INTRODUCTION
Irritable bowel syndrome (IBS) is the most common disorder seen in gastroenterological practice[1,2]. The disorder affects approximately 15% to 20% of the world's population and is predominately found in women[2]. It comprises a group of functional bowel disorders in which abdominal discomfort or pain is associated with defecation or a change in bowel habit, and with features of disordered defecation[3,4]. The pathophysiology of the symptom remains unclear, and visceral hypersensitivity or decreased pain thresholds to distension of the gut is considered to be a biologic marker for IBS and is present in most patients with this gastrointestinal disorder[5]. Possibly, there are dysfunctions in the processing of sensory stimuli in the "brain-gut" axis that may cause visceral hypersensitivity and secondary motility changes[6]. The central nervous system is believed to play a strong modulatory or etiological role in the pathophysiology of the disease[7].
In animals, the perception of somatovisceral pain is derived from the expression of the immediate early gene c-fos[8-11]. Numerous positron emission tomography (PET)[12-15] or functional magnetic resonance imaging (fMRI)[16-18] studies have dealt with the central processing of somatic pain in humans. In contrast, the neural networks involved in the perception of visceral pain in humans, especially rectal pain, have been the subjects of a limited number of functional brain imaging studies[19-23].
Previous studies of somatic pain using PET scanning to measure the regional cerebral blood flow have suggested that the anterior cingulate cortex (ACC), prefrontal cortex (PFC), insular cortex (IC), and thalamus (THAL) are important loci in pain perception[12,24]. Studies of visceral pain have generally suggested that these brain centers are important in sensation. fMRI is an alternative technique to measure changes in regional cerebral activity during stimulation. Using fMRI, the cerebral loci activated by rectal distention were also characterized in healthy volunteers[22].
In this study, we examined the effect of rectal balloon-distention stimulus by blood oxygenation level-dependent functional magnetic resonance imaging (BOLD-fMRI) in the visceral pain center and to compare the distribution, extent, and intensity of activated areas between irritable bowel Syndrome (IBS) patients and normal controls.
MATERIALS AND METHODS
Subjects
Eleven normal right-handed control subjects (6 men and 5 women; age, 24-49 years; average age, 39 years) and twenty-six right-handed patients with IBS (12 men and 14 women; age, 18-61 years; average age, 47 years) participated in the study. All volunteers were free of any gastrointestinal complaint. The IBS patients were all diagnosed in Ruijin Hospital, and met the Rome II criteria for IBS[4], which include at least 12 wk, not necessarily to be consecutive in the preceding 12 mo of abdominal discomfort or pain that has two of the following three features: (1) Relieved with defecation; (2) Onset associated with a change in frequency of stool; (3) Onset associated with a change in form (appearance) of stool. Each patient underwent a basic evaluation to exclude organic disease including a history, physical examination, and colonoscopy.
Distention protocol
Subjects reclined on the magnetic resonance imaging (MRI) table with head resting on a beanbag saddle that reduced head motion. A plastic balloon (Medtronic Synectics, USA) was placed in rectum at 10-15 cm from the anal margin. First, the subjects were tested for the rectal sensation, including the thresholds for sensation of gas, defecation and pain. Second, subjects reported the subjective pain intensity at 90 mL and 120 mL rectal balloon-distention by using visual analogue scale (0 = no pain, 10 = unbearable pain). Then, fMRI scanning was begun. Subjects were instructed to expect 4 series of rectal stimuli. Each set of distention included 3 stimuli of the same volume lasting 30 s each, with a 30-second rest period in between. The balloon inflation and deflation for each stimulus required an average of 6 s. The baseline volume during the rest periods was 0 mL. The first series of stimulus volume was 30 mL, the second 60 mL, the third 90 mL, and the last 120 mL.
MRI scanning
BOLD imaging was performed on a 1.5-T GE Signa MRI system. Each scanning consisted of a T1-weighted (the parameters included TR/TE = 400 ms/14 ms, matrix = 256 × 256, NEX = 1). Next, four 10-mm-thickslices aligned at an approximately 20o angle above the anterior commissure-posterior commissure line to include the ACC, IC, PFC, and THAL. A functional scan was performed using echo planar imaging, and a matrix of 64 × 64, NEX = 1. The pulse sequence parameters included a 90o flip-angle with a TR (image repetition rate)/TE (effective echo time) of 3000 ms/60 ms. Each run consisted of 3 repetitions of 30 s of rest, followed by 30 s of stimulus. In each 30-second period, 10 parameters were collected, 60 data during each series.
Data processing and analysis
Data analysis was performed using correlation-coefficient tool in Functional software (AW3.2, SUN workstation). The confidence level was 0.05. Brain areas thought to mediate painful sensation included the ACC, the IC, the PFC, and THAL. These regions of interest (ROI) were identified and circled on the high-resolution anatomic images by a radiologist, who was blind to the identity of the patient and to the active pixels. The regional cerebral activation was evaluated by the percentage area of ROI and the percentage change in MR signal intensity of ROI. The percentage area of ROI was calculated by the formula: the percentage area of ROI = the pixels of ROI/the total pixels of selected pain center × 100%. The percentage change in MR signal intensity of ROI = (the MR signal intensity during stimulation - the Mean baseline signal)/the mean baseline signal × 100%. The average percentage change in MR signal intensity was calculated for each subject at each stimulus volume in each ROI. To exclude the influence of balloon inflation and deflation, the first and the tenth MR signal intensity of the rest and stimulus phase were eliminated.
Statistical analysis
The data were expressed as means ± SEM. For comparison of means, an unpaired Student's t test was used. The primary comparisons were the thresholds for sensation and VAS score between IBS patients and controls. Secondary analysis included the percentage of ROI and the average percentage change in MR signal intensity of ROI comparing IBS patients with controls. Statistically significant differences by 2-tailed t tests were defined by P < 0.05.
RESULTS
Rectal sensation test
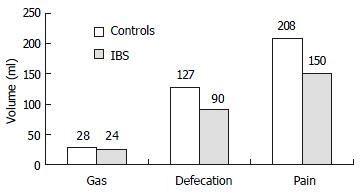
In the control group, the average thresholds for sensation of gas, defecation and pain were 28 mL, 127 mL, and 208 mL. They were 24 mL, 90 mL, and 150 mL respectively in IBS group. The thresholds for sensation of defecation and pain were significantly lower in IBS group than in control group (P < 0.05, Figure 1).
Figure 1 Rectal sensation test (the thresholds for sensation).
VAS score
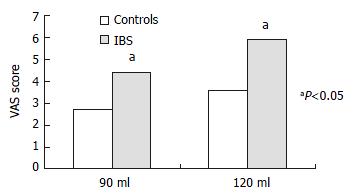
At 30 mL rectal distention, subjects generally sensed a very-low-intensity stimulation, using the terms "gas", "mildly felt". At 60 mL rectal distention, some IBS patients expressed sensation of defecation. At 90 mL rectal distention, a large number of IBS patients and some normal controls expressed sensation of stool, associated with mild-moderate pain, and VAS score was 4.42 ± 2.00 vs 2.71 ± 1.78. At 120 mL rectal distention, most IBS patients reported moderate-severe painful sensation, and VAS score was 5.90 ± 1.84 vs 3.95 ± 2.04. In this study, three IBS patients could not tolerate 120 mL rectal distention. The VAS score of 90 mL and 120 mL rectal distention (painful rectal distention) was significantly higher in IBS patients than in control (P < 0.05, Figure 2).
Figure 2 Subjective pain intensity.
Functional brain imaging
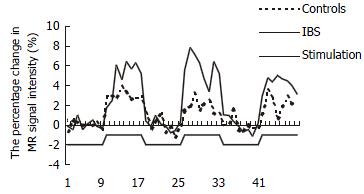
The time course of rectal stimulation sensation center response indicated immediate increase and rapid decline in BOLD signal in parallel with the mechanical distending stimulus (Figure 3). For both IBS patients and control subjects, rectal distention stimulation increased the activity of anterior cingulate cortex (35/37), insular cortex (37/37), prefrontal cortex (37/37), and thalamus (35/37) in most cases.
Figure 3 The percentage change in MR signal intensity time course of PFC in response to 3 rectal distentions at 90 mL.
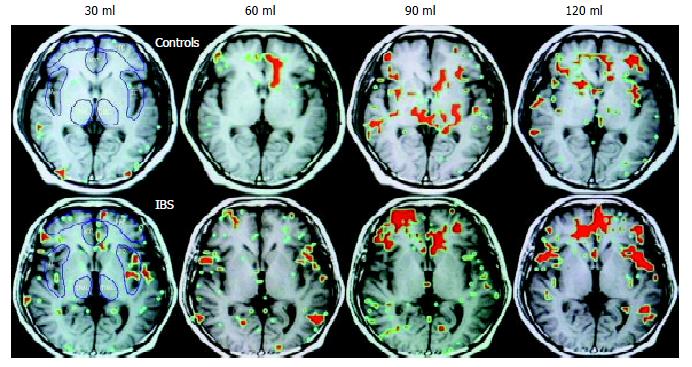
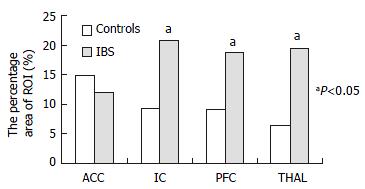
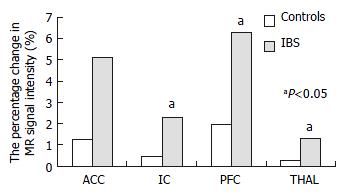
In patients with IBS, the average percentage area of ROI increased in parallel with rectal distention volumes in the IC, PFC, and THAL, only that in PFC had statistical significance (P < 0.05). In controls, this increasing tendency only occurred in the ACC (Figure 4). At 120 mL rectal distention, the average percentage area of ROI and the average percentage change in MR signal intensity of ROI in the IC, PFC, and THAL were significantly greater in patients with IBS than in control subjects (P < 0.05, Figure 5 and Figure 6).
Figure 4 Functional brain map.
The red area is the ROI.
Figure 5 The average area of ROI at 120 mL rectal distention.
Figure 6 The percentage change in MR signal intensity of ROI at 120 mL rectal distention.
DISCUSSION
FMRI is a useful technology to measure changes in regional CNS blood oxygenation, which is in parallel with regional metabolic activity[25-27]. The BOLD technology detects changes in the ratio of deoxyhemoglobin to oxyhemoglobin. When brain-center neurons are metabolically active, there is an increase in local blood flow and a relative increase in the amount of oxyhemoglobin, and an increase in magnetic resonance signal[25-29]. Accordingly, the magnetic resonance signal in a given pixel will increase above baseline if the region is activated in response to stimulation. FMRI offers advantages over PET such as direct anatomic correlation, avoidance of radioisotopes, and acceptable signal-to-noise ratio that do not require large numbers of stimuli. fMRI images give similar results as PET[30,31].
It showed that fMRI has adequate sensitivity to measure regional cerebral blood flow changes in response to visceral - in this case rectal - stimulation. Activity in the 4 selected CNS pain centers, ACC, IC, PFC, and THAL, promptly increase with rectal distention stimulation. The 4 selected pain centers are components of the brain's pain-processing system[12,24,32,33]. Current studies pointed to the THAL as a relay center, connecting afferent signals from the spinothalamic tract and spinoreticular tracts to higher centers such as the cingulate, prefrontal, and insular cortices[34,35]. The IC is believed to mediate primarily visceral sensations (taste, smell, gastric, colonic, and other visceral inputs) including rectal stimuli, whereas the ACC is thought to mediate the affective or "emotional" content of sensory information. The insular cortex neurons distributed between the taste area and the visceral area receive convergent inputs from baroreceptor, chemoreceptor, gustatory and nociceptive organs and may have roles in taste aversion or in regulation of visceral responses[36]. Using positron emission tomography (PET), Craig's[37] group found contralateral activity correlated with graded cooling stimuli only in the dorsal margin of the middle/posterior insula in humans. Furthermore, Krushel[38] referred to the region of convergence in the agranular insular cortex as the visceral cortex, and suggested its involvement in the efficient integration of specific visceral sensory stimuli with correlated limbic or motivational consequences. The visceral cortex may help regulate the organism's visceral response to stress.
The PFC is thought to exert higher executive functions in pain perception[39]. There are several different functional divisions of the PFC, including the dorsolateral, ventromedial, and orbital sectors. Each of these regions plays some role in affective processing that shares the feature of representing affect in the absence of immediate rewards and punishments as well as in different aspects of emotional regulation[40].
In this study, the thresholds for sensation of defecation and pain were significantly lower in IBS group than in control group, and VAS score was significantly higher in IBS patients than in controls. The results were similar to the previous studies[41]. Normal volunteers and IBS patients had significant cerebral activation in the 4 selected brain centers (ACC, IC, PFC, and THAL) during distention stimulation at 30 mL, 60 mL, 90 mL, and 120 mL. Significant differences in cerebral activation (both the percentage area and the percentage change in MR signal intensity of ROI) were found between IBS patients and controls. In IBS patients, there was significantly greater area of ROI of the PFC with 120 mL distention than with other volume distention. Conversely, in control subjects there was no significant increase in activation of these areas with 120 mL distention compared with others. Furthermore, at 120 mL rectal distention, there was significantly greater activation of the IC, PFC, and THAL in patients with IBS than in control subjects. In summary, by a variety of measures, it is possible that IC and PFC responses to visceral pain in IBS are greater than that in controls.
There were several studies about the CNS activity in response to visceral stimulation by using PET and fMRI, but the results differed. Silverman[20] found a lack of activation within the ACC or PFC with nonpainful stimuli, and reported activation of PFC in response to rectal pain only in IBS and the ACC only in normal subjects. In contrast, more recently Mertz[23], using fMRI, observed that pain led to a greater activation of the ACC than nonpainful stimuli. In Bernstein's[42] study, they also found that normal controls and subjects with IBD and IBS shared similar loci of activations to visceral sensations of stool and pain. A significantly higher percentage of pixels activated in the anterior cingulate gyrus over both pain and stool conditions for the control group than for the IBS group and for the IBS group than for the IBD group (P < 0.035). In another study, Bonaz et al[7] revealed significant deactivations within the right insula, the right amygdala, and the right striatum. There were gender differences in cortical representation of rectal distension in healthy humans. Male subjects showed localized clusters of fMRI activity primarily in the sensory and parietooccipital regions, whereas female subjects also showed activity in the anterior cingulate and insular regions[43]. Thus, somatic and visceral sensation including pain perception can be studied noninvasively in humans with functional brain imaging techniques. Positron emission tomography and functional magnetic resonance imaging have identified a series of cerebral regions involved in the processing of somatic pain, including the anterior cingulate, insular, prefrontal, inferior parietal, primary and secondary somatosensory, and primary motor and premotor cortices, the thalamus, hypothalamus, brain stem, and cerebellum[44]. Experimental evidence supports possible specific roles for individual structures in processing the various dimensions of pain[44].
In conclusion, our data conform that fMRI is an objective brain imaging technique to measure the change in regional cerebral activation exactly. Using fMRI, some patients with IBS could be detected having visceral hypersensitivity in response to painful rectal balloon-distention. In this study, IC and PFC of IBS patients are the major loci in CNS processing of visceral perception.