修回日期: 2003-10-20
接受日期: 2003-11-13
在线出版日期: 2004-03-15
目的: 明确黄色肉芽肿性胆囊炎的超声表现特征, 以提高影像诊断的正确性.
方法: 回顾性分析经手术病理证实的黄色肉芽肿性胆囊炎32例的超声表现. 男17例, 女15例, 年龄21-88(平均55.3岁).
结果: 所有患者均有胆囊壁增厚, 壁厚4-6 mm为15例 (46.9%), 7-10 mm 14例(43.8%), 11-22 mm 3例(9.3%). 内壁光滑20例(62.5%), 内壁不光滑12例(37.5%). 壁间低回声结节5例(15.6%), 壁间结石1例(3.1%). 合并胆石症30例(93.8%), 其中单纯胆囊结石22例(68.8%), 单纯胆总管结石2例(6.3%), 胆囊结石合并胆总管结石6例 (18.8%). 浸润肝脏形成等回声或弱回声团块2例(6.3%).
结论: 黄色肉芽肿性胆囊炎主要表现为胆囊壁不同程度增厚, 可有壁内低回声结节, 常伴有胆囊结石或胆管结石. 超声检查可反映黄色肉芽肿性胆囊炎的病理改变.
引文著录: 张梅, 彭玉兰, 罗燕, 庄华, 杨志刚. 黄色肉芽肿性胆囊炎的超声表现及其病理学基础. 世界华人消化杂志 2004; 12(3): 738-740
Revised: October 20, 2003
Accepted: November 13, 2003
Published online: March 15, 2004
AIM: To determine the sonographic features of xantho-granulomatous cholecystitis (XGC), which could improve imaging diagnosis.
METHODS: The sonographic features of 32 patients with surgically resected XGC were retrospectively evaluated on the basis of the surgical and pathological findings. The patients were 15 women and 17 men, aged from 21 to 88 (mean 55.3) years.
RESULTS: The gallbladder wall was thickened in all patients. Among the 32 cases, 15 (46.9%) were between 4 mm to 6 mm; 14 (43.8%) were between 7 mm to 10 mm; 3 (9.3%) were between 11 mm to 22 mm. On the membranous surface of the gallbladder wall, 20 (62.5%) were smooth, while 12 (37.5%) were uneven. Other manifestations included intramural hypoechoic nodule in 5 (15.6%), intramural cholelithiasis in 1 (3.1%), and cholelithiasis 30 (93.8%), respectively. Two patients (6.3%) had liver hypoechoic or iso-echoic mass resulted from the infiltration of XGC.
CONCLUSION: Sonographic manifestations present thickened gallbladder wall, with intramural hypoechoic nodules and/or cholelithiasis. Sonographic examination can reveal the surgical and pathological findings of the XGC.
- Citation: Zhang M, Peng YL, Luo Y, Zhuang H, Yang ZG. Xanthogranulomatous cholecystitis: Sonographic, surgical and pathologic correlation. Shijie Huaren Xiaohua Zazhi 2004; 12(3): 738-740
- URL: https://www.wjgnet.com/1009-3079/full/v12/i3/738.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v12.i3.738
黄色肉芽肿性胆囊炎(xanthogranulomatous cholecystitis, XGC)是一种以胆囊慢性炎症为基础, 伴胆囊肉芽肿、重度增生纤维化以及泡沫样组织细胞为特征的炎性病变[1-3]. XGC的临床及超声表现难以与胆囊炎胆石症鉴别[4]. 当XGC的胆囊壁弥漫性明显增厚呈实性改变, 局部明显增厚形成瘤样肿块或伴有肝脏浸润时, 易误诊为胆囊癌 [5-20]. 为此, 我们对32例经手术病理证实的XGC进行回顾性分析, 着重探讨其超声表现特征及其病理学基础, 以提高该疾病的影像诊断准确性.
我院1997-06/2003-06超声检查后经手术及病理证实的XGC 32例. 男17例, 女15例. 年龄21-88(平均55.3岁). 病程4 d-30 a, 平均31 mo. 有右上腹疼痛史30例, 无疼痛史2例, 分别因黄疸及体检就诊. 有多次胆囊炎急性发作史21例. 发热2例, 皮肤黄疸11例, 腹部包块3例.
仪器为TOSHIBA-240, RTFINO, HDI3500型超声诊断仪, 探头频率3.5 MHz. 常规检查胆囊及胆道系统. 观察胆囊大小、壁厚、胆囊壁回声情况, 有无胆囊结石、胆管结石和胆道扩张, 胆囊与肝实质分界情况, 有无肝实质浸润灶以及上腹部淋巴结长大. 所有标本均纵行剖开, 40 g/L甲醛液固定, 常规石蜡包埋, 切片, HE染色, 光镜观察.
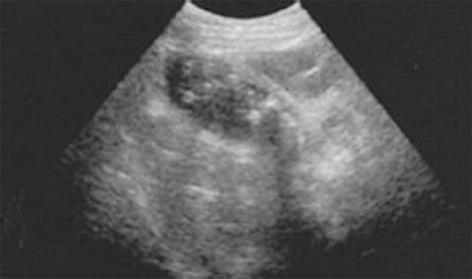
所有患者均有胆囊壁增厚(图1-3), 壁厚4-6 mm 15例(46.9%), 7-10 mm 14例(43.8%), 11-22 mm 3例(9.3%). 内壁不光滑12例(37.5%), 内壁光滑20例(62.5%). 壁间低回声结节5例(15.6%, 图1), 壁间结石1例(3.1%, 图2). 胆囊长大12例(37.5%), 胆囊缩小6例(18.8%), 胆囊正常大小14例(43.8%). 合并胆石症30例(93.8%), 其中单纯胆囊结石22例(68.8%, 图3), 单纯胆总管结石2例(6.3%), 胆囊结石合并胆总管结石6例(18.8%). 胆囊与肝脏分界欠清4例(12.5%). 累及肝外胆管致胆道梗阻2例(6.3%). 伴上腹部包裹性积液1例. 门静脉旁可见长大的淋巴结1例(3.1%, 表1). 超声疑诊为胆囊癌5例, 其中1例形成从囊壁突向囊腔的等回声团块, 大小约30 mm×22 mm; 2例可见与胆囊相连的胆囊旁肝实质内等回声或低回声团块, 直径40 mm-60 mm, 团块边界清楚; 2例胆囊缩小、胆囊壁明显增厚呈实性改变.
| 观察指标 | n (%) |
| 胆囊 长大 | 12 (37.5%) |
| 缩小 | 6 (18.8%) |
| 内壁光滑 | 20 (62.5%) |
| 内壁不光滑 | 12 (37.5%) |
| 壁间低回声结节 | 5 (15.6%) |
| 壁间结石 | 1 (3.1%) |
| 胆石症单纯胆囊结石 | 22 (68.8%) |
| 单纯胆总管结石 | 2 (6.3%) |
| 胆囊结石合并胆总管结石 | 6 (18.8%) |
| 胆囊与肝脏分界清楚 | 28 (87.5%) |
| 分界不清楚 | 4 (12.5%) |
| 上腹部淋巴结 | |
| 未见长大 | 31 (96.9%) |
| 长大 | 1 (3.1%) |
剖开切下的胆囊, 见胆囊壁不同程度地增厚、质硬, 部分水肿明显, 可见壁间黄绿色结节, 显微镜下见胆囊壁内大量泡沫样组织细胞、急慢性炎症细胞、纤维母细胞、异物巨细胞等形成的特征性肉芽肿. 术中见单纯胆囊结石22例(图3), 单纯胆总管结石2例, 胆囊结石合并胆总管结石6例. 多数病例黏膜平滑, 少数凹凸不平, 结石嵌顿处黏膜糜烂. 胆囊与周围组织不同程度的粘连或被网膜包裹. 胆囊壁部分坏疽5例, 胆囊穿孔伴上腹部包裹性积液1例, 胆囊胆总管内瘘2例, Mirizzi综合征1例. 累及肝外胆管致慢性炎症2例. 累及肝脏致肝间质慢性炎细胞浸润、肝细胞脂肪变性4例. 2例胆囊旁肝实质内形成浸润灶时可见纤维组织大量增生, 大量炎细胞浸润. 1例门静脉旁见大小分别为30 mm×20 mm及10 mm×5 mm的淋巴结, 病理为淋巴结反应性增生改变. 所有病例均未见肿瘤细胞.
1970年, Christensen首次报道7例XGC. 本病占同期胆囊切除术的0.7-11.2%, 以50-60岁多见, 本组平均年龄为55.3岁. XGC与胆囊结石或胆道结石密切相关, 文献[9]报道达78-96%, 本组30例, 占93.8%. XGC的临床表现缺乏特异性, 常有反复发作的右上腹疼痛, 可伴有黄疸、发热, 偶能触及肿大的胆囊. XGC的发病机制尚不十分清楚, 多数学者认为由急性炎症和梗阻综合因素引起[1-3,21-24]. 胆汁沿着破裂的Rokitansky-Aschoff窦或黏膜溃疡病灶不断渗入至胆囊壁, 组织细胞聚集, 吞噬胆汁中的胆固醇, 形成富含脂质的泡沫样组织细胞, 随着病程发展, 病灶扩大, 纤维组织大量增生, 形成炎性肉芽肿块, 并与肝脏或临近器官粘连、浸润. 有时影像学检查可将XGC误诊为胆囊癌, 因此世界卫生组织(WHO)对胆道肿瘤组织学分类时也将XGC列入其中[9].
XGC病理上根据病变累及范围分为两型: (2)局限型: 胆囊壁正常结构受到不同程度破坏, 代之以结节性肉芽肿结构, 胆囊壁增厚, 壁间形成单一或多发病灶, 直径3-30 mm的黄绿色结节: (2)弥漫型: 病变浸润胆囊壁全层, 并向外侵犯脂肪结缔组织及临近器官[6,14,24]. 本组病例均有胆囊壁的增厚, 多数内壁光滑, 部分胆囊壁内见低回声结节, 病理为大量泡沫样组织细胞、急慢性炎症细胞、纤维母细胞、异物巨细胞等形成的特征性黄色肉芽肿. 少数内壁凹凸不平, 结石嵌顿处黏膜糜烂, 镜下见病变主要位于胆囊壁内, 被黏膜覆盖. XGC常伴胆囊结石或胆道结石, 本组有30例, 占93.8%. 当病变累及肝外胆管时, 超声表现为肝外胆管壁增厚、管腔狭窄, 并致肝内胆管梗阻性扩张, 与手术发现一致, 病理为胆管慢性炎症. 当肝脏受侵时, 超声显示胆囊与肝脏分界欠清, 还可形成与胆囊相连的肝实质内占位团块, 手术发现为胆囊与周围组织不同程度粘连或被网膜包裹, 病理证实为胆囊周围炎性反应和肝慢性炎细胞浸润. 超声所见胆囊旁肝实质内占位团块, 病理为肝脏浸润灶内纤维组织大量增生, 大量炎细胞浸润.
本病被认为是一种少见、良性并有破坏性的胆囊炎性病变[9-10,15]. 可伴发胆囊壁坏疽、胆囊穿孔、内瘘、Mirizzi综合征、胆管炎性狭窄致胆道梗阻. 其并发症发生率高, 本组11例, 占34%, 主要为胆囊壁坏疽性改变, 其次为胆囊壁穿孔后内瘘的形成. 据文献[5,9,14]报道有10%的XGC合并胆囊癌, 但本组无病例并发胆囊癌. XGC是否属于癌前病变有待进一步证实. 因此, 当超声发现持续性壁增厚的慢性胆囊炎时, 应尽早手术, 或针吸活检, 以获得组织学证据. Maguruma et al 报告采用腔内超声也有利于XGC的诊断.
在临床诊断中, 采用影像学方法可鉴别XGC与胆囊癌[1,3,6,11,24]. 当XGC的胆囊壁弥漫性明显增厚呈实性改变、局部明显增厚形成瘤样肿块或伴有肝脏浸润灶时, 须与胆囊癌相鉴别. 以下XGC的影像学表现特点有助于与胆囊癌鉴别: (1)胆囊壁增厚. 抗炎治疗后胆囊壁持续增厚且病程较长时, 提示XGC的可能; (2)超声示胆囊内壁光滑, 本组20例, 占62.5%, CT显示为黏膜线的连续, 此点对XGC与胆囊癌的鉴别诊断很有帮助; (3)胆囊壁局限性病变者, 超声示壁内低回声结节, 本组5例, 占15.6%, CT示胆囊壁间低密度结节区域占据增厚的胆囊壁较大区域时(有文献报道为超过60%), 高度提示XGC; (4)绝大多数患者上腹部未见长大的淋巴结, 本组31例, 占96.9%. 而胆囊癌生物学恶性度高, 肿瘤细胞易沿淋巴引流扩散, 常致门腔间隙、肝门以及腹腔动脉周围淋巴结长大. 因此, 有无上腹部淋巴结长大, 也有助于XGC与胆囊癌相鉴别.
编辑: N/A
| 1. | Chun KA, Ha HK, Yu ES, Shinn KS, Kim KW, Lee DH, Kang SW, Auh YH. Xanthogranulomatous cholecystitis: CT features with emphasis on differentiation from gallbladder carcinoma. Radiology. 1997;203:93-97. [PubMed] [DOI] |
| 2. | Hsu C, Hurwitz JL, Schuss A, Katz DS. Radiology-Pathology Conference: Xanthogranulomatous cholecystitis. Clin Imaging. 2003;27:421-425. [PubMed] [DOI] |
| 3. | Kim PN, Lee SH, Gong GY, Kim JG, Ha HK, Lee YJ, Lee MG, Auh YH. Xanthogranulomatous cholecystitis: radiologic findings with histologic correlation that focuses on intramural nodules. AJR Am J Roentgenol. 1999;172:949-953. [PubMed] [DOI] |
| 5. | Ros PR, Goodman ZD. Xanthogranulomatous cholecystitis versus gallbladder carcinoma. Radiology. 1997;203:10-12. [PubMed] [DOI] |
| 6. | Parra JA, Acinas O, Bueno J, Güezmes A, Fernández MA, Fariñas MC. Xanthogranulomatous cholecystitis: clinical, sonographic, and CT findings in 26 patients. AJR Am J Roentgenol. 2000;174:979-983. [PubMed] [DOI] |
| 10. | Enomoto T, Todoroki T, Koike N, Kawamoto T, Matsumoto H. Xanthogranulomatous cholecystitis mimicking stage IV gallbladder cancer. Hepatogastroenterology. 2003;50:1255-1258. [PubMed] |
| 11. | Gore RM, Yaghmai V, Newmark GM, Berlin JW, Miller FH. Imaging benign and malignant disease of the gallbladder. Radiol Clin North Am. 2002;40:1307-1323, vi. [PubMed] [DOI] |
| 12. | Levy AD, Murakata LA, Abbott RM, Rohrmann CA Jr. From the archives of the AFIP. Benign tumors and tumorlike lesions of the gallbladder and extrahepatic bile ducts: radiologic-pathologic correlation. Armed Forces Institute of Pathology. Radiographics. 2002;22:387-413. [PubMed] [DOI] |
| 13. | Levy AD, Murakata LA, Rohrmann CA Jr. Gallbladder carcinoma: radiologic-pathologic correlation. Radiographics. 2001;21:295-314; questionnaire, 549-555. [PubMed] [DOI] |
| 15. | Roels K, Bogaert J, Van Hoe L, Vanbeckevoort D, Delvaux S. Xanthogranulomatous cholecystitis associated with a xanthogranulomatous pseudotumour on the left diaphragm. Eur Radiol. 1999;9:1139-1141. [PubMed] [DOI] |
| 16. | Yoshida J, Chijiiwa K, Shimura H, Yamaguchi K, Kinukawa N, Honda H, Tanaka M. Xanthogranulomatous cholecystitis versus gallbladder cancer: clinical differentiating factors. Am Surg. 1997;63:367-371. [PubMed] |
| 19. | Maeda T, Shimada M, Matsumata T, Adachi E, Taketomi A, Tashiro Y, Tsuneyoshi M, Sueishi K, Sugimachi K. Xanthogranulomatous cholecystitis masquerading as gallbladder carcinoma. Am J Gastroenterol. 1994;89:628-630. [PubMed] |
| 20. | Howard TJ, Bennion RS, Thompson JE Jr. Xanthogranulomatous cholecystitis: a chronic inflammatory pseudotumor of the gallbladder. Am Surg. 1991;57:821-824. [PubMed] |
| 21. | Casas D, Pérez-Andrés R, Jiménez JA, Mariscal A, Cuadras P, Salas M, Gómez-Plaza MC. Xanthogranulomatous cholecystitis: a radiological study of 12 cases and a review of the literature. Abdom Imaging. 1996;21:456-460. [PubMed] [DOI] |
| 22. | Houston JP, Collins MC, Cameron I, Reed MW, Parsons MA, Roberts KM. Xanthogranulomatous cholecystitis. Br J Surg. 1994;81:1030-1032. [PubMed] [DOI] |
| 23. | Moldavsky M, Hadary A, Turani H. Xanthogranulomatous cholecystitis. Acta Cytol. 1998;42:1050-1051. [PubMed] |
| 24. | Kim PN, Ha HK, Kim YH, Lee MG, Kim MH, Auh YH. US findings of xanthogranulomatous cholecystitis. Clin Radiol. 1998;53:290-292. [PubMed] [DOI] |