扩增条件: 95 ℃预变性3 min后进入下述循环周期: 95 ℃变性30 s, 56.5 ℃退火30 s, 72 ℃延伸60 s. 35个循环后72 ℃保温7 min结束反应. 以20 g/L的琼脂糖凝胶(含0.5 g/L溴乙錠)水平电泳检测PCR产物. 扩增产物为Apo B基因第26外显子包含Xba I酶切位点的多态性片段, 长度为710 bp. 取PCR扩增产物15 μL加入Xba I酶(立陶宛MBI公司生产、深圳晶美试剂公司提供)15 U, 37 ℃消化过夜后, 以20 g/L的琼脂糖凝胶(含0.5 g/L溴乙錠)120 V稳压电压分离酶切产物40 min,以DL2000 Marker为标准分子量, 在紫外灯下检视各区带并分析结果.仅出现一条710 bp片段为X-X-基因型; 出现433 bp和277 bp两条片段为X+X+基因型; 出现710 bp、433 bp 和277 bp三条片段为X+X-基因型.
1.2.3 肝功及血脂成分的测定: 肝功能、血脂用全自动生物化学分析仪(日本日立株式会社, 7170A)检测. 检查项目有谷丙转氨酶(ALT), 胆固醇(CHO), 高密度脂蛋白(HDL), 低密度脂蛋白(LDL), 载脂蛋白B(Apo B).
1.2.4 血清HCV RNA水平的检测: 采用深圳达安基因有限公司提供的定量试剂盒及实时定量PCR扩增仪检测血清HCV RNA水平.
统计学处理 用SPSS11.0统计学软件分析处理. 计量资料用(mean±SD)表示, 采用t检验; 计数资料用χ2检验.
PCR扩增产物全长710 bp, 与预计长度相符. 将酶切产物进行限制性片段长度多态性分析, 结果显示有两种带型: 仅出现一条710 bp片段为X-X-基因型; 出现710 bp、433 bp和277 bp三条片段为X+X-基因型(图1, 2).
中国汉族人(包括病例及对照)基因型均以X-X-基因型占优势, X+X-杂合子少见, 未见X+X+基因型. 少见的等位基因X+频率在病例组低于对照组, 分别为0.071, 0.121, 但经χ2检验无统计学显著性(P = 0.136, 表1).
| n | X-X-(%) | X+X-(%) | X+X+(%) | X+ | X- | |
| 病例组 | 77 | 66 (85.7) | 11 (14.3) | 0 (0) | 7.1% | 92.9% |
| 对照组 | 62 | 47 (75.8) | 15(24.2) | 0 (0) | 12.1% | 87.9% |
慢性肝炎组的等位基因X+频率明显低于健康对照组, 以肝硬化组为最明显, 但经χ2检验无显著性(P = 0.280, 表2).
| n | X-X-(%) | X+X-(%) | X+X+(%) | X+(%) | X-(%) | |
| 慢性肝炎组 | 65 | 55(84.6) | 10(15.4) | 0(0) | 7.7 | 92.3 |
| 肝硬化组 | 12 | 11(91.7) | 1(8.3) | 0(0) | 4.2 | 95.8 |
| 对照组 | 62 | 47(75.8) | 15(24.2) | 0(0) | 12.1 | 87.9 |
对病例组X-X-和X+X-基因型间的血脂水平进行比较, X+X-组的CHO, LDL, APO B水平均高于X-X-组, 经t检验仅Apo B有统计学意义(P = 0.019); X+X-组的HDL水平低于X-X-组, 但无统计学显著性(表3).
按照血清中HCV RNA的水平, 以HCV RNA<80为阴性, 将慢性丙型肝炎患者分为HCV RNA 阳性组和HCV RNA阴性组, 比较两组间基因型分布的差异性.连续性校正χ2检验显示, 两组之间差异显著(表4).
| n | X-X- | X+X- | X+X+ | X+(%) | X-(%) | |
| 病例组 | 77 | 66 | 11 | 0 | 7.1 | 92.9 |
| HCV RNA<80000 copies/L组 | 14 | 9 | 5 | 0 | 17.9 | 82.1 |
| HCV RNA≥80000 copies/L组 | 63 | 57 | 6 | 0 | 4.8 | 95.2 |
相关性分析显示, 慢性丙型肝炎患者血清Apo B水平与血清HCV RNA水平之间呈直线负相关关系(R =-0.538, P = 0.005), 但与ALT水平无相关性(R = 0.224, P = 0.210).
相关性分析显示, 慢性丙型肝炎患者血清LDL水平与血清HCV RNA水平之间呈直线负相关关系(R = -0.460, P = 0.016), 但与ALT水平无相关性(R = -0.007, P = 0.968).
HCV感染具有宿主特异性, 对其体外研究造成了很大障碍, 其致病机制尚不清楚.目前认为, 阻断HCV感染靶细胞的关键问题是搞清楚宿主细胞表面的HCV受体或辅助受体. 近年来在对感染细胞和机体的大量研究[12,15,16]证实, LDL-R即使不是唯一的, 也是重要的HCV感染靶细胞的受体分子, 并且HCV内化过程是由HCV-LDL/HCV-VLDL复合物通过LDL-R进行的.
载脂蛋白B100 既是LDL的主要载脂蛋白又是细胞表面LDL-R的专一性配体, 许多研究均证实它与HCV感染密切相关. 在丙型肝炎患者的血清中, HCV可与LDL或VLDL相结合而存在[6-9], 而且用抗Apo B抗体可以从感染血清中沉淀出HCV[4]. Andre et al[6]证实纯化的HCV病毒颗粒富含甘油三酯, 且至少含有Apo B, HCV RNA和核心蛋白三种成分; 进一步研究发现抗 Apo B抗体和抗Apo E抗体可以阻断病毒颗粒进入细胞, 反之上调LDL-R可以促进病毒颗粒的细胞内化作用. Petit et al[18]报道HCV感染者血清Apo B水平显著低于正常人, 而且Apo B水平与肝脏脂肪变性和HCV病毒载量呈现负相关关系. 这些研究充分证明, 载脂蛋白B是HCV感染靶细胞所依赖的重要的内源性蛋白质之一.
载脂蛋白B100基因结构现已充分阐明, 人类Apo B100基因定位于第二号染色体短臂末端, 全长43 kb, 包含29个外显子和28个内含子. 在已知的基因中, Apo B100基因具有最明显的多态性. 某些位点的多态性与血脂变化及LDL受体结合相关, Xba I位点就是研究较多的一个. Xba I酶切位点的多态性是由于2 488位密码子第三个碱基突变(ACC→ACT), 产生一个Xba I酶切位点, 但并未改变所编码的氨基酸序列. 以往的研究虽然对Xba I位点的多态性是否是缺血性心脏病或冠心病的易感因素存在争议[25,26,32,33], 却一致认为Xba I酶切位点多态性可明显影响血脂水平[24-29]. 纯合子X+ X+基因型血浆中TC、LDL、Apo B100水平最高, 杂合子X+X-次之, 纯合子X-X-最低[25,28,29,33]. 体外动力学研究发现, X+X+基因型的LDL与其受体结合力及经受体介导的清除率均低于具X-X-基因型的LDL[22].
本研究结果显示, 中国汉族人(包括病例及对照) Apo B基因型均以X-X-基因型占优势, X+X-杂合子少见, 未见X+X+基因型; 对照组X+等位基因频率略高于以往国内文献报道[23,29], 明显低于白种人[26,33], 提示X+等位基因的频率存在明显的种族特异性. 本研究发现, 丙型肝炎患者的X+等位基因频率低于健康对照组, 以肝硬化组为著, 但无统计学意义, 其原因可能是: (1)该位点的多态性与人群对HCV的易感性没有必然的联系; (2)与统计样本量相对较少有关. 在不同病毒载量的慢性丙肝患者组之间, Apo B基因Xba I位点基因型分布存在显著差异. HCV RNA≥80组X+等位基因频率低于HCV RNA<80组, 提示由于杂合子X+X-基因型的LDL与其受体结合力及经受体介导的清除率均低于纯合子X-X-基因型, 可能影响了HCV感染靶细胞的效率, 因而导致其血清中病毒血症水平较低. 我们比较了病例组各种基因型间的血脂水平, 发现X+X-组的CHO, LDL, APO B水平均高于X-X-组, 仅APO B有统计学意义(P = 0.019). 这一结果与以往的国内外研究结果相符[25,28,29,33]. 虽然Xba I位点的变异并未改变所编码的氨基酸序列, 但可通过减弱LDL与其受体的结合, 降低LDL的分解代谢率而使血浆CHO , LDL, APO B水平升高.
我们还发现, 慢性丙型肝炎患者血清Apo B水平、血清LDL水平与血清HCV RNA水平之间均呈显著负相关关系. 这与相关文献报道[17,18]一致, 其机制可能为血清中Apo B、LDL通过与LDL-R的结合而竞争性的抑制了HCV病毒颗粒的细胞内化作用, 因而随着血清Apo B水平、血清LDL水平的升高而血清病毒载量趋于下降. 本研究中我们未发现血清Apo B水平、血清LDL水平与ALT水平的相关性, 其原因可能是: (1)转氨酶的影响因素较多; (2)血清Apo B水平、血清LDL水平对病毒载量的影响远远超过其对肝损伤的影响, 而肝脏的损伤程度还与宿主的免疫反应密切相关, 二者之间并不是平行发展的.
总之, 我们观察到 Apo B基因Xba I位点的多态性、血清Apo B水平、血清LDL水平均可显著影响慢性丙型肝炎患者的血清HCV RNA水平. 尚需扩大样本量进行证实及更深入的研究. 如载脂蛋白B的基因多态性和丙型肝炎临床病程、预后有无关系?载脂蛋白B仅仅是作为HCV的运输和结构蛋白存在而影响血清HCV水平, 还是有其他的影响机制?单采浆血浆分离置换法降低丙型肝炎患者病毒负荷的机制是什么?弄清这些关系, 不仅对我们认识HCV与其受体作用的机制有重要意义, 而且有助于探索治疗HCV感染的新方法.
电编: 张勇 编辑: 菅鑫妍 审读: 张海宁
| 2. | Zoulim F, Chevallier M, Maynard M, Trepo C. Clinical consequences of hepatitis C virus infection. Rev Med Virol. 2003;13:57-68. [PubMed] [DOI] |
| 3. | 张 妮, 刘 正稳. 瘦素及其与肝脏脂肪变性和慢性丙型肝炎的关系. 国外医学. 生理、病理科学与临床分册. 2003;23:185-187. |
| 4. | Thomssen R, Bonk S, Propfe C, Heermann KH, Kochel HG, Uy A. Association of hepatitis C virus in human sera with beta-lipoprotein. Med Microbiol Immunol. 1992;181:293-300. [PubMed] [DOI] |
| 5. | Thmssen R, Bonk S, Thiele A. Density heterogeneities of hepatitis C virus in human sera due to the binding of beta- lipoproteins and immunoglobulins. Med Microbiol Immunol. 1993;182:329-334. [PubMed] |
| 6. | Andre P, Komurian-Pradel F, Deforges S, Perret M, Berland JL, Sodoyer M, Pol S, Brechot C, Paranhos-Baccala G, Lotteau V. Characterization of low- and very-low-density hepatitis C virus RNA-containing particles. J Virol. 2002;76:6919-6928. [PubMed] [DOI] |
| 7. | Prince AM, Huima-Byron T, Parker TS, Levine DM. Visualization of hepatitis C virions and putative defective interfering particles isolated from low-density lipoproteins. J Viral Hepat. 1996;3:11-17. [PubMed] [DOI] |
| 8. | Thomssen R, Bonk S. Virolytic action of lipoprotein lipase on hepatitis C virus in human sera. Med Microbiol Immunol. 2002;191:17-24. [PubMed] [DOI] |
| 9. | Kono Y, Hayashida K, Tanaka H, Ishibashi H, Harada M. High-density lipoprotein binding rate differs greatly between genotypes 1b and2a/2b of hepatitis C virus. J Med Virol. 2003;70:42-48. [PubMed] [DOI] |
| 10. | Polgreen PM, Fultz SL, Justice AC, Wagner JH, Diekema DJ, Rabeneck L, Weissman S, Stapleton JT. Association of hypocholesterolaemia with hepatitis C virus infection in HIV-infected people. HIV Med. 2004;5:144-150. [PubMed] [DOI] |
| 11. | Agnello V, Abel G, Elfahal M, Knight GB, Zhang QX. Hepatitis C virus and other flaviviridae viruses enter cells via low density lipoprotein receptor. Proc Natl Acad Sci U S A. 1999;96:12766-12771. [PubMed] [DOI] |
| 12. | Monazahian M, Bohme I, Bonk S, Koch A, Scholz C, Grethe S, Thomssen R. Low density lipoprotein receptor as a candidate receptor for hepatitis C virus. J Med Virol. 1999;57:223-229. [PubMed] [DOI] |
| 13. | Wunschmann S, Medh JD, Klinzmann D, Schmidt WN, Stapleton JT. Characterization of hepatitis C Virus (HCV) and HCV E2 interactions with CD81 and the low-density lipoprotein receptor. J Virol. 2000;74:10055-10062. [PubMed] [DOI] |
| 14. | Monazahian M, Kippenberger S, Muller A, Seitz H, Bohme I, Grethe S, Thomssen R. Binding of human lipoproteins (low, very low, high density lipoproteins) to recombinant envelope proteins of hepatitis C virus. Med Microbiol Immunol. 2000;188:177-184. [PubMed] [DOI] |
| 15. | Meyer K, Basu A, Ray R. Functional features of hepatitis C virus glycoproteins for pseudotype virus entry into mammalian cells. Virology. 2000;276:214-226. [PubMed] [DOI] |
| 16. | Lambot M, Fretier S, Op De Beeck A, Quatannens B, Lestavel S, Clavey V, Dubuisson J. Reconstitution of hepatitis C virus envelope glycoproteins into liposomes as a surrogate model to study virus attachment. J Biol Chem. 2002;277:20625-20630. [PubMed] [DOI] |
| 17. | Enjoji M, Nakamuta M, Kinukawa N, Sugimoto R, Noguchi K, Tsuruta S, Iwao M, Kotoh K, Iwamoto H, Nawata H. Beta- lipoproteins influence the serum level of hepatitis C virus. Med Sci Monit. 2000;6:841-844. [PubMed] |
| 18. | Petit JM, Benichou M, Duvillard L, Jooste V, Bour JB, Minello A, Verges B, Brun JM, Gambert P, Hillon P. Hepatitis C virus- associated hypobetalipoproteinemia is correlated with plasma viral load, steatosis, and liver fibrosis. Am J Gastroenterol. 2003;98:1150-1154. [PubMed] [DOI] |
| 19. | Marson P, Boschetto R, De Silvestro G, Martini S, Gabelli C, Buoro S, Giordano R, Palu G. Changes in HCV viremia following LDL apheresis in a HCV positive patientwith familial hypercholesterolemia. Int J Artif Organs. 1999;22:640-644. [PubMed] |
| 20. | Schettler V, Monazahian M, Wieland E, Ramadori G, Grunewald RW, Thomssen R, Muller GA. Reduction of hepatitis C virus load by H.E.L.P.LDL apheresis. Eur J Clin Invest. 2001;31:154-155. [PubMed] [DOI] |
| 21. | Schettler V, Monazahian M, Wieland E, Thomssen R, Muller GA. Effect of heparin-induced extracorporeal low-density lipoprotein precipitation (HELP) apheresis on hepatitis C plasma virus load. Ther Apher. 2001;5:384-386. [PubMed] [DOI] |
| 22. | Series J, Cameron I, Caslake M, Gaffney D, Packard CJ, Shepherd J. The Xba1 polymorphism of the apolipoprotein B gene influences the degradation of low density lipoprotein in vitro. Biochim Biophys Acta. 1989;1003:183-188. [PubMed] [DOI] |
| 24. | Tahri-Daizadeh N, Tregouet DA, Nicaud V, Poirier O, Cambien F, Tiret L. Exploration of multilocus effects in a highly polymorphic gene, the apolipoprotein (APOB) gene, in relation to plasma apoB levels. Ann Hum Genet. 2004;68:405-418. [PubMed] [DOI] |
| 25. | Benn M, Nordestgaard BG, Jensen JS, Grande P, Sillesen H, Tybjaerg-Hansen A. Polymorphism in APOB associated with increased low-density lipoprotein levels in both genders in the general population. J Clin Endocrinol Metab. 2005;90:5797-5803. [PubMed] [DOI] |
| 26. | Turner PR, Talmud PJ, Visvikis S, Ehnholm C, Tiret L. DNA polymorphisms of the apoprotein B gene are associated with altered plasma lipoprotein concentrations but not with perceived risk of cardiovasculardisease: European Atherosclerosis Research Study. Atherosclerosis. 1995;116:221-234. [PubMed] [DOI] |
| 27. | Peacock R, Dunning A, Hamsten A, Tornvall P, Humphries S, Talmud P. Apolipoprotein B gene polymorphisms, lipopr- oteins and coronary atherosclerosis: a study of young myocardial infarction survivors and healthy population-based individuals. Atherosclerosis. 1992;92:151-164. [PubMed] [DOI] |
| 28. | Han T, Jiang Z, Suo G, Zhang S. Apolipoprotein B-100 gene Xba I polymorphism and cholesterol gallstone disease. Clin Genet. 2000;57:304-308. [PubMed] [DOI] |
| 29. | Tan YF, Yang S, Yu RB, Shen C, Ding WL, Zhou WM, Gong WD, Yao CL. Relationship among the XhaI and EcoRI locus polymorphisms of apolipoprotein B gene, serum lipid metabolism and gallstone disease. Zhonghua Yi Xue Za Zhi. 2003;83:844-847. [PubMed] |
| 30. | Singh MK, Pandey UB, Ghoshal UC, Srivenu I, Kapoor VK, Choudhuri G, Mittal B. Apolipoprotein B-100 XbaI gene polymorphism in gallbladder cancer. Hum Genet. 2004;114:280-283. [PubMed] [DOI] |
| 31. | Boerwinkle E, Lee SS, Butler R, Schumaker VN, Chan L. Rapid typing of apolipoprotein B DNA polymorphisms by DNA amplification. Association between Ag epitopes of human apolipoprotein B-100, a signal peptide insertion/deletion polymorphism, and a 3'flanking DNA variable number of tandem repeats polymorphism of the apolipoprotein B gene. Atherosclerosis. 1990;81:225-232. [PubMed] [DOI] |
| 32. | Scartezini M, Zago MA, Chautard-Freire-Maia EA, Pazin-Filho A, Marin-Neto JA, Hotta JK, Nascimento AJ, Dos-Santos JE. The X-X-/E+E+ genotype of the XbaI/EcoRI polymorphisms of the apolipoprotein B gene as a marker of coronary artery disease in a Brazilian sample. Braz J Med Biol Res. 2003;36:369-375. [PubMed] [DOI] |
| 33. | Islam MS, Raitakari OT, Juonala M, Kahonen M, Hutri-Kahonen N, Collings A, Aalto-Setala K, Kontula K, Marniemi J, Viikari JS. Apolipoprotein A-I/C-III/A-IV SstI and apolipoprotein B XbaI polymorphisms and their association with carotid artery intima-media thickness in the Finnish population. The Cardiovascular Risk in Young Finns Study. Atherosclerosis. 2005;180:79-86. [PubMed] [DOI] |