Published online Oct 15, 2003. doi: 10.3748/wjg.v9.i10.2236
Revised: July 25, 2003
Accepted: August 2, 2003
Published online: October 15, 2003
AIM: To analyze gastric polypoid lesions in our patient-population with respect to histopathologic features and demographic, clinical, and endoscopic characteristics of patients.
METHODS: Clinical records and histopathologic reports of patients with gastric polypoid lesions were analyzed retrospectively. All lesions had been totally removed by either endoscopic polypectomy or hot biopsy forceps. The histopathologic slides were re-evaluated by the same histopathologist.
RESULTS: One-hundred and fifty gastric polypoid lesions were identified in 91 patients. There were 53 (58%) women and 38 (42%) men with a median age of 53 (range, 31 to 82) years. The most frequent presenting symptom was dyspepsia that was observed in 35 (38.5%) patients. Symptoms were mostly related to various associated gastric abnormalities such as chronic gastritis or H pylori infection rather than polypoid lesion itself. Polypoid lesions were commonly located in the antrum followed by cardia. Out of 150 lesions, 80 (53%) had the largest dimensions less than or equal to 5 mm and only 7 were pedunculated. The frequencies of hyperplastic polyps, foveolar hyperplasia, and fundic gland polyps were 46%, 18%, and 14% respectively. We also detected gastritis varioliformis in 12 specimens, lymphoid follicles in 9, 4 adenomatous polyps in 4, polypoid lesions with edematous mucosa in 4, inflammatory polyps in 3, and carcinoid tumor in 1. Adenomatous changes were observed within two hyperplastic polyps and low grade dysplasia in one adenoma. Histopathologic evaluation of the surrounding gastric mucosa demonstrated chronic gastritis in 72 (79%) patients and H pylori infection in 45 (49%).
CONCLUSION: Hyperplastic polyps are the most frequently encountered subtype of gastric polypoid lesions. They are usually associated with chronic gastritis or H pylori gastritis. Contrary to the previous belief, they may harbour adenomatous changes or dysplastic foci. Therefore, endoscopic polypectomy seems as a safe and fast procedure for both diagnosis and treatment of gastric polypoid lesions at the same session. In addition, edematous mucosa may appear misleadingly as a polypoid lesion in some instances and it can be ruled out only by histopathologic examination.
- Citation: Gencosmanoglu R, Sen-Oran E, Kurtkaya-Yapicier O, Avsar E, Sav A, Tozun N. Gastric polypoid lesions: Analysis of 150 endoscopic polypectomy specimens from 91 patients. World J Gastroenterol 2003; 9(10): 2236-2239
- URL: https://www.wjgnet.com/1007-9327/full/v9/i10/2236.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i10.2236
The frequency of gastric polyps is gradually increasing due to widespread use of endoscopic examinations[1,2]. Any discrete lesion protruding into the lumen of gastrointestinal (GI) tract appeared at endoscopy is called as “polypoid lesion”[3]. However, a polyp is defined as a proliferative or neoplastic lesion of gastrointestinal mucosal layer[3]. Although endoscopic appearances of some polyps may be diagnostic, the term “polyp” should not be used for every discrete protrusions identified at endoscopy unless histopathologically confirmed[4,5]. According to the classification suggested by Oberhuber and Stolte[4], gastric polypoid lesions are divided into five distinct groups: non-neoplastic polyps such as hyperplastic polyp, hamartomatous polyps such as Peutz-Jeghers polyps, heterotopic tissue polyps such as heterotopic pancreas, neoplastic polyps such as adenoma, and reactive polypoid lesions such as foveolar hyperplasia. In their series, hyperplastic polyps and fundic gland polyps are the two most common subtypes of gastric polypoid lesions[4].
In this study, the demographic, clinical, and endoscopic characteristics of patients with gastric polypoid lesions were presented. The histopathologic features of these lesions were also reported and their malignancy potential is discussed.
Patients with gastric polypoid lesions detected by upper gastrointestinal endoscopy at the Institute of gastroenterology, Marmara University, between January 1998 and December 2002 were analyzed retrospectively. All gastroscopies were performed under sedation with intravenous midazolam and topical pharyngeal anesthesia with 10% lidocaine. The location, shape, size, and surface appearance of each polypoid lesion were assessed. Polypoid lesions were totally removed either by endoscopic polypectomy with an attempt or by hot biopsy forceps with multiple attempts according to their size. In addition, multiple biopsies were collected from both antrum and incisura angularis for Helicobacter pylori (H pylori) urease test and from surrounding gastric mucosa to detect any associated histopathologic changes such as chronic gastritis, H pylori infection, or intestinal metaplasia. Endoscopic records were screened for any complication resulted from polypectomy.
An experienced pathologist (O. K-Y.) re-evaluated all the tissue samples to confirm the histopathologic subclassification of gastric polypoid lesions in our series according to the classification suggested by Oberhuber and Stolte[4].
One hundred and fifty gastric polypoid lesions were identified in 91 consecutive patients from 2630 (3.4%) upper GI endoscopies. There were 53 (58%) women and 38 (42%) men with slightly female predominance (1.4:1). The ages of patients ranged from 31 to 82 years with a median of 53.
The most frequent presenting symptom was dyspepsia (38.5%) followed by epigastric pain (27.5%), and anemia (11%). Symptoms were usually related to the associated gastric abnormalities such as gastritis rather than polypoid lesion itself. Exceptionally, there was an antral hyperplastic polyp causing intermittent gastric outlet obstruction in one case in which the problem was solved with its removal by endoscopic polypectomy. The patient was symptom-free in the 8 months of follow-up.
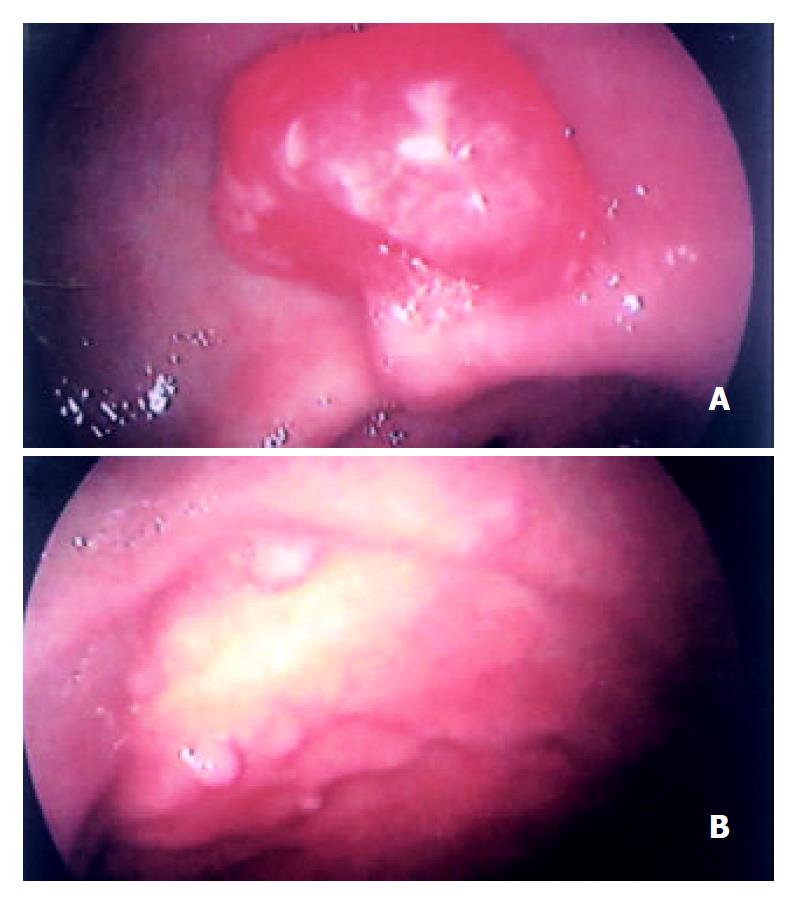
Characteristics of the gastric polypoid lesions are shown in Table 1. Out of 150 gastric polypoid lesions, 61 (40.6%) were located in the antrum followed by 40 (26.6%) in cardia, 34 (22.6%) in corpus, and 13 (8.6%) in fundus. In two patients who had previously undergone partial gastrectomy, the lesions were detected around anastomoses (1.2%). Only 7 out of 150 (4.6%) lesions were pedunculated (Figure 1A), while the remainder was sessile.
| Characteristics | Number* (%) |
| Location | |
| Antrum | 61 (40.7%) |
| Cardia | 40 (26.7%) |
| Corpus | 34 (22.7%) |
| Fundus | 13 (8.7%) |
| Peri-anastomotic | 2 (1.2%) |
| Shape | |
| Sessile | 143 (95.3%) |
| Pedunculated | 7 (4.7) |
| Size | |
| < 5 mm | 80 (53.4%) |
| 5-10 mm | 51 (34.0%) |
| 10-20 mm | 17 (11.4%) |
| 20-30 mm | 2 (1.2%) |
| Histologic subtypes | |
| Hyperplastic polyp | 69 (46.0%) |
| Foveolar hyperplasia | 27 (18.0%) |
| Fundic gland polyp | 21 (14.0%) |
| Gastritis varioliformis | 12 (8.0%) |
| Lymphoid follicles | 9 (6.0%) |
| Adenoma | 4 (2.7%) |
| Edematous mucosa | 4 (2.7%) |
| Inflammatory polyp | 3 (2.0%) |
| Carcinoid tumor | 1 (0.6%) |
Eighty (53%) gastric polypoid lesions with the largest dimensions less than or equal to 5 mm were totally removed by hot biopsy forceps. In the remainder, the largest dimension ranged from 6 to 30 mm and all lesions but one were excised by snare polypectomy. One lesion was initially evaluated by forceps biopsy because it was suspected to be a submucosal lesion. After a definite histopathologic diagnosis of carcinoid tumor was established in this patient, it was totally removed by snaring. Among 17 (11%) polypoid lesions with surface erosion, 5 were larger than 10 mm. Multiple lesions were detected in 29 (32%) patients (Figure 1B). No complication developed following the endoscopic procedure in any patient.
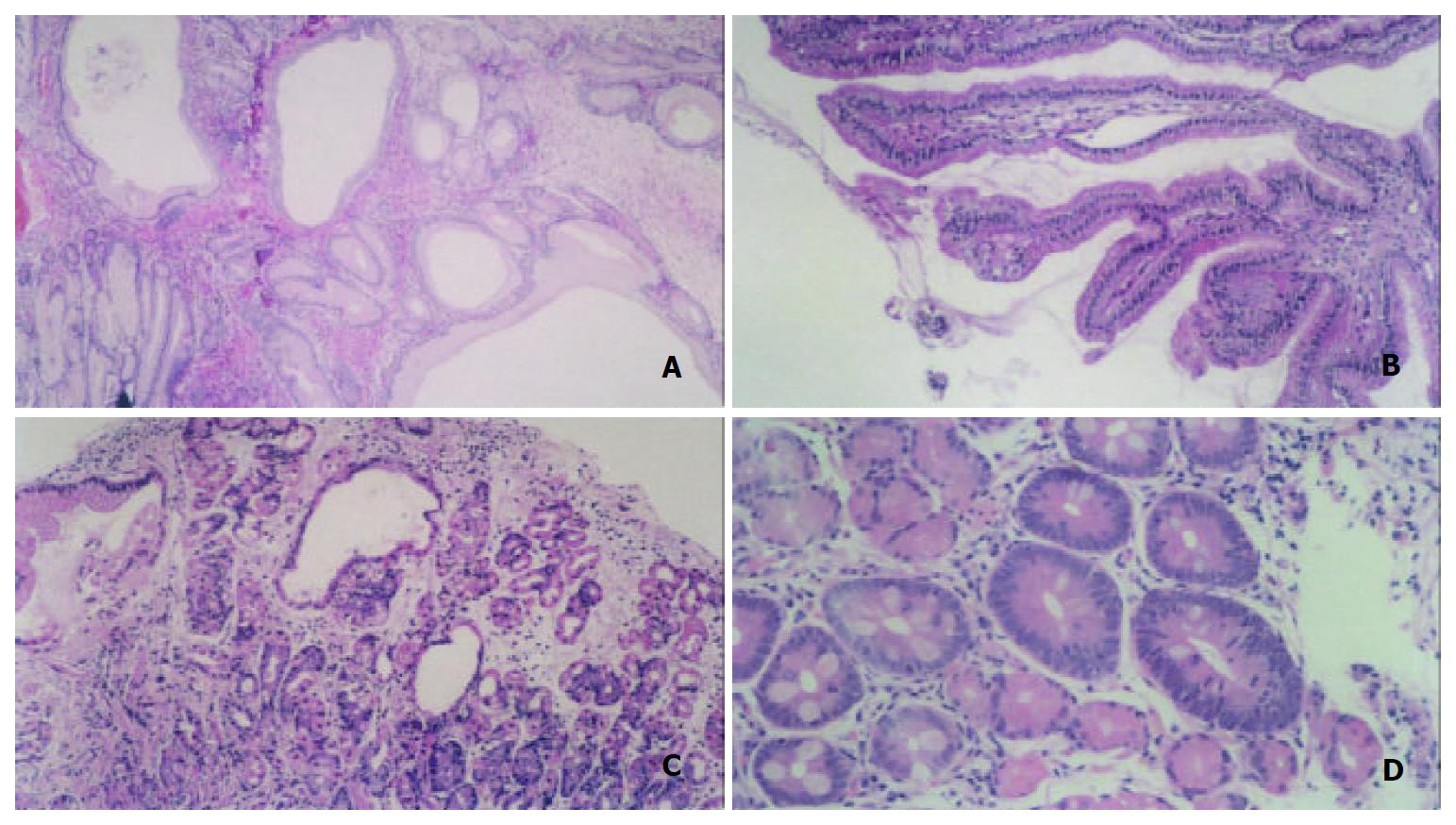
The most frequently encountered histopathologic subtype of gastric polypoid lesions was hyperplastic polyp (Figure 2A) which was diagnosed in 46% of the lesions, followed by foveolar hyperplasia (Figure 2B), fundic gland polyp (Figure 2C), and gastritis varioliformis (Table 2). Three of 43 patients with hyperplastic polyp had adenomas (Figure 2D) as well. Interestingly, the lesions ranging from 4 to 15 mm in diameter were observed as polypoid in 4 patients at endoscopy, but no pathologic changes except an edematous mucosa were determined in samples of endoscopic polypectomy. On the other hand, adenomatous changes were noted within two hyperplastic polyps. Out of 150 lesions, low grade dysplasia was found in one adenoma.
| Surrounding gastric mucosa | Type of Polyp | |||
| Hyperplastic | Fundic gland | Adenomatous | Inflammatory | |
| Normal | 10 | 3 | 1 | - |
| Chronic gastritis | 33 | 1 | 3 | 3 |
| H pylori gastritis | 19 | 1 | 1 | 1 |
| Intestinal metaplasia | 12 | - | 3 | 1 |
Evaluation of the surrounding gastric mucosa revealed that 72 (79%) patients had chronic gastritis, 45 (49%) associated H pylori infection, and 33 (36%) intestinal metaplasia, while the remainder (21%) had normal gastric mucosa (Table 2).
The average size of hyperplastic polyps was 8 mm in diameter. However, there was quite a large, hyperplastic polyp 30 mm in diameter, in one patient, and it caused gastric outlet obstruction by plugging the pyloric channel because of its antral location. They were preferentially located in the antrum (42%) and out of 69 hyperplastic polyps, 5 (7%) were pedunculated. Only fourteen patients (32%) had multiple hyperplastic polyps, while all the fundic gland polyps were multiple. Coexistent gastric abnormalities such as chronic gastritis, H pylori infection, and intestinal metaplasia were determined in 33 (77%), 19 (44%), and 12 (28%) patients, respectively.
The incidence of gastric polyps was 2% in 2630 patients who underwent upper GI endoscopic examination at our institution. Our rate was very similar to previously reported frequencies of 2%-3%[4]. However, the overall incidence of gastric polypoid lesions in our patient-population was 3.4%. Gastric polyps were usually seen as small and sessile polypoid lesions at endoscopy in patients over 40 years old[6]. Although a vast majority of gastric polyps were asymptomatic, they might cause epigastric pain, gastrointestinal bleeding, and symptoms of gastric outlet obstruction[6-8]. The complication risk was generally related to polyp size. We detected only two polyps larger than 2 cm in diameter in our series. A relationship between the presenting symptom and the polyp itself was observed only in one lesion as detailed above. Our results support the fact that underlying gastric abnormalities are likely to be responsible factors for presenting symptoms in patients with gastric polyps.
While polypectomy was performed either endoscopically or surgically in the treatment of symptomatic gastric polyps, there were still no standardized guidelines concerning the management of asymptomatic ones[5,9]. Many endoscopists first took forceps biopsies from gastric polypoid lesions. After obtaining a definite histopathologic diagnosis, they performed polypectomy to these lesions[5]. However, forceps biopsies carried the risk of missing the neoplastic foci within polyp, since only a small portion of the lesion was sampled in this technique[10]. Seifert and Elster[11] compared histopathologic results of biopsy materials and polypectomy specimens of same lesions and showed a remarkable discrepancy between them in 70% of cases. With this observation, the authors recommended to remove all gastric polyps larger than 5 mm in diameter by an experienced endoscopist[10,12]. In our study, all lesions except one, which was likely to be a submucosal lesion, were totally removed by either snare or hot biopsy forceps without any complication. Endoscopic polypectomy seems as a safe and fast procedure for both diagnosis and treatment of gastric polypoid lesions at the same session.
Some authors reported hyperplastic polyps or fundic gland polyps as the most frequently encountered subtypes of gastric polyps[13-16]. These lesions have previously been accepted as completely benign. However, some current studies showed that they might include adenomatous changes or dysplastic areas[4,7,13,17]. The reported frequencies of dysplastic foci within hyperplastic polyps showed a wide range (4%-22%)[18,19]. Hizawa[20] and Zea-Iriarte[21] found the incidence of malignancy in hyperplastic polyps was 2% and 1.8%, respectively. Since hyperplastic polyps were usually associated with chronic gastritis, particularly autoimmune gastritis and H pylori gastritis, patients with hyperplastic polyp had an increased risk of synchronous or metachronous adenocarcinomas elsewhere in the stomach[2,4,22]. In a series including 21 patients with hyperplastic polyps, chronic atrophic gastritis was found in all of them and H pylori gastritis in 16[16]. On the other hand, the rate of gastric cancer development in nonpolypoid mucosa was reported as 3.3% in another study of 2036 hyperplastic polyps[23]. In our series, the presence of chronic gastritis and H pylori gastritis was demonstrated in 76% and in 45% of hyperplastic polyps, respectively. In addition, two of 69 hyperplastic polyps contained adenomatous changes. These results support the suggestion of removing polypoid lesions instead of taking biopsy from them if feasible, when they are observed at endoscopy.
Gastric adenomas, similar to hyperplastic polyps, were usually detected in pathologically abnormal gastric mucosa such as gastritis or intestinal metaplasia[13,16]. The malignant potential of gastric adenomas was related to their histologic features, size, shape, and surface appearance[24]. While malignancy risk of adenomas smaller than 2 cm in diameter ranged from 1% to 5%, it was higher than 50% in larger ones[8]. The risk of gastric cancer in other parts of gastric mucosa in patients with adenoma varied between 8% and 59%[4]. Contrarily, fundic gland polyps were almost always associated with normal gastric mucosa and sometimes with long-term use of omeprazole[4,13]. They are divided into two different forms: sporadic form and syndromic form, which are associated with familial adenomatous polyposis (FAP) and attenuated variants. In a series including 319 fundic gland polyps from the John Hopkins Hospital, the FAP-associated polyps tended to include low grade dysplasia more than the sporadic ones (25% versus 1%)[25]. Furthermore, patients with fundic gland polyp might have an increased risk of harbouring a colorectal adenoma or carcinoma[4,23]. Nevertheless, prospective studies are necessary to ascertain whether fundic gland polyp is a sign for colorectal tumours or not. In our study, 75% of patients with adenoma had chronic gastritis and intestinal metaplasia, whilst gastritis was detected solely in one patient with fundic gland polyps.
Foveolar hyperplasia was the second most common type of gastric polypoid lesions in our series. There is still a debate on whether foveolar hyperplasia is a precursor of hyperplastic polyps[4,23]. The most important distinction between the two lesions was based on the presence of neoplastic foci. Orlowska and associates[26] analyzed 751 hyperplastic lesions and did not find carcinoma in any of foveolar hyperplasia either by primer biopsy or at follow-up. It is wise to separate foveolar hyperplasia and hyperplastic polyp from each other as two distinct subtypes of foveolar hyperplastic lesions, since foveolar hyperplasia has no malignant potential.
We determined that four lesions with polypoid appearance at endoscopy were actually areas of edematous mucosa by histopathological examination. This observation showed that a lesion protruding into the gastric lumen might appear as polypoid lesion even it was not a true polyp. In order to prevent diagnostic confusion, the term “polyp” should be used after achieving exact histopathologic diagnosis as well-supported by the above instance.
In summary, hyperplastic polyp is the most frequently encountered subtype of gastric polypoid lesions. It is usually associated with chronic gastritis or H pylori gastritis. Hyperplastic polyps have been described as harmless lesions until recently. However, risk of their malignant transformation has been emphasized in the current literature. For this reason, endoscopic polypectomy seems to be a sensible diagnostic and therapeutic procedure of hyperplastic polyps when feasible. Finally, endoscopic surveillance in these patients may be recommended to exclude both possibility of recurrence and cancer development elsewhere in stomach.
The authors thank Dr. Ilgin Ozden for contributing to the redaction of this article.
Edited by Wang XL
| 1. | Silverstein FE, Tytgat GNJ. Stomach II: Tumors and polyps. Gastrointestinal Endoscopy. 3rd ed. London: Mosby 1997; 147-180. |
| 2. | Dent TL, Kukora JS, Buinewicz BR. Endoscopic screening and surveillance for gastrointestinal malignancy. Surg Clin North Am. 1989;69:1205-1225. [PubMed] |
| 3. | Crawford JM. The gastrointestinal tract. Pathologic Basis of Disease. 6th ed. Philadelphia: W. B. Saunders Company 1999; 775-843. |
| 4. | Oberhuber G, Stolte M. Gastric polyps: an update of their pathology and biological significance. Virchows Arch. 2000;437:581-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 67] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 5. | Lau CF, Hui PK, Mak KL, Wong AM, Yee KS, Loo CK, Lam KM. Gastric polypoid lesions--illustrative cases and literature review. Am J Gastroenterol. 1998;93:2559-2564. [PubMed] |
| 6. | Sebastian MW. Benign tumors of stomach. The biological basis of modern surgical practise. 15th ed. Philadelphia: W.B. Saunders Company 1997; 868-875. |
| 7. | Dean PG, Davis PM, Nascimento AG, Farley DR. Hyperplastic gastric polyp causing progressive gastric outlet obstruction. Mayo Clin Proc. 1998;73:964-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Kumar A, Quick CR, Carr-Locke DL. Prolapsing gastric polyp, an unusual cause of gastric outlet obstruction: a review of the pathology and management of gastric polyps. Endoscopy. 1996;28:452-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Kudis V, Siegel E, Schilling D, Nüsse T, Bohrer MH, Riemann JF. [The hyperplastic gastric polyp - a praecancerosis?]. Z Gastroenterol. 2002;40:295-298. [PubMed] |
| 10. | Muehldorfer SM, Stolte M, Martus P, Hahn EG, Ell C. Diagnostic accuracy of forceps biopsy versus polypectomy for gastric polyps: a prospective multicentre study. Gut. 2002;50:465-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 98] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Seifert E, Elster K. Gastric polypectomy. Am J Gastroenterol. 1975;63:451-456. [PubMed] |
| 12. | Ginsberg GG, Al-Kawas FH, Fleischer DE, Reilly HF, Benjamin SB. Gastric polyps: relationship of size and histology to cancer risk. Am J Gastroenterol. 1996;91:714-717. [PubMed] |
| 13. | Debongnie JC. Gastric polyps. Acta Gastroenterol Belg. 1999;62:187-189. [PubMed] |
| 14. | Stolte M, Sticht T, Eidt S, Ebert D, Finkenzeller G. Frequency, location, and age and sex distribution of various types of gastric polyp. Endoscopy. 1994;26:659-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 136] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | Papa A, Cammarota G, Tursi A, Montalto M, Cuoco L, Certo M, Fedeli G, Gasbarrini G. Histologic types and surveillance of gastric polyps: a seven year clinico-pathological study. Hepatogastroenterology. 1998;45:579-582. [PubMed] |
| 16. | Ljubicić N, Kujundzić M, Roić G, Banić M, Cupić H, Doko M, Zovak M. Benign epithelial gastric polyps--frequency, location, and age and sex distribution. Coll Antropol. 2002;26:55-60. [PubMed] |
| 17. | Declich P, Ambrosiani L, Grassini R, Tavani E, Bellone S, Bortoli A, Gozzini C, Prada A. Fundic gland polyps: a still elusive entity on the eve of the year 2000. Pol J Pathol. 2000;51:3-8. [PubMed] |
| 18. | Daibo M, Itabashi M, Hirota T. Malignant trasformation of gas-tric hyperplastic polyps. Am J Gastroenterol. 1990;85:327-328. |
| 19. | Davaris P, Petraki K, Archimandritis A, Haritopoulos N, Papacharalampous N. Mucosal hyperplastic polyps of the stomach. Do they have any potential to malignancy? Pathol Res Pract. 1986;181:385-389. [PubMed] |
| 20. | Hizawa K, Fuchigami T, Iida M, Aoyagi K, Iwashita A, Daimaru Y, Fujishima M. Possible neoplastic transformation within gastric hyperplastic polyp. Application of endoscopic polypectomy. Surg Endosc. 1995;9:714-718. [PubMed] |
| 21. | Zea-Iriarte WL, Sekine I, Itsuno M, Makiyama K, Naito S, Nakayama T, Nishisawa-Takano JE, Hattori T. Carcinoma in gastric hyperplastic polyps. A phenotypic study. Dig Dis Sci. 1996;41:377-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 75] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Abraham SC, Singh VK, Yardley JH, Wu TT. Hyperplastic polyps of the stomach: associations with histologic patterns of gastritis and gastric atrophy. Am J Surg Pathol. 2001;25:500-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 117] [Article Influence: 4.9] [Reference Citation Analysis (1)] |
| 23. | Stolte M. Clinical consequences of the endoscopic diagnosis of gastric polyps. Endoscopy. 1995;27:32-37; discussion 59-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Park DI, Rhee PL, Kim JE, Hyun JG, Kim YH, Son HJ, Kim JJ, Paik SW, Rhee JC, Choi KW. Risk factors suggesting malignant transformation of gastric adenoma: univariate and multivariate analysis. Endoscopy. 2001;33:501-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Wu TT, Kornacki S, Rashid A, Yardley JH, Hamilton SR. Dysplasia and dysregulation of proliferation in foveolar and surface epithelia of fundic gland polyps from patients with familial adenomatous polyposis. Am J Surg Pathol. 1998;22:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 96] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 26. | Orlowska J, Jarosz D, Pachlewski J, Butruk E. Malignant transformation of benign epithelial gastric polyps. Am J Gastroenterol. 1995;90:2152-2159. [PubMed] |