修回日期: 2003-08-10
接受日期: 2003-09-18
在线出版日期: 2004-02-15
目的: 评价结肠充气CT对检测大肠肿瘤的敏感性和特异性.
方法: 对100例临床怀疑大肠肿瘤的患者进行结肠充气CT和结肠镜检查.
结果: 结肠镜检测出大肠癌13例, 大肠息肉23例, 共46个息肉(11个直径大于或等于1 cm, 14个直径在6-9 mm, 21个直径≤5 mm). 结肠充气CT检测出大肠癌15例(其中假阳性1例), 大肠息肉16个(9个直径大于或等于1 cm). 结肠充气CT对检测大肠癌的敏感性100% (95%可信区间(confidence interval, CI) (75%-100%), 特异性93%(95%CI: 66%-100%); 对检测大肠癌+直径大于或等于1 cm息肉的敏感性92%(95%CI: 73%-99%), 特异性96% (95%CI: 78%-100%). 结肠充气CT还检测出结肠镜未发现的大肠癌1例, 2例大肠癌患者的远处转移和1例其他肿瘤.
结论: 结肠充气CT对检测大肠癌和直径1cm以上息肉有很高的敏感性和特异性, 但对直径1cm以下息肉检出率低. 对于临床可疑的大肠癌患者, 结肠充气CT可作为检测结肠癌的初步检查手段.
引文著录: 王毅, 龚水根, 张伟国, 陈金华, 张连阳, 陈金萍. 结肠充气CT对检测大肠肿瘤的敏感性和特异性. 世界华人消化杂志 2004; 12(2): 359-362
Revised: August 10, 2003
Accepted: September 18, 2003
Published online: February 15, 2004
AIM: To evaluate the sensitivity and specificity of pneumocolon computed tomography (CT) in the detection of colorectal neoplasms.
METHODS: A total of 100 patients with suspected colorectal neoplasms underwent both pneumocolon CT and colonoscopy.
RESULTS: On colonoscopy 13 colorectal carcinomas were detected in 13 patients, and 46 polyps in 24 patients (11 polyps were ≥ 1 cm in diameter, 14 were 6-9 mm, and 21 were ≤ 5 mm). Pneumocolon CT detected 15 cancers (included one false positive cancer), but only 16 polyps (9 were ≥ 1 cm). This resulted in a sensitivity of 100% (95% confidence interval (CI) 75%-100%) and specificity of 93% (95%CI: 66%-100%) for detection of colorectal carcinoma, and a sensitivity of 93% (95%CI: 73%-99%) and specificity of 96% (95%CI: 78%-100%) for detection of carcinoma and/or ≥ 1 cm polyps. Pneumocolon CT also identified carcinoma not seen at colonoscopy in one patient, and detected metastases in 2 colorectal carcinoma patients and extracolonic carcinoma in one patient.
CONCLUSION: Pneumocolon CT has a high sensitivity and specificity for detection of colorectal carcinoma and/or ≥1 cm colorectal polyps but not for < 1 cm colorectal polyps. Pneumocolon CT may be suitable for initial investigation of patients with symptoms of colorectal malignancy.
- Citation: Wang Y, Gong SG, Zhang WG, Chen JH, Zhang LY, Chen JP. Sensitivity and specificity of pneumo-colon CT in detecting colorectal neoplasms. Shijie Huaren Xiaohua Zazhi 2004; 12(2): 359-362
- URL: https://www.wjgnet.com/1009-3079/full/v12/i2/359.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v12.i2.359
结肠镜是目前检测大肠肿瘤最准确的方法[1-10], 并能通过他进行活组织检查和息肉切除[11-14]. 但大肠CT检查无创伤性, 可供观察全段大肠, 主要的技术有结肠充气CT、CT结肠造影术和CT仿真结肠镜[2,15-17]. 结肠充气CT较CT仿真结肠镜的优势是检查时间短, 操作简便, 无需特殊软件来进行三维重建, 并能清晰观察CT仿真结肠镜显示不理想的肠管外软组织结构[18-21]. 我们评价结肠充气CT对检测大肠肿瘤的敏感性和特异性.
疑有大肠肿瘤的患者100例, 男63例, 女37例, 平均年龄61(43-82)岁. 临床表现有腹痛47例, 便血41例, 排便习惯改变32例, 可疑腹部肿块21例, 贫血18例, 消瘦16例, 钡剂灌肠检查提示结肠异常11例和结肠梗阻2例. 具有大肠癌家族史的无症状个体不作为本研究的对象.
检查前1 d对患者作清洁肠道准备, 扫描前10 min静脉内注射盐酸山莨菪碱10 mg, 然后向直肠内插入Foley管, 缓慢地注入空气直到患者有腹胀感, 最大用量不超过2 L. 采用Siemen Somatom Plus 4型螺旋CT机进行检查. 患者于仰卧位, 扫描条件: 准直8 mm, 螺距1.5 cm, 完成扫描后用4 mm间隔重建. 所有患者均行平扫加增强, 增强扫描以3 mL/s的速度注入造影剂100 mL. 扫描范围下至耻骨联合, 上至膈顶. CT检查后休息1 h以上, 行结肠镜检查. 检查前静脉注射安定及哌替啶. 设备为Olympus Keymed CF 200-HL结肠镜及其附件. 操作时做到手法轻柔, 合理注气, 循腔进镜, 反复钩拉, 必要时变换体位, 争取较短的时间到达回盲部. 记录每段结肠(包括右侧结肠、横结肠、左侧结肠和乙直肠)的异常发现, 通过活检钳估计息肉的大小, 或切除息肉术直接测量, 并记录检查的完整性和患者的耐受情况.
统计学处理 采用NoSA统计分析软件对所得数据进行χ2检验.
结肠镜检查成功到达盲肠89例(89%), 其中51例表现正常. 11例失败的原因包括肠道准备不足(6例)、肠管结构复杂(2例)、肿瘤梗阻(2例)和患者不能耐受(1例), 其中8例所见肠管无异常发现. 结肠镜共检出大肠肿瘤36例(36%), 其中13例为侵袭性大肠癌, 46个息肉分布于23例患者中, 其中1例合并有侵袭性大肠癌. 9例大肠癌和37个息肉位于左侧结肠内或其远端, 均在距离肛缘60cm的范围内(表1). 对46个息肉中的41个进行了病理学检查, 40个得到证实, 而1个位于降结肠大小约1 cm的息肉病理学结果为原位腺癌. 5个息肉未能得到病理学检查, 直径均在5 mm以下. 13例大肠癌均得到病理学证实. 另外结肠镜还发现5例其他异常, 包括3例结肠憩室和2例溃疡性结肠炎.
| 检查方法 | 息肉直径(mm) | 息肉部位 | 癌 | |||||
| 1-5 | 6-9 | ≥10 | 右 | 横 | 左 | 乙直 | ||
| 结肠充气CT | 2 | 5 | 9 | 1 | 2 | 4 | 9 | 14 |
| 结肠镜 | 21 | 14 | 11 | 5 | 4 | 13 | 24 | 13 |
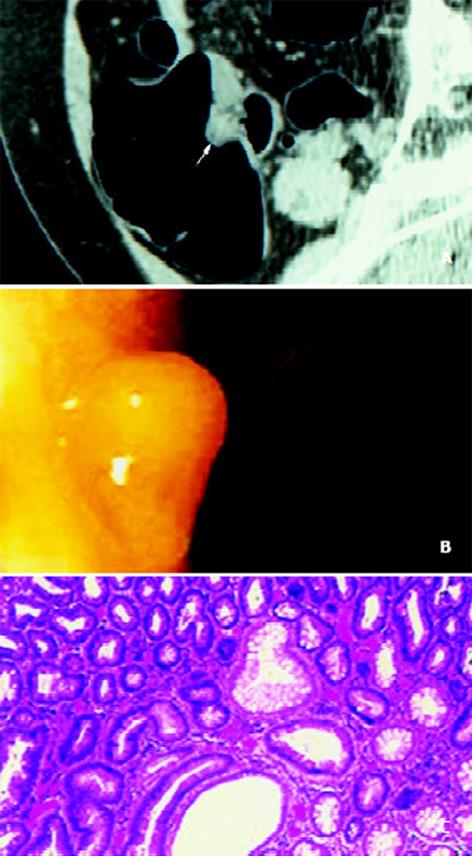
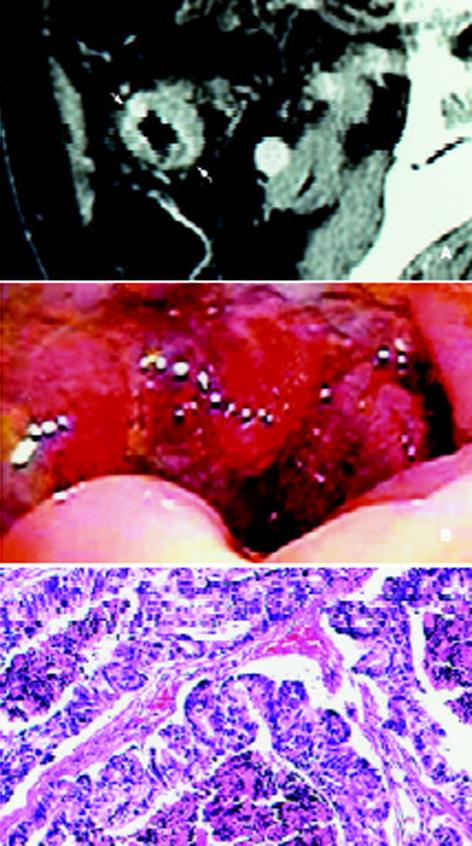
结肠充气CT检查100例中, 2例分别是乙状结肠和横结肠, 1为乙状结肠和降结肠, 另1例为乙状结肠、降结肠和横结肠未得到充盈. 该检查未发现任何并发症. 结肠镜检测出的36例大肠肿瘤(13例癌和46个息肉)中, 27例(13例大肠癌和14例患者的16个息肉)于结肠充气CT检查中得到检出(图1, 2), 结肠充气CT还检测出未被结肠镜发现的升结肠癌1例、假阳性乙状结肠癌1例和假阳性息肉2例(直径分别是7 mm和6 mm). 1例患者大肠癌与息肉合并发生, 结肠充气CT仅检出了大肠癌, 而遗漏了1个直径小于5 mm的息肉. 以结肠镜检查结果作为标准, 结肠充气CT对检测大肠肿瘤总的敏感性49% (95%CI: 44%-63%), 特异性91% (95%CI: 75%-98%). 结肠充气CT诊断大肠肿瘤15例, 其中13例是为结肠镜检出的侵袭性大肠癌, 1例为假阳性, 1例为结肠镜检查所漏诊. 结肠充气CT对于检测大肠癌的敏感性100%(95%CI: 75%-100%), 特异性93% (95%CI: 66%-100%). 对结果进一步分析还发现, 随着息肉直径的增加, 结肠充气CT对大肠息肉的检出率明显增大(1-5 mm, 2/21; 6-9 mm, 5/14; 大于或等于10 mm, 9/11), 并有统计学意义(P<0.05) (表1). 当越多直径越小的息肉列入计算, 结肠充气CT对大肠肿瘤检测的敏感性与特异性也随之而逐渐降低(大肠癌+直径大于或等于10 mm的息肉时, 敏感性92% (95%CI: 73%-99%), 特异性96% (95%CI: 78%-100%); 大肠癌+直径大于或等于6 mm的息肉时, 敏感性71%(95%CI: 54%-91%), 特异性90% (95%CI: 74%-98%); 大肠癌+所有息肉时, 敏感性49% (95%CI: 44%-63%), 特异性91%(95%CI: 75%-98%)(表1). 结肠充气CT对大肠息肉的检出率与其发生部位无关(右结肠, 1/5; 横结肠, 2/4; 左结肠, 4/13; 乙直肠9/24) (P>0.05). 另外结肠充气CT还发现6例其他病变, 包括脂肪肝3例, 大肠癌远处转移2例(肝转移1例, 癌性腹水1例)和可疑胰腺癌1例.
本研究表明, 虽然结肠充气CT对检测大肠肿瘤的总敏感性较低(49%, 95%CI: 44%-63%), 但对大肠癌的检测却有很高的敏感性和特异性, 另外结肠充气CT还可提供常规结肠镜不能获得的关于肿瘤局部浸润范围与远处转移等方面的信息, 且不需要特殊的软件, 检查时间也较短. 尽管如此, 其影像表现需要谨慎解释, 原因是: (1)大肠癌的实际发病率远远低于本研究的计算结果(14%); (2)要特别注意各种原因造成的假象, 如肥大的结肠袋襞, 肠管扩张不够等; (3)尽管本研究得出结肠充气CT对大检测肠癌100%的敏感性, 但是95%可信区间的下限(75%)不够理想.
临床上对直径1 cm以上大肠息肉的检测有重要的意义, 因为直径1 cm以下的息肉, 其恶变率较低(大约1%)[22-25]. 本研究表明, 结肠充气CT对息肉的检出率随其直径的增大而有意义地增高. 我们采用准直8 mm, 螺距1.5 mm, 重建间隔4 mm, 既有效地降低了放射线剂量, 又获得对直径大于或等于10 mm息肉及大肠癌92%的敏感性, 这一数值近似于以往学者采用更小准直和重建间隔及三维重建的研究结果(敏感性93%)[26-27]. 然而也有学者报道CT对直径10 mm以上息肉的检出率低, Rex et al[28]采用二维和三维CT结肠造影术研究了46例患者, 并对其中17例息肉患者进行了乙状结肠镜检查, 结果表明二维和三维CT结肠造影术对直径1 cm以上息肉的敏感性分别是29%和50%. Spinzi et al[29]采用准直5 mm, 螺距2 mm CT结肠造影术研究, 结果显示对直径1 cm以上息肉的敏感性为58%. 因此根据我们的结果可以推测, 结肠充气CT对10 mm以上息肉的检测可能优于CT结肠造影术.
结肠充气CT对直径10 mm以上息肉也有少部分漏诊, 可能是位置邻近直肠内Foley管、结肠内过多的粪渣和结肠未得到充分扩张. 因此检查前良好的肠道准备、采用更细的直肠Foley管和力求使结肠各段充分扩张可提高对10 mm以上大肠息肉的检出率. 必要时可进一步注气扩张肠管, 并重新定位后对部分结肠段进行二次扫描, 降结肠常常是未能扩张的肠段, 可采用仰卧位加俯卧位扫描, 尽管这些措施增加了放射线剂量, 但十分必要. 另外三维CT重建也许有助于进一步评价二维轴位扫描相上难以定性的病变[26-28]. 结肠CT极少有发现结肠外其他病变的报道, 我们采用腹部CT检查的标准毫安, 可成功地检测结肠及结肠外其他部位的病变, 因此改变了部分患者的治疗计划. 另外我们检出的所有大肠息肉中, 80%位于距离肛缘60 cm的大肠内, 是可曲性乙状结肠镜可以到达的范围[30-32], 可以推测将结肠充气CT与乙状结肠镜联合应用可检出大部分大肠息肉.
总之, 结肠充气CT对检测大肠癌和直径10 mm以上息肉有很高的敏感性和特异性, 但对直径10 mm以下大肠息肉的检出率低. 另外, 结肠充气CT还能够提供结肠镜不能发现的关于大肠癌分期和大肠外其他病变等信息, 具有重要的临床意义.
编辑: N/A
| 1. | Wan J, Zhang ZQ, Zhu C, Wang MW, Zhao DH, Fu YH, Zhang JP, Wang YH, Wu BY. Colonoscopic screening and follow-up for colorectal cancer in the elderly. World J Gastroenterol. 2002;8:267-269. [PubMed] |
| 2. | Makin GB, Breen DJ, Monson JR. The impact of new technology on surgery for colorectal cancer. World J Gastroenterol. 2001;7:612-621. [PubMed] |
| 3. | Han Y, Uno Y, Munakata A. Does flexible small-diameter colonoscope reduce insertion pain during colonoscopy? World J Gastroenterol. 2000;6:659-663. [PubMed] [DOI] |
| 11. | Sung JJ, Chan FK, Leung WK, Wu JC, Lau JY, Ching J, To KF, Lee YT, Luk YW, Kung NN. Screening for colorectal cancer in Chinese: comparison of fecal occult blood test, flexible sigmoidoscopy, and colonoscopy. Gastroenterology. 2003;124:608-614. [PubMed] [DOI] |
| 12. | Jung M, Beilenhoff U, Pietsch M, Kraft B, Rippin G. Standardized reprocessing of reusable colonoscopy biopsy forceps is effective: results of a German multicenter study. Endoscopy. 2003;35:197-202. [PubMed] [DOI] |
| 13. | Liangpunsakul S, Rex DK. Colon tumors and colonoscopy. Endoscopy. 2002;34:875-881. [PubMed] [DOI] |
| 14. | Lewis JD, Ng K, Hung KE, Bilker WB, Berlin JA, Brensinger C, Rustgi AK. Detection of proximal adenomatous polyps with screening sigmoidoscopy: a systematic review and meta-analysis of screening colonoscopy. Arch Intern Med. 2003;163:413-420. [PubMed] [DOI] |
| 18. | Miao YM, Amin Z, Healy J, Burn P, Murugan N, Westaby D, Allen-Mersh TG. A prospective single centre study comparing computed tomography pneumocolon against colonoscopy in the detection of colorectal neoplasms. Gut. 2000;47:832-837. [PubMed] [DOI] |
| 19. | Sosna J, Morrin MM, Kruskal JB, Farrell RJ, Nasser I, Raptopoulos V. Colorectal neoplasms: role of intravenous contrast-enhanced CT colonography. Radiology. 2003;228:152-156. [PubMed] [DOI] |
| 20. | Harvey CJ, Renfrew I, Taylor S, Gillams AR, Lees WR. Spiral CT pneumocolon: applications, status and limitations. Eur Radiol. 2001;11:1612-1625. [PubMed] [DOI] |
| 21. | Yong AA, Harris JE, Shorvon PJ. The value of prone imaging in CT pneumocolon. Clin Radiol. 2000;55:959-963. [PubMed] [DOI] |
| 22. | Calvert PM, Frucht H. The genetics of colorectal cancer. Ann Intern Med. 2002;137:603-612. [PubMed] [DOI] |
| 23. | Anwar S, White J, Hall C, Farrell WE, Deakin M, Elder JB. Sporadic colorectal polyps: management options and guidelines. Scand J Gastroenterol. 1999;34:4-11. [PubMed] [DOI] |
| 24. | Deen KI, de Silva HJ. Colorectal polyps. Ceylon Med J. 1999;44:6-10. [PubMed] |
| 25. | Bond JH. Polyp guideline: diagnosis, treatment, and surveillance for patients with colorectal polyps. Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 2000;95:3053-3063. [PubMed] [DOI] |
| 26. | Yee J, Kumar NN, Hung RK, Akerkar GA, Kumar PR, Wall SD. Comparison of supine and prone scanning separately and in combination at CT colonography. Radiology. 2003;226:653-661. [PubMed] [DOI] |
| 28. | Rex DK, Vining D, Kopecky KK. An initial experience with screening for colon polyps using spiral CT with and without CT colography (virtual colonoscopy). Gastrointest Endosc. 1999;50:309-313. [PubMed] [DOI] |
| 29. | Spinzi G, Belloni G, Martegani A, Sangiovanni A, Del Favero C, Minoli G. Computed tomographic colonography and conventional colonoscopy for colon diseases: a prospective, blinded study. Am J Gastroenterol. 2001;96:394-400. [PubMed] [DOI] |
| 30. | O'Brien K, Sweeney BF Jr, Conger N, Fischer JR, Lang KA. Prevalence of proximal adenomas after an adenoma is found on flexible sigmoidoscopy. Cancer Detect Prev. 2003;27:259-265. [PubMed] [DOI] |
| 31. | Patel K, Hoffman NE. The anatomical distribution of colorectal polyps at colonoscopy. J Clin Gastroenterol. 2001;33:222-225. [PubMed] [DOI] |
| 32. | Farraye FA, Wallace M. Clinical significance of small polyps found during screening with flexible sigmoidoscopy. Gastrointest Endosc Clin N Am. 2002;12:41-51. [PubMed] [DOI] |