Published online Mar 15, 2003. doi: 10.3748/wjg.v9.i3.633
Revised: May 19, 2002
Accepted: June 11, 2002
Published online: March 15, 2003
We present here a large (3 cm) hyperplastic gastric polyp prolapsed into duodenum and caused outlet obstruction and iron deficiency anemia in 60 years old male patient. Endoscopic removal was performed successfully.
- Citation: Alper M, Akcan Y, Belenli O. Large pedinculated antral hyperplastic gastric polyp traversed the bulbus causing outlet obstruction and iron deficiency anemia: endoscopic removal. World J Gastroenterol 2003; 9(3): 633-634
- URL: https://www.wjgnet.com/1007-9327/full/v9/i3/633.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i3.633
In the literature, it is rarely to see the patients with gastric outlet obstruction due to prolapsing gastric polyps[1]. Inflammatory fibroid polyp of the gastrointestinal tract is the type most frequently reported[2]. We present here a large (3 cm) hyperplastic gastric polyp prolapsed into duodenum and caused outlet obstruction and iron deficiency anemia in 60 years old male patient. Endoscopic removal was performed successfully.
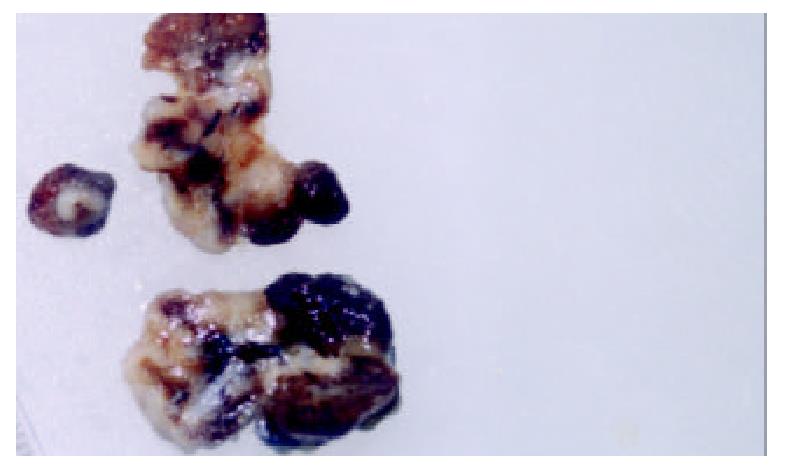
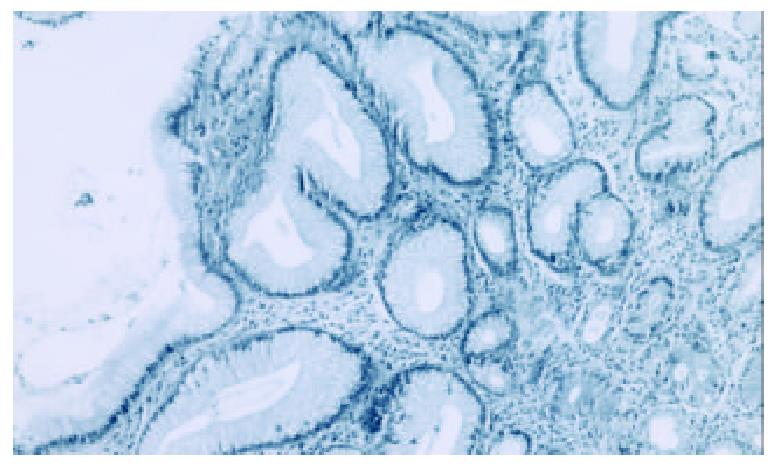
A 60 years old man was admitted to hospital due to severe fatigue, intermittent nausea and vomiting. Undigested food might have been seen in the vomitus. His hemoglobin was 7.6 gr/dl, MCV: 65 and serum iron level: 35 (low); iron binding capacity: 450 (high). All of aforementioned laboratory results indicated that the patient was suffering from iron deficiency anemia. Lower GIS barium enema examination and fiber sigmoidoscopy revealed no pathologic change. In upper endoscopy, initially we saw pyloric canal partially obstructed by a smooth surfaced pili-like structure. When passed to bulbus we observed a large polypoid mass. The biopsies taken were reported as hyperplastic gastric polyp. After re-evaluation of the endoscopic appearance by a second upper endoscopy, we thought that the pili-like structure traversing the pyloric canal might be a stalk of a polyp. Upon dragging the polyp with a controlled force, we were able to bring the polyp back to stomach. It was a pedinculated large antral polyp with a small area eroded on it, which was a possible explanation for blood loss. The polypectomy and removal was performed successfully in toto. The gross appearance (Figure 1) and microscopic examination (Figure 2) revealed a large hyperplastic polyp with no malignant component in any part. The patient who was regarded cured is under periodic endoscopic followed up. Clinically we transfused two bags of blood and later continued with iron supplementation therapy. Now, the patient is quite well with hemoglobin level of 13.5 gr/dl and has no signs of gastric outlet obstruction, freely consumes a normal diet.
Histologically, hyperplastic polyp is characterised by a markedly elongated foveolar region: the underlying glands are usually mucous glands. There is a marked lamina propria edema and inflammatory cell infiltration. The frequency of hyperplastic gastric polyps is reported between 1.3% and 28.3% in different series of upper gastrointestinal polypectomy[3,4]. Malignant transformation for hyperplastic polyps is small but the risk may be little bit higher if the polyp is more than 2 cm[5]. Among the gastric polyps causing outlet obstruction, fibroid polyps are relatively more frequent. Sporadic case reports with other histologic types are encountered like submucous lipoma[6]. To the best of our knowledge, there is no hyperplastic gastric polyp with a size of 3 cm originated in the antrum, crossed through the pylorus and captured in the bulbus. Rösch et al[7], by now, reported one case of hyperplastic polyp in duodenum formed as a heterotopia of gastric mucosa. But it was different from our case clinically and with respect to place of formation. In our patient, a 3-cm pedinculated polyp had formed in antrum, passed through the pylorus while it was small. Later, it presumably enlarged in bulbus so much that it was unable to go back to the stomach. We think so because we hardly take back it to the stomach through pylorus.
Gastric polyps may intussusept to duodenum causing gastric outlet obstruction. If the prolapsed polyp contains a functional antral mucosa over it, that mucosa may keep secreting gastrin due to being placed in the alkaline media of duodenum. In turn this hypergastrinemia may lead to erosion of the prolapsed polyp and blood loss[8]. Such an assumption could be valid in our case too.
Consequently, large prolapsed polyps can be dragged into stomach by easing the polypectomy procedure with a controlled force, instead of performing it in bulbus, which is a narrower space than stomach.
Edited by Zhang JZ
| 1. | Kumar A, Quick CR, Carr-Locke DL. Prolapsing gastric polyp, an unusual cause of gastric outlet obstruction: a review of the pathology and management of gastric polyps. Endoscopy. 1996;28:452-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Johnstone JM, Morson BC. Inflammatory fibroid polyp of the gastrointestinal tract. Histopathology. 1978;2:349-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 113] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Möckel W. [Hyperplasiogenic gastric polyps and stomach cancer. Endoscopic findings of early stomach cancer in 3 out of 42 biopsies of hyperplasiogenic polyps]. Fortschr Med. 1984;102:635-638. [PubMed] |
| 4. | Stolte M, Sticht T, Eidt S, Ebert D, Finkenzeller G. Frequency, location, and age and sex distribution of various types of gastric polyp. Endoscopy. 1994;26:659-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 135] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Gschwantler M, Pulgram T, Feichtenschlager T, Brownstone E, Gabriel C, Bibus B, Weiss W. Gastric carcinoma arising from a hyperplasiogenic polyp with a diameter of less than 2 centimeters. Z Gastroenterol. 1995;33:610-612. [PubMed] |
| 6. | Kallie NR, Peters JA. Submucous lipoma of the stomach: a case report. Can J Surg. 1976;19:42-45. [PubMed] |
| 7. | Rösch W, Höer PW. Hyperplasiogenic polyp in the duodenum. Endoscopy. 1983;15:117-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Brooks GS, Frost ES, Wesselhoeft C. Prolapsed hyperplastic gastric polyp causing gastric outlet obstruction, hypergastrinemia, and hematemesis in an infant. J Pediatr Surg. 1992;27:1537-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |