Published online May 21, 2025. doi: 10.3748/wjg.v31.i19.101913
Revised: March 18, 2025
Accepted: April 17, 2025
Published online: May 21, 2025
Processing time: 232 Days and 12.8 Hours
Endoscopic bilateral biliary drainage is a first line palliative treatment for unre
To evaluate a possible superiority of simultaneous “side by side” (SBS) biliary drainage in unresectable MHBO.
We identified 135 patients who benefited from bilateral drainage using uncovered self-expandable metallic stents between 2010 and 2023. Among them, 62 benefited from simultaneous SBS bilateral drainage between 2017 and 2023, and 73 bene
Technical success was significantly increased in simultaneous drainage compared with sequential drainage (94% vs 75%, P = 0.008). However, simultaneous SBS drainage and sequential SIS drainage had a similar technical success (94% vs 95%). We observed no differences regarding clinical success, procedure duration and recurrent biliary obstruction rate. Stent patency was shorter in the SIS group compared with the simultaneous group (103 days vs 144 days). Early adverse events were more frequent in the sequential group (31% vs 21%, P = 0.205), with no differences regarding SIS or SBS technique. Technical failure was associated with a higher rate of infectious fatal adverse events (9.5% vs 1.7%, P = 0.02). Reintervention after recurrent biliary obstruction seems to be more successful after using SBS rather than SIS techniques (83% vs 75%, P = 0.53).
Simultaneous SBS metallic stent placement using an ultra-thin delivery system was technically easier and as efficient as sequential bilateral stenting in unresectable MHBO to achieve bilateral drainage. The SIS procedure remains a good option in unresectable MHBO.
Core Tip: This retrospective study focused on the different drainage techniques using endoscopic retrograde cholangiopancreatography for malignant hilar biliary obstruction. It highlighted the benefits of parallel drainage, particularly when performed simultaneously using ultra-thin delivery devices. This resulted in a clear advantage in terms of technical success and reduced the risk of complications associated with technical failure, which was more frequently observed in the case of sequential drainage, especially in a “side by side” fashion.
- Citation: Guilmoteau T, Rouquette O, Buisson A, Cambier S, Abergel A, Poincloux L. Direct comparison of simultaneous and sequential endoscopic metallic bilateral stenting in malignant hilar biliary obstruction. World J Gastroenterol 2025; 31(19): 101913
- URL: https://www.wjgnet.com/1007-9327/full/v31/i19/101913.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i19.101913
Management of malignant hilar biliary obstruction (MHBO) remains a challenging situation. Most obstructions are unresectable due to the patient’s general condition or local/metastatic tumor extent[1]. The latest guidelines recommend endoscopic biliary drainage as a first-line option, using preferentially uncovered metallic stents over plastic stents[2-6]. Bilateral drainage must be preferred to unilateral drainage in high-grade malignant hilar stricture because it provides a longer stent patency, with a lower reintervention rate for recurrent biliary obstruction (RBO) and similar clinical outcomes and adverse events (AEs)[7-10]. Drainage of at least 50% of total functional liver volume must be obtained[11].
Bilateral drainage can be performed using either “side by side” (SBS) or “stent in stent” (SIS) techniques, with no difference regarding technical and clinical success, stent patency, and survival[12,13]. Nevertheless, bilateral biliary drainage using metallic stents is still a technical challenge and includes many failed procedures even for a trained operator. Emergence of a new ultra-thin (6 Fr or smaller) delivery system enables simultaneous SBS metallic stent deploy
We investigated all patients who underwent bilateral biliary metallic stenting during endoscopic retrograde cholangiopancreatography (ERCP) for MHBO in Clermont-Ferrand University Hospital between January 1, 2010 and January 1, 2023. Conventional sequential SBS placement was performed at our institution between 2010 and 2017. Since 2017, simultaneous SBS placement has been performed on patients with unresectable MHBOs requiring bilateral drainage. The patient cohort was divided into those who underwent sequential SBS or SIS placement between 2010 and 2017 (sequential group) and those who underwent simultaneous SBS placement between 2017 and 2023 (simultaneous group). The two groups were compared retrospectively. Exclusion criteria included patients with no jaundice, resectable obstructions, minors, pregnancy, or patients concerned with limited judicial protection.
MHBO is confirmed after histological or cytological analysis [endoscopic ultrasound (EUS)-fine needle aspiration or fine needle biopsy, ERCP bile duct brushing, single-operator cholangioscopy system biopsy (SpyGlass®, Boston Scientific Corporation, United States) or percutaneous biopsy] when possible. Due to the mild diagnosis rentability of cytological brushing and the difficulties to obtain direct endoscopic biopsies in cholangiocarcinoma, histological/cytological proof was not systematically achieved. Thus, diagnosis was sometimes confirmed by a multidisciplinary team regarding medical history and biological and imaging findings. Unresectable status was assessed according to general medical condition and locoregional or metastatic extent after a medicosurgical multidisciplinary approach. The study was approved by our local Ethics Committee (IRB00013412, “CHU de Clermont Ferrand IRB #1”, IRB number 2023-CF003) with compliance to the French policy of individual data protection and was performed in accordance with the principles of the Declaration of Helsinki.
We retrospectively collected clinical data from patient charts including: Demographic information; type of procedure; type of stent and delivery-system catheter used; date of procedure; tumor type and biliary extent according to Bismuth and Corlette classification; procedure duration (in minutes); postoperative chemotherapy status; total bilirubin rate (μmol/L) at day 0 and day 7; early AE related to the procedure (day 0-day 7); late stent-related complications (RBO, i.e. stent patency and/or dysfunction); type and success of reintervention after RBO; and time until death or last follow-up.
All patients underwent sectional cross imaging (CT or magnetic resonance imagery) to evaluate hepatic volumetry and biliary extension of the MHBO and to assess surgical resectability. All procedures were performed by two ERCP-trained operators (> 2000 biliary stenting each) in an interventional endoscopy room equipped with fluoroscopy ad patients in dorsal decubitus position under general anesthesia after orotracheal intubation. Antibiotic prophylaxis was administered at the discretion of the anesthesiologist following the Société Française d’Anesthésie et de Réanimation recommendations[17]. Rectal nonsteroidal anti-inflammatory drugs (100 mg diclofenac or indomethacin) were administered based on the operator’s discretion. All procedures were performed using carbon dioxide insufflation with a 4.2 mm working channel duodenoscope (TJF-160® and TJF-190®, Olympus Medical Systems Corp., Tokyo, Japan). All patients underwent complete biliary sphincterotomy when deep biliary catheterization (either transpapillary or using the “double guidewire techni
Once deep biliary catheterization was achieved, multiple guidewires (0.035 inch straight or angle tip hydrophilic guide
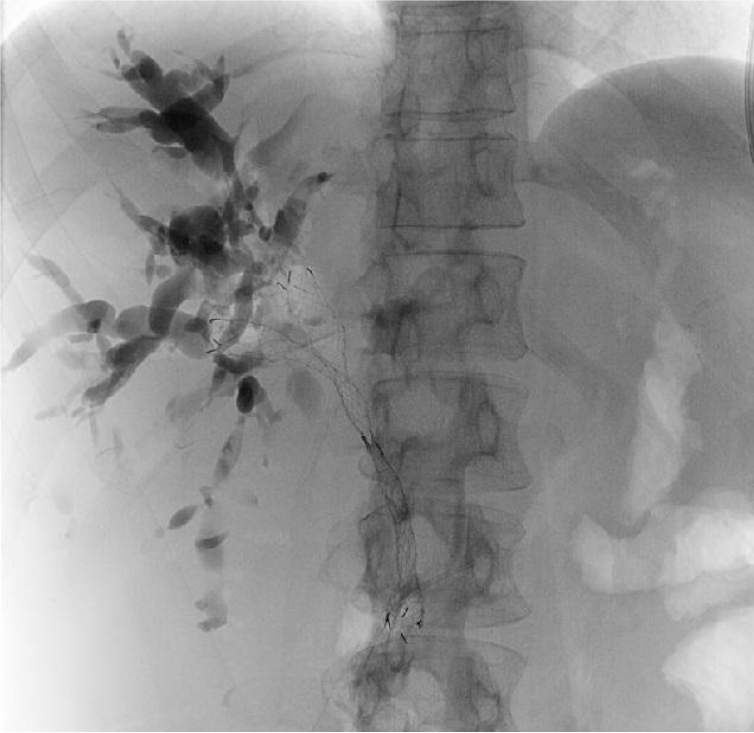
We used a Y-shaped stent with a wide wire mesh design (either M-Hilar Bonastent®, Mi-Tech, South Korea, or Y-Type Niti-S Stent®, Taewoong Medical, South Korea) to perform the SIS technique (or “through the mesh”). These stents have a thin delivery catheter of 7 Fr allowing to cross the wide wire mesh and an 8 mm diameter once they are deployed. For this technique, a bilateral guidewire catheterization is not mandatory. After deployment of the first stent across the hilar stricture, the guidewire left across the primary stent was carefully withdrawn, without pulling it back completely, and was then inserted into the undrained contralateral hepatic duct through the central wide mesh of the primary stent. Another uncovered SEMS was then introduced over the guidewire and deployed in the contralateral hepatic duct (Figure 1).
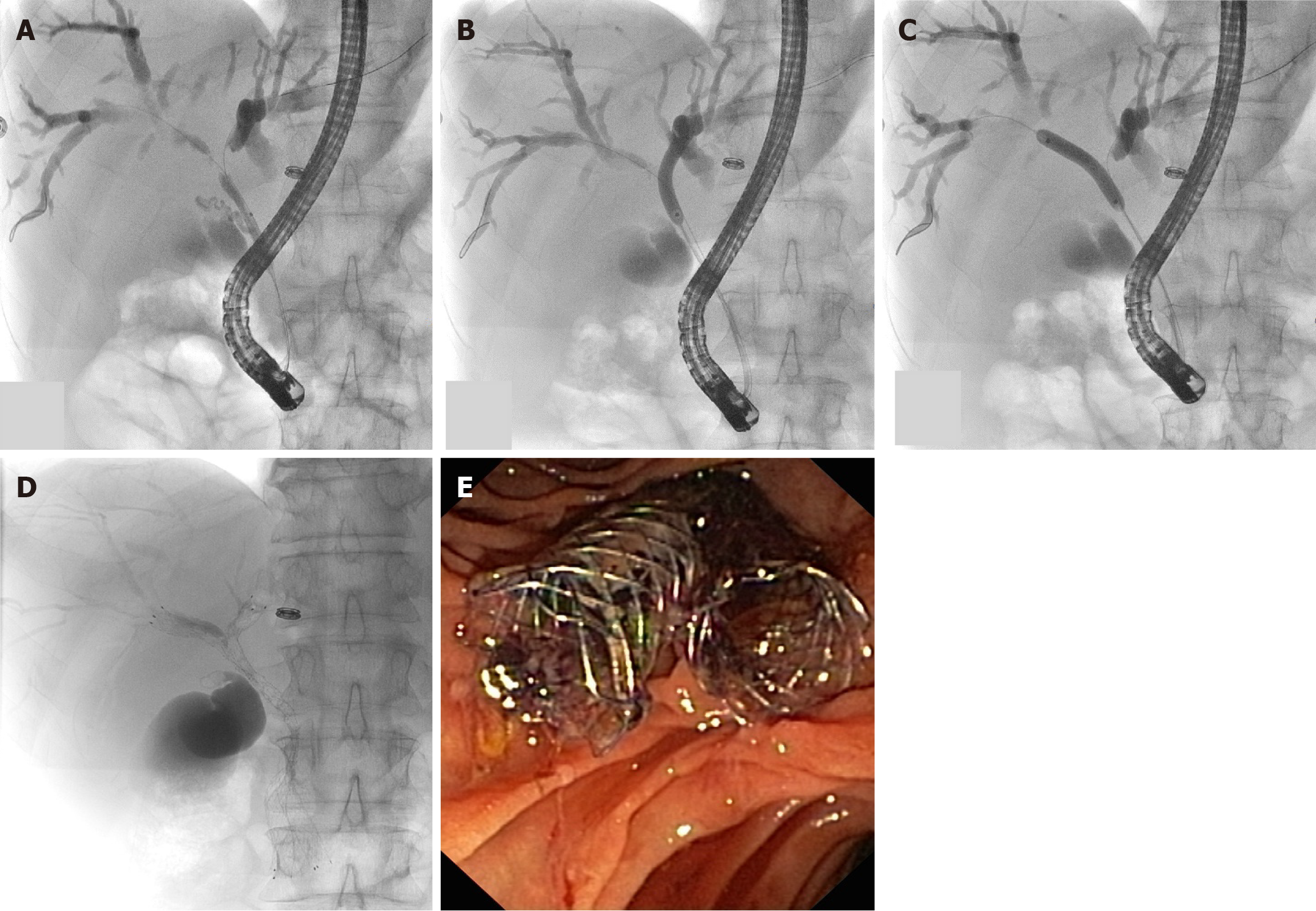
For this technique, we used SEMS with an ultra-thin delivery system that allowed simultaneous SBS bilateral hilar stenting achievement with a 4.2 mm working channel duodenoscope. First, a laser-cut SEMS aixstent® (Leufen Medical GmbH, Berlin, Germany) was carried by a 5 Fr delivery system from 2017 to 2020, and then the Niti-S M-Type® (Tae
The primary outcome for this study was to determine the technical success rate for each procedure (sequential or simul
Study data were collected and managed using REDCap electronic data capture tools hosted at the University Hospital of Clermont-Ferrand, France. Statistical analysis was performed using STATA 15 (Stata Corp LLC, TX, United States). Categorical variables were expressed as n (%). Continuous variables were expressed as mean or median and interquartile range. Group differences were evaluated using Fisher’s or χ2 tests for categorical variables. For continuous variables, group differences were evaluated using Wilcoxon’s, Mann-Whitney’s, or Kruskal-Wallis tests. Survival time was determined using the Kaplan-Meier method. Univariate and multivariate analyses were evaluated using the logistic regression model. Significance was defined as P < 0.05.
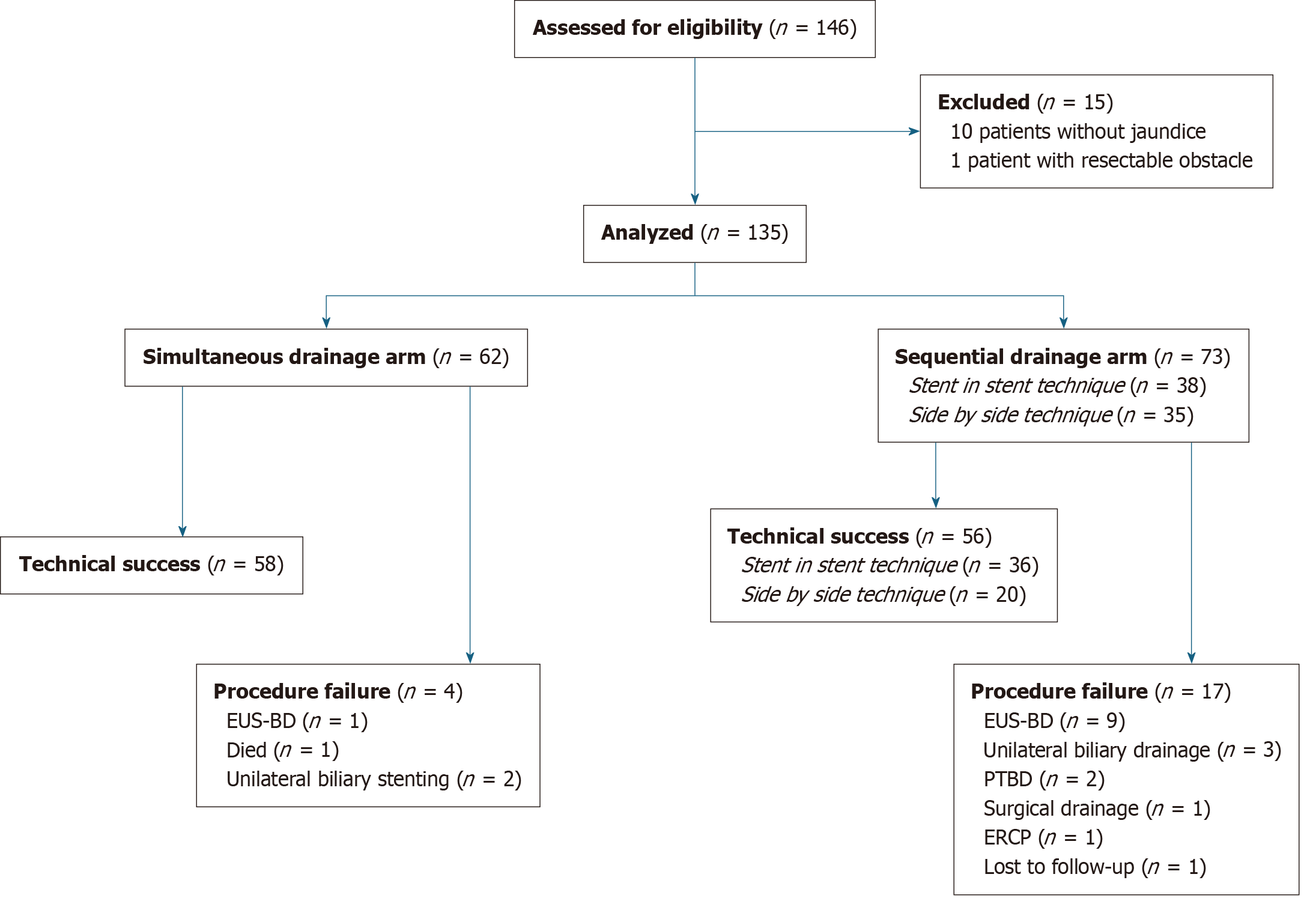
We identified 146 patients who benefited from bilateral drainage for MHBO between 2010 and 2023. Among them, 135 patients were included: 62 were treated with simultaneous bilateral drainage (between 2017 and 2023); and 73 were treated with sequential bilateral drainage (38 had SBS bilateral stent placement and 35 had SIS bilateral stent placement between 2010 and 2017). The flowchart of the study is presented in Figure 3. Patient characteristics were retrospectively collected and included age, sex, tumor type, Bismuth and Corlette classification of biliary extent, bilirubin rate at day 0, postoperative chemotherapy treatment status, and survival time. Results are presented in Table 1 and we observed no significant differences between the two groups.
| Characteristics | Sequential group, overall | Sequential group, side by side | Sequential group, stent in stent | Simultaneous group | P value |
| Number of patients | 73 | 35 | 38 | 62 | |
| Male | 41 (56) | 21 (51) | 20 (49) | 35 (56) | 0.82 |
| Age, years, median | 71 | 71 | 71 | 68 | 0.59 |
| Tumor type | 0.32 | ||||
| Cholangiocarcinoma | 34 (47) | 19 (54) | 15 (39) | 38 (61) | |
| Hilar metastasis | 34 (47) | 14 (40) | 20 (53) | 21 (34) | |
| Hepatocarcinoma | 5 (6) | 2 (6) | 3 (8) | 3 (5) | |
| Bismuth and Corlette classification | 0.053 | ||||
| II | 1 (1) | 0 (0) | 1 (2) | 8 (12) | |
| IIIa | 17 (23) | 11 (31) | 6 (16) | 9 (15) | |
| IIIb | 5 (7) | 2 (6) | 3 (8) | 9 (15) | |
| IV | 50 (69) | 22 (63) | 28 (74) | 36 (58) | |
| Bilirubin rate, day 0, μmol/L, median (IQR) | 224 (158-340) | 238 (162-342) | 220 (150-338) | 225 (132-334) | 0.80 |
| Postoperative chemotherapy | 25 (36) | 14 (42) | 11 (30) | 31 (53) | 0.095 |
| Survival time, days, median (IQR) | 61 (39-78) | 69 (43-128) | 43 (27-65) | 67 (56-105) | 0.24 |
Technical success was achieved in 94% of patients in the simultaneous group and in 77% of patients in the sequential group (P = 0.008). In the sequential group, technical success was more often achieved for the SIS technique (95%) than with the SBS technique (57%) (P = 0.001). A total of 58 patients underwent technical success in the simultaneous group: 21 using aixstent BDH® device (Leufen Medical GmbH, Berlin, Germany) and 37 using Niti-S M-Type® device (TaeWoong Medical, Seoul, Korea). We did not observe any significant difference in technical success between patients who had aixstent BDH or Niti-S stent implantation. Technical failure tended to be associated with a higher risk of death (hazard ratio: 1.35, P = 0.22). Baseline bilirubin rate did not appear to impact technical success. In the univariate and multivariate analysis, technical success was less frequent for Bismuth and Corlette IV type and metastatic hilar obstruction (Table 2). Patient outcomes are presented in Table 3.
| Variables | Univariate analysis, OR | Univariate analysis, 95%CI | Univariate analysis, P value | Multivariate analysis, OR | Multivariate analysis, 95%CI | Multivariate analysis, P value |
| Baseline bilirubin rate | 0.98 | 0.63-1.52 | 0.931 | 0.90 | 0.51-1.57 | 0.703 |
| Bismuth and Corlette type IV | 0.50 | 0.17-1.45 | 0.202 | 0.23 | 0.42-1.22 | 0.085 |
| Hilar metastasis | 0.45 | 0.17-1.19 | 0.106 | 0.27 | 0.06-1.10 | 0.068 |
| Patient outcomes | Sequential group, overall | Sequential group, side by side | Sequential group, stent in stent | Simultaneous group | P value |
| Technical success | 56 (77) | 58 (94) | 0.008 | ||
| 56 (77) | 20 (57) | 36 (95) | 58 (94) | 0.001 | |
| Clinical success (n = 101) | 33 (72) | 13 (76) | 20 (69) | 41 (75) | 0.82 |
| Procedure duration, minutes, median (IQR) | 80 (60-90) | 75 (35-93) | 80 (60-90) | 72 (58-99) | 0.75 |
| Early adverse event | |||||
| Overall | 23 (31) | 12 (34) | 11 (29) | 12 (21) | 0.39 |
| Pancreatitis | 8 (11) | 4 (11) | 4 (11) | 5 (8) | 0.81 |
| Cholangitis | 12 (16) | 6 (17) | 6 (16) | 4 (6) | 0.19 |
| Hemorrhage | 2 (3) | 1 (3) | 1 (3) | 4 (6) | 0.66 |
| Duodenal perforation | 1 (1) | 1 (3) | 0 (0) | 0 (0) | 0.26 |
| Recurrent biliary obstruction | 9 (18) | 1 (5) | 8 (20) | 13 (22) | 0.049 |
| Time to RBO, days, mean | 112 | 1821 | 103 | 144 | |
| Reintervention after RBO | 9 (100) | 1 (100) | 8 (100) | 11 (85) | 0.49 |
| Successful reintervention | 7 (78) | 1 (100) | 6 (75) | 9 (82) | 1 |
Clinical success was observed in 75% of patients in the simultaneous group and in 72% of patients in the sequential group. In the sequential group, there was no significant difference concerning clinical success between the SBS and SIS techniques (76% and 69%, respectively, P = 0.823).
Median procedure duration was 80 min in the sequential group and 72 min in the simultaneous group (P = 0.92), with no difference between sequential SBS and SIS techniques (75 and 80 minutes, respectively, P = 0.75).
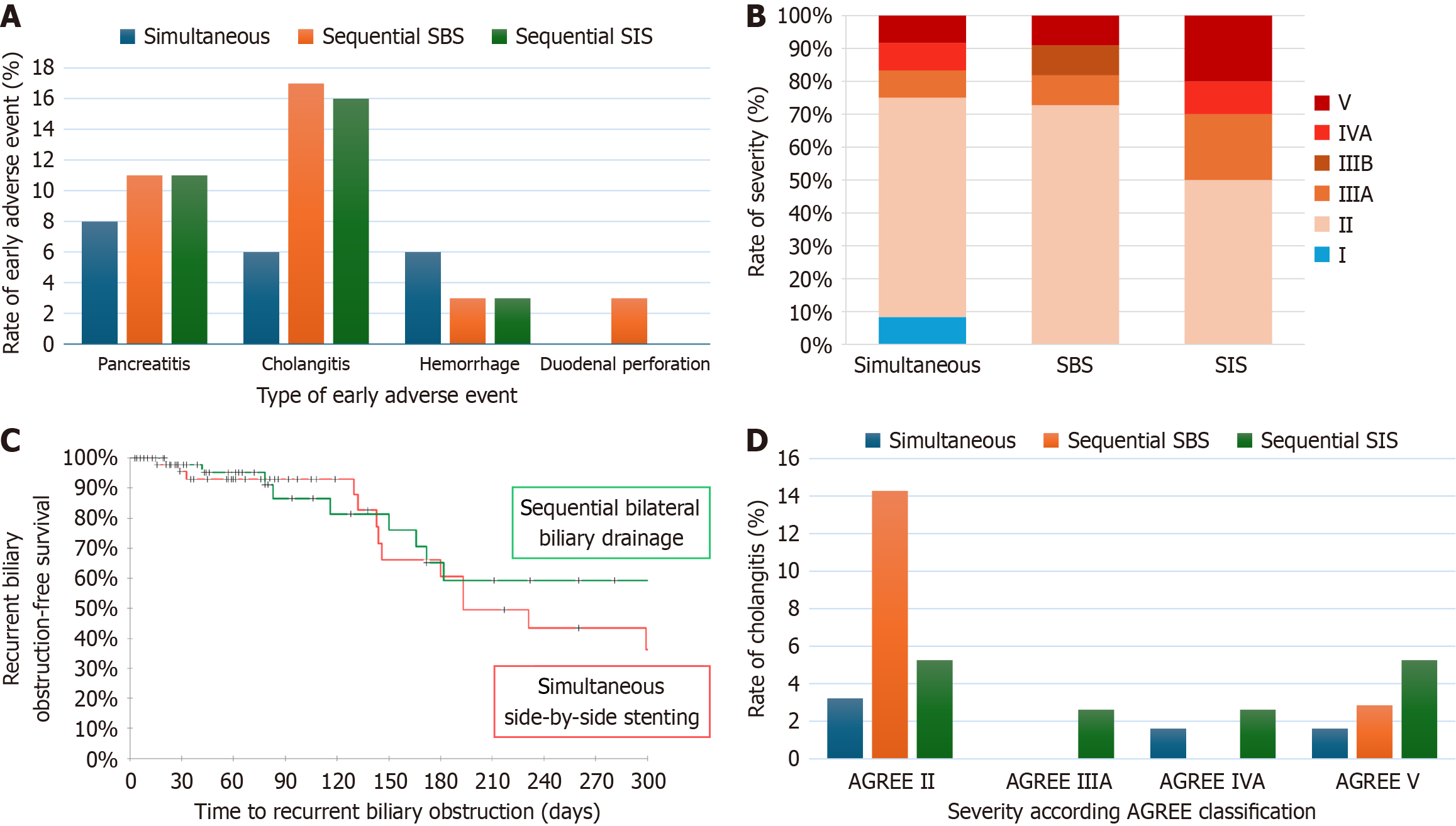
Overall, an early AE was observed in 31% of patients in the sequential group and 21% in the simultaneous group, with no significant difference (P = 0.205). Complication rates were similar between the SBS and SIS techniques in sequential group (34% and 29%, respectively, P = 0.39). Early AEs included 13 pancreatitis (no patient required intensive care unit admission or endoscopic/surgical intervention), 16 cholangitis (2 patients admitted in intensive care unit, 4 died), 6 hemorrhagic complications (due to sphincterotomy or iatrogenic duodenal ulcer, all medically managed), and 1 duodenal perforation occurred (in SBS sequential group, surgically managed). Cholangitis had a trend to be more frequently observed in the sequential group (16% vs 6%, P = 0.07), with no differences between the SBS or SIS techniques (17% and 16% respectively, P = 0.19). Early AE rates are represented in Figure 4A.
Most of the AEs were graded AGREE II (64% of overall AEs). We observed three fatal complications (AGREE V) in the sequential group and 1 fatal complication in the simultaneous group; both were infectious complications due to cho
Among patients with technical success, RBO was observed in 13 patients in the simultaneous group and 9 patients in the sequential group (22% and 18%, respectively). In the sequential group, RBO occurred in 1 patient (5%) in the SBS group and in 8 patients (20%) in the SIS group (P = 0.049). Mean time to RBO was 144 and 112 days in the simultaneous and sequential groups, respectively. Only 1 patient experienced RBO in the sequential SBS group after 182 days. Mean time to RBO in the sequential SIS group was 103 days. Using the Kaplan-Meier method among the patients with technical success, the risk of RBO was not different between the simultaneous and sequential groups (P = 0.39) (Figure 4C). After RBO, all patients underwent endoscopic reintervention, except 2 patients in the simultaneous group (15%, P = 0.49) who were not compatible with general anesthesia. Technical and clinical success were obtained in 82%, 75%, and 100% of cases in the simultaneous, sequential SIS, and SBS groups, respectively. Reintervention seemed to be more efficient when SBS bilateral drainage (either simultaneous or sequential) was performed compared with the SIS technique (83% vs 75%, P = 0.53).
We observed a median survival time of 67 days in the simultaneous group vs 61 days in the sequential group (69 days in the SBS group and 43 days in the SIS group). No significant difference was observed between groups (P = 0.24).
Complete biliary drainage in cases of unresectable MHBO frequently requires bilateral metallic drainage, a technically challenging endoscopic procedure. The emergence of SEMS associated to an ultra-thin delivery system such as aixstent® BDH (Leufen Medical GmbH, Berlin, Germany) carried by a 5 Fr delivery system and Niti-S M-Type® (TaeWoong Medical, Seoul, Korea) carried by a 6 Fr delivery system has been a true revolution in our practice by highly increasing technical success without impacting clinical outcomes or RBO rate compared with sequential stenting. Our study showed that simultaneous bilateral biliary drainage using a 6 Fr or 5 Fr delivery system was superior to sequential drainage when an SBS approach is chosen. Technical success was achieved in 94% of cases, a success rate that is similar with previous studies that evaluated feasibility of simultaneous SBS drainage, with a technical success ranging from 71% to 100%[14-16,19]. Our results concerning technical success of sequential SBS drainage are comparable with Inoue et al[14] (71% of technical success, P = 0.045). We also observed a high technical success rate of 95% for the SIS procedure and was comparable with previously existing literature (approximately 100%). Interestingly, we observed a higher rate of technical failure for patients who suffered hilar metastatic obstruction and for type IV of Bismuth and Corlette strictures. Baseline bilirubin rate did not appear to interfere with technical success or failure. A high technical success is important because it is closely related to the risk of post-procedure AE, particularly cholangitis, even though contrast agent injection in the non-catheterized liver segments was carefully avoided, whatever technique we used.
We reported a lower rate of early AE in the simultaneous group compared with the sequential group (21% vs 31%, P = 0.205). Cholangitis was observed more in the sequential group, with no difference between the SBS or SIS technique (Figure 4D). The higher rate of cholangitis in the sequential SBS group might be explained by the higher rate of technical failure. Concerning the sequential SIS group, the higher rate of cholangitis might be explained by the unilateral balloon dilatation of the bile duct before bilateral stenting or the difficulty of accurate positioning of the proximal tip of the crossing stent due to the frictional forces at the crossing point of the two stents. Recent meta-analysis evaluating SIS and SBS bilateral drainage found no differences in terms of AE between the two techniques (risk difference: -0.09, P = 0.07)[20], despite the fact that some authors suggest a higher rate of cholangitis with SBS techniques due to higher incidence of portal vein occlusion or obstruction of one of the two stents[21]. Use of thinner stents of 8 mm in simultaneous and sequential SIS groups probably contributed to lower the portal vein occlusion rate.
Technical failure was associated with a significantly higher rate of fatal cholangitis (OR 5.89, 0.78-44.4, P = 0.085), reminding us of the absolute necessity of adequate drainage of all opacified biliary areas, using if necessary in case of ERCP failure, alternative techniques such as percutaneous transhepatic biliary drainage (PTBD) or EUS-guided biliary drainage (EUS-BD). Furthermore, Vienne et al[11] proved that drainage of an atrophic biliary area is useless and im
We expected a shorter procedure time in the simultaneous group since Inoue et al[14] and Kawakubo et al[15] proved that simultaneous drainage shortens procedure time compared with sequential procedure (22 min and 25 min for simultaneous bilateral stenting in their study, respectively). In our study, the median procedure time was not different between the simultaneous and sequential procedures (80 min vs 72 min, P = 0.92). It was close to the simultaneous procedure time found by Chennat et al[19] and Law and Baron[15] (64 min and 75 min, respectively). We suffered from a lack of data concerning procedure duration. This is explained by the possibility for a same patient to benefit from both diagnostic EUS and therapeutic ERCP in the same procedure time. We excluded from procedure duration analysis all patient who benefited from the two procedures at the same time to not interfere with data of ERCP alone. Procedure time could sometimes include anesthetic induction and/or orotracheal extubation, which probably increased procedure time in our study.
Clinical success was defined in our study as a decrease of at least 50% of the bilirubin rate at day 7. Recent ESGE recommendations suggest that clinical success should be defined as a decrease of 50%-75% bilirubin rate after 2-4 weeks. We observed a similar clinical success rate (72% to 75%, P = 0.82) between the sequential and simultaneous group, a result that might be better with a different definition of clinical success, such as recommended by the ESGE[24]. Due to retro
We observed a shorter median survival time compared with other studies (61 days in the sequential group and 67 days in the simultaneous group in our study), especially in the sequential SIS group (43 days). In comparison, median survival time ranged from 146 days to 381 days in a meta-analysis by Chen et al[26] (five studies comparing SIS and SBS, 250 patients). This survival does not seem to be influenced by the stenting technique used but is rather a reflection of the severity of the underlying pathology, particularly in the SIS group where a slightly higher proportion of patients present with metastatic disease and have less access to postoperative chemotherapy.
That observation might also explain the lower RBO rate we observed in our study knowing that the usual RBO rate ranges from 18% to 53% in the studies that compared SIS and SBS, with a median stent patency of 118 days to 262 days, respectively[26]. Mean time to RBO was 144 days in the simultaneous group and 103 days in the SIS group. A difference that might be explained by the large cell mesh design of the stents used in the SIS technique, favoring tumor ingrowth[26,27]. Reintervention after RBO seems to be more successful with SBS stenting (sequential and simultaneous combined) than with SIS stenting (83% vs 75%, P = 0.53). This non-significant difference might be explained by the easier access to both distal tip of the stents with SBS drainage rather than with SIS techniques (two end-tip stents in the duodenal lumen with SBS technique vs one with SIS technique).
To date, this study was the largest concerning comparison of simultaneous and sequential bilateral biliary drainage. Patients were recruited over a large period of 13 years, and procedures were realized all along by only two trained operators. Most reinterventions for RBO proceeded in our tertiary center. The limits of this study were the single center retrospective design, with missing data affecting clinical success and procedure duration. It is important to note that the only study that compared simultaneous and sequential bilateral biliary drainage was also a retrospective monocentric study, with a smaller cohort of 34 patients[16]. Furthermore, due to a large recruitment period, technical success of the sequential technique might have been negatively impacted (procedures performed from 2010 to 2017 in comparison with the simultaneous technique performed from 2017 and 2023).
Endoscopic simultaneous bilateral metallic stenting using new SEMS with an ultra-thin (5 Fr or 6 Fr) delivery system is technically easier and as efficient as sequential bilateral stenting in unresectable MHBO to achieve bilateral drainage and can be useful to avoid the risk of a failed second stent placement. However, we reported a similar technical and clinical success in simultaneous SBS and sequential SIS groups with a higher rate of infectious complications in the sequential group even after successful SIS placement. Technical failure was significantly associated with fatal infectious complications. The RBO rate was similar in simultaneous and sequential SIS groups but with a shorter stent patency in the SIS group. We failed to show a difference in terms of procedure duration between the two techniques. Both simultaneous SBS and sequential SIS are valuable options for palliative endoscopic drainage in MHBO. However, the technical require
We dedicate this work to the memory of Professor Laurent Poincloux.
| 1. | Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BS J, Youssef BA M, Klimstra D, Blumgart LH. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234:507-17; discussion 517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 973] [Cited by in RCA: 963] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 2. | Dumonceau JM, Tringali A, Papanikolaou IS, Blero D, Mangiavillano B, Schmidt A, Vanbiervliet G, Costamagna G, Devière J, García-Cano J, Gyökeres T, Hassan C, Prat F, Siersema PD, van Hooft JE. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated October 2017. Endoscopy. 2018;50:910-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 529] [Cited by in RCA: 475] [Article Influence: 67.9] [Reference Citation Analysis (0)] |
| 3. | Rerknimitr R, Angsuwatcharakon P, Ratanachu-ek T, Khor CJ, Ponnudurai R, Moon JH, Seo DW, Pantongrag-Brown L, Sangchan A, Pisespongsa P, Akaraviputh T, Reddy ND, Maydeo A, Itoi T, Pausawasdi N, Punamiya S, Attasaranya S, Devereaux B, Ramchandani M, Goh KL; Asia-Pacific Working Group on Hepatobiliary Cancers. Asia-Pacific consensus recommendations for endoscopic and interventional management of hilar cholangiocarcinoma. J Gastroenterol Hepatol. 2013;28:593-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 186] [Article Influence: 15.5] [Reference Citation Analysis (1)] |
| 4. | Xia MX, Pan YL, Cai XB, Wu J, Gao DJ, Ye X, Wang TT, Hu B. Comparison of endoscopic bilateral metal stent drainage with plastic stents in the palliation of unresectable hilar biliary malignant strictures: Large multicenter study. Dig Endosc. 2021;33:179-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Sangchan A, Kongkasame W, Pugkhem A, Jenwitheesuk K, Mairiang P. Efficacy of metal and plastic stents in unresectable complex hilar cholangiocarcinoma: a randomized controlled trial. Gastrointest Endosc. 2012;76:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 166] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 6. | Mukai T, Yasuda I, Nakashima M, Doi S, Iwashita T, Iwata K, Kato T, Tomita E, Moriwaki H. Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. J Hepatobiliary Pancreat Sci. 2013;20:214-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 165] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 7. | Naitoh I, Ohara H, Nakazawa T, Ando T, Hayashi K, Okumura F, Okayama Y, Sano H, Kitajima Y, Hirai M, Ban T, Miyabe K, Ueno K, Yamashita H, Joh T. Unilateral versus bilateral endoscopic metal stenting for malignant hilar biliary obstruction. J Gastroenterol Hepatol. 2009;24:552-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 148] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 8. | Lee TH, Kim TH, Moon JH, Lee SH, Choi HJ, Hwangbo Y, Hyun JJ, Choi JH, Jeong S, Kim JH, Park DH, Han JH, Park SH. Bilateral versus unilateral placement of metal stents for inoperable high-grade malignant hilar biliary strictures: a multicenter, prospective, randomized study (with video). Gastrointest Endosc. 2017;86:817-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 132] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 9. | Aghaie Meybodi M, Shakoor D, Nanavati J, Ichkhanian Y, Vosoughi K, Brewer Gutierrez OI, Kalloo AN, Singh V, Kumbhari V, Ngamruengphong S, Khashab MA. Unilateral versus bilateral endoscopic stenting in patients with unresectable malignant hilar obstruction: a systematic review and meta-analysis. Endosc Int Open. 2020;8:E281-E290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Yang F, Wang XM, Xia FF, Han XQ. Endoscopic metal stenting for malignant hilar biliary obstruction: an update meta-analysis of unilateral versus bilateral stenting. Wideochir Inne Tech Maloinwazyjne. 2021;16:472-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Vienne A, Hobeika E, Gouya H, Lapidus N, Fritsch J, Choury AD, Chryssostalis A, Gaudric M, Pelletier G, Buffet C, Chaussade S, Prat F. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc. 2010;72:728-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 218] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 12. | Lee TH, Moon JH, Choi JH, Lee SH, Lee YN, Paik WH, Jang DK, Cho BW, Yang JK, Hwangbo Y, Park SH. Prospective comparison of endoscopic bilateral stent-in-stent versus stent-by-stent deployment for inoperable advanced malignant hilar biliary stricture. Gastrointest Endosc. 2019;90:222-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 13. | Naitoh I, Inoue T. Optimal endoscopic drainage strategy for unresectable malignant hilar biliary obstruction. Clin Endosc. 2023;56:135-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 14. | Inoue T, Ishii N, Kobayashi Y, Kitano R, Sakamoto K, Ohashi T, Nakade Y, Sumida Y, Ito K, Nakao H, Yoneda M. Simultaneous Versus Sequential Side-by-Side Bilateral Metal Stent Placement for Malignant Hilar Biliary Obstructions. Dig Dis Sci. 2017;62:2542-2549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Law R, Baron TH. Bilateral metal stents for hilar biliary obstruction using a 6Fr delivery system: outcomes following bilateral and side-by-side stent deployment. Dig Dis Sci. 2013;58:2667-2672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 16. | Kawakubo K, Kawakami H, Kuwatani M, Kudo T, Abe Y, Kawahata S, Kubo K, Kubota Y, Sakamoto N. Single-step simultaneous side-by-side placement of a self-expandable metallic stent with a 6-Fr delivery system for unresectable malignant hilar biliary obstruction: a feasibility study. J Hepatobiliary Pancreat Sci. 2015;22:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Martin C, Auboyer C, Boisson M, Dupont H, Gauzit R, Kitzis M, Leone M, Lepape A, Mimoz O, Montravers P, Pourriat JL; Steering committee of the French Society of Anaesthesia and Intensive Care Medicine (SFAR) responsible for the establishment of the guidelines. Antibioprophylaxis in surgery and interventional medicine (adult patients). Update 2017. Anaesth Crit Care Pain Med. 2019;38:549-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 18. | Nass KJ, Zwager LW, van der Vlugt M, Dekker E, Bossuyt PMM, Ravindran S, Thomas-Gibson S, Fockens P. Novel classification for adverse events in GI endoscopy: the AGREE classification. Gastrointest Endosc. 2022;95:1078-1085.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 151] [Article Influence: 50.3] [Reference Citation Analysis (0)] |
| 19. | Chennat J, Waxman I. Initial performance profile of a new 6F self-expanding metal stent for palliation of malignant hilar biliary obstruction. Gastrointest Endosc. 2010;72:632-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | de Souza GMV, Ribeiro IB, Funari MP, de Moura DTH, Scatimburgo MVCV, de Freitas Júnior JR, Sánchez-Luna SA, Baracat R, de Moura ETH, Bernardo WM, de Moura EGH. Endoscopic retrograde cholangiopancreatography drainage for palliation of malignant hilar biliary obstruction - stent-in-stent or side-by-side? A systematic review and meta-analysis. World J Hepatol. 2021;13:595-610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Naitoh I, Hayashi K, Nakazawa T, Okumura F, Miyabe K, Shimizu S, Yoshida M, Yamashita H, Ohara H, Joh T. Side-by-side versus stent-in-stent deployment in bilateral endoscopic metal stenting for malignant hilar biliary obstruction. Dig Dis Sci. 2012;57:3279-3285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 22. | Kongkam P, Orprayoon T, Boonmee C, Sodarat P, Seabmuangsai O, Wachiramatharuch C, Auan-Klin Y, Pham KC, Tasneem AA, Kerr SJ, Romano R, Jangsirikul S, Ridtitid W, Angsuwatcharakon P, Ratanachu-Ek T, Rerknimitr R. ERCP plus endoscopic ultrasound-guided biliary drainage versus percutaneous transhepatic biliary drainage for malignant hilar biliary obstruction: a multicenter observational open-label study. Endoscopy. 2021;53:55-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 23. | Vanella G, Bronswijk M, Maleux G, van Malenstein H, Laleman W, Van der Merwe S. EUS-guided intrahepatic biliary drainage: a large retrospective series and subgroup comparison between percutaneous drainage in hilar stenoses or postsurgical anatomy. Endosc Int Open. 2020;8:E1782-E1794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (1)] |
| 24. | van der Merwe SW, van Wanrooij RLJ, Bronswijk M, Everett S, Lakhtakia S, Rimbas M, Hucl T, Kunda R, Badaoui A, Law R, Arcidiacono PG, Larghi A, Giovannini M, Khashab MA, Binmoeller KF, Barthet M, Perez-Miranda M, van Hooft JE. Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022;54:185-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 273] [Article Influence: 91.0] [Reference Citation Analysis (3)] |
| 25. | Paik WH, Park YS, Hwang JH, Lee SH, Yoon CJ, Kang SG, Lee JK, Ryu JK, Kim YT, Yoon YB. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc. 2009;69:55-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 188] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 26. | Chen L, Gao GM, Li DL, Chen ZK. Side-by-side versus stent-in-stent bilateral stenting for malignant hilar biliary obstruction: a meta-analysis. Wideochir Inne Tech Maloinwazyjne. 2022;17:279-288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 27. | Heo JY, Lee HS, Son JH, Lee SH, Bang S. Clinical Outcomes of Bilateral Stent-in-Stent Placement Using Self-Expandable Metallic Stent for High-Grade Malignant Hilar Biliary Obstruction. Yonsei Med J. 2018;59:827-833. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |