Published online May 14, 2025. doi: 10.3748/wjg.v31.i18.105866
Revised: March 12, 2025
Accepted: March 26, 2025
Published online: May 14, 2025
Processing time: 94 Days and 1.3 Hours
In this article, we have commented on the article by Augustin et al. The authors presented a systematic review of the diagnosis, treatment, and outcomes of primary hyperparathyroidism-induced acute pancreatitis in pregnant women. Since acute pancreatitis during pregnancy could cause maternal as well as fetal adverse outcomes, understanding this pathology is essential. Although there are various etiologies of acute pancreatitis during pregnancy, primary hyperparathyroidism is one of the causes that complicate hypercalcemia. Along with con
Core Tip: Primary hyperparathyroidism-induced acute pancreatitis during pregnancy is a rare condition and can cause maternal and fetal adverse outcomes. Therefore, early diagnosis and appropriate therapeutic intervention are essential. This article comments on the recent systematic review of this condition published in the World Journal of Gastroenterology. In addition, multiple endocrine neoplasia screening is recommended for the better prognosis of the cases.
- Citation: Kamimura K, Terai S. Importance of understanding a diagnostic-treatment algorithm for primary hyperparathyroidism-induced acute pancreatitis during pregnancy. World J Gastroenterol 2025; 31(18): 105866
- URL: https://www.wjgnet.com/1007-9327/full/v31/i18/105866.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i18.105866
A recently published article authored by Augustin et al[1] presented a systematic review on primary hyperparathyroidism (PHPT)-induced acute pancreatitis in pregnant women. Various etiologies can induce acute pancreatitis; PHPT being one of the causes. Since acute pancreatitis in the pregnancy period could lead to maternal as well as fetal adverse outcomes, accurate diagnosis and appropriate treatment are crucial. Therefore, knowledge and understanding of the condition is very important. Since acute pancreatitis induced by hyperparathyroidism in the pregnancy period is a relatively rare condition, sufficient information has not been summarized in the literature to date. Hence, a systematic review of this pathology was necessary to establish diagnostic and treatment algorithms. Augustin et al[1] concluded that examining the serum calcium level is the key to early diagnosis and therapeutic intervention of PHPT-induced acute pancreatitis. Recently, the guidelines for the clinical practice to manage the PHPT have been published, as it involves multiple organs and is complicated with various symptoms[2-5]. In addition, approximately 10% of PHPT is associated with various syndromes and genetic diseases, such as multiple endocrine neoplasia type 1 (MEN1)[6,7]. MEN is an autosomal dominant inherited tumor syndrome that is characterized by multiple tumors affecting the parathyroid glands, pituitary glands, and pancreas. Therefore, further screening, including genetic diagnosis, might be beneficial for pregnant women and their babies for accurate prediction of additional tumor onset and other symptoms.
Although biliary tract stones and alcohol abuse are the major etiologies of acute pancreatitis, it can also be caused by hypertriglyceridemia, hypercalcemia, autoimmune diseases, endoscopic retrograde cholangiopancreatography, and trauma[8,9]. Among various factors that cause hypercalcemia, PHPT is reported to be associated with acute pancreatitis occurrence with approximately a 5%-6% rate[10]. Misgar et al[10] reviewed the records of 242 PHPT cases and reported that pancreatitis was the only presenting complaint, and PHPT screening was important for any patient with pancreatitis with high serum calcium levels, particularly when the other common etiologies of pancreatitis are present. The major pathology of PHPT-induced acute pancreatitis is the deposition of calcium in the pancreatic duct, thereby obstructing it. In addition, the direct toxic action of parathyroid hormone (PTH) and conversion of trypsinogen to trypsin triggers pancreatitis in individuals with PHPT[11,12]. Early diagnosis and management of PHPT is important since it can cause various complications and symptoms, including kidney stones, weakened bones, hypertension, nausea, and constipation[6,10]. Furthermore, some cases of PHPT are related to inherited conditions, such as MEN1, involving the parathyroid glands[6,7]. Carsote et al[6] reviewed 1375 cases of hypercalcemia-induced pancreatitis in 9 studies and summarized that MEN1 with PHPT has been reported in 85%-90% of the subjects. Therefore, an accumulation of symptomatic PHPT case information will contribute to establishing diagnostic and treatment algorithms and facilitating the early detection of MEN[1-7].
PHPT in the pregnancy period is a rare occurrence, with approximately 1% reported incidence[13,14]. However, the number of case reports has increased in recent years, and more information is available[15,16]. Diagnosis of PHPT is difficult during pregnancy due to the nonspecific symptoms; however, careful screening is necessary to prevent adverse outcomes for the mother and fetus, as well as the neonate, especially when serum calcium levels are elevated. Incidents of acute pancreatitis during pregnancy are further rare, which have been reported to range between 0.1% and 0.01%[17-20]. However, considering the serious complications for both mother and fetus, it is important to diagnose properly and provide appropriate therapeutic options. PHPT is one of the causes of acute pancreatitis in the pregnancy period as well as in non-pregnant cases[3,8-12]. Therefore, although rare, the information regarding PTPH-induced acute pancreatitis during pregnancy was an unmet need for accurate diagnosis and therapeutic intervention for a better outcome for the mother, fetus, and neonate. For this condition, Augustin et al[1] reviewed 54 cases of PTPH-induced acute pancreatitis in pregnancy from 51 studies in 55 years since 1968. The study collected and reviewed the largest number of cases reported to date. Among these cases, for treating PHPT, surgical treatment was performed in 33 cases during pregnancy and 12 cases after delivery. No detailed information was available for the remaining nine cases. Histological analyses revealed the parathyroid adenoma (46 cases), carcinoma (2 cases), and hyperplasia (1 case).
Regarding the maternal and fetal mortality of 9.3%, the authors analyzed various factors. For maternal outcomes of alive or death, age, various factors including, previous pregnancies, previous deliveries, pancreatitis occurrence in gestational week, pancreatitis postpartum, amylase, lipase, calcium, phosphorus, number of abortion, complex delivery, delivery occurrence week, and fetal/child death and no difference in the two groups were shown. It should be noted; however, that the maternal death rate was observed to be higher in cases where surgical intervention was required for pancreatitis management compared with the cases treated conservatively (60.0% vs 16.3%). Moreover, maternal deaths were associated with elevated PTH levels (910 pg/mL vs 302 pg/mL). Regarding fetal/child outcomes, when the five cases of mortality group was compared with the survivors, the mortality group demonstrated statistically elevated calcium (4.1 mmol/L vs 3.3 mmol/L) and PTH (1914 pg/mL vs 302 pg/mL) levels. The need for surgical intervention for acute pancreatitis was similar in both groups (20.0% vs 20.4%)[1].
Previous studies have reported that maternal hypercalcemia can induce premature birth, intrauterine growth retardation, suppression of fetal parathyroid gland development, and neonatal hypocalcemia, which results in tetany that can persist for several weeks. High maternal PTH levels also result in elevated maternal blood pressure, increasing the risk of preeclampsia[21,22]. These pathologies induced by elevated serum calcium and PTH levels contribute to the increased mortality. Further analysis by Augustin et al[1], using a multivariable logistic regression model, demonstrated that serum lipase levels at the time of acute pancreatitis, and the timing of delivery are related to the risk of maternal mortality in PHPT-induced acute pancreatitis. Complex delivery was found to be a risk factor for fetal/child mortality.
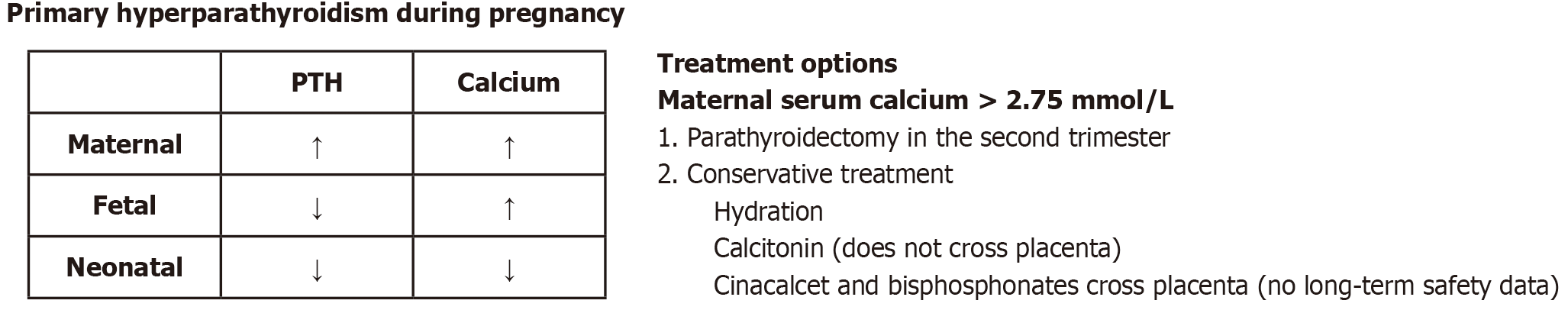
According to the reports[13-16] and guidelines from The American Association of Endocrine Surgeons, surgical treatment is recommended for symptomatic cases, cases having serum calcium levels of greater than 1 mg/dL, and cases complicated with nephrolithiasis, nephrocalcinosis, hypercalciuria, impaired renal function, osteoporosis, or fragility fracture[23]. In addition, a single-center study has demonstrated that PHPT can be managed conservatively in pregnancy with calcium levels of < 2.85 mmol/L when no complications such as acute pancreatitis or other hypercalcemia syndrome are present[24]. No consensus currently exists regarding the treatment of PHPT in pregnancy; however, parathyroidectomy performed in the second trimester is preferred when the patient is symptomatic or if the calcium level is high (> 2.75 mmol/L)[16,17,25,26]. Calcitonin, cinacalcet, and bisphosphonate could be used; however, due to the lack of long-term safety data no guidelines on medications are currently available. Particularly, as cinacalcet and bisphosphonates cross the placenta and might be embryotoxic (Figure 1)[21].
Serum calcium levels decrease during pregnancy, primarily due to hemodilution, decreased serum albumin levels, and calcium transport from the mother to the fetus[21,22,27]. Therefore, elevated serum calcium levels during pregnancy might indicate the presence of a pathophysiological condition. Augustin et al[1] concluded that early diagnosis of PTPH-induced acute pancreatitis with the serum calcium test is warranted for detecting acute pancreatitis during pregnancy. This is because higher calcium and PTH values increase the risk of fetal and child mortalities, abortions, and complex deliveries. Meanwhile, in this review, the screening workup for MEN was reported in only three cases. Most PHPT cases are sporadic, and their incidence is estimated to be 0.3% in the general population[10]; on the other hand, 5%-10% of PHPT patients might have syndromes and hereditary diseases, including MEN1. MEN1 is an autosomal dominant inherited tumor syndrome that is characterized by the presence of pancreatic, parathyroid, and pituitary gland tumors[2]. Imaging studies, including computed tomography, parathyroid scintigraphy with 99mTc, and magnetic resonance imaging, assist in the diagnosis[28]. Parathyroid tumors are the most common cause of hyperparathyroidism and are detected in > 90% of patients with MEN1[2,3,28]. MEN1 can be fatal if not accurately diagnosed and treated. To date, information regarding the impact of MEN1 on pregnancy is insufficient, and further reports, including actual case experiences, are warranted[27]. According to published reports, MEN1-induced endocrinopathies affect pregnancies, with a high incidence of complications related to PHPT, while non-parathyroid symptoms are less frequent. Additionally, maternal calcium and blood glucose levels are key factors for screening and monitoring hypercalcemia and gestational diabetes, which are the major complications of pregnancy in MEN1 cases[27]. Magnetic resonance imaging and ultrasonography are useful for diagnosing parathyroid tumors in pregnant women due to their sensitivity and lack of exposure to ionizing radiation. Hypercalcemia results in maternal complications such as renal stones, arrhythmia, pancreatitis, miscarriage, and preeclampsia[21,22,29]. Therefore, parathyroidectomy in the second trimester of pregnancy is recommended to reduce maternal and fetal mortality caused by these clinical symptoms and to minimize the risk of complications[21,22,29]. Therefore, screening for MEN1 is also essential for the cases diagnosed with PHPT-induced acute pancreatitis in pregnancy.
Understanding PHPT-induced acute pancreatitis and its occurrence in pregnancy is important for the early diagnosis and appropriate therapeutic intervention to prevent maternal and fetal adverse outcomes. Further consideration of MEN screening could be considered for the PHPT etiology for a better prognosis.
| 1. | Augustin G, Lai Q, Cigrovski Berkovic M. Primary hyperparathyroidism-induced acute pancreatitis in pregnancy: A systematic review with a diagnostic-treatment algorithm. World J Gastroenterol. 2024;30:3755-3765. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (33)] |
| 2. | Palermo A, Tabacco G, Makras P, Zavatta G, Trimboli P, Castellano E, Yavropoulou MP, Naciu AM, Anastasilakis AD. Primary hyperparathyroidism: from guidelines to outpatient clinic. Rev Endocr Metab Disord. 2024;25:875-896. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Bilezikian JP, Khan AA, Silverberg SJ, Fuleihan GE, Marcocci C, Minisola S, Perrier N, Sitges-Serra A, Thakker RV, Guyatt G, Mannstadt M, Potts JT, Clarke BL, Brandi ML; International Workshop on Primary Hyperparathyroidism. Evaluation and Management of Primary Hyperparathyroidism: Summary Statement and Guidelines from the Fifth International Workshop. J Bone Miner Res. 2022;37:2293-2314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 219] [Article Influence: 73.0] [Reference Citation Analysis (0)] |
| 4. | Salmon MK, Fritz CG, Barrette LX, Romeo D, Suresh NV, Ng JJ, Balar E, Prasad A, Moreira A, Rajasekaran K. Quality appraisal of clinical practice guidelines for the evaluation and management of primary hyperparathyroidism. Endocrine. 2024;85:864-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Silva BC, Cusano NE, Bilezikian JP. Primary hyperparathyroidism. Best Pract Res Clin Endocrinol Metab. 2024;38:101247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 6. | Carsote M, Nistor C, Gheorghe AM, Sima OC, Trandafir AI, Nistor TVI, Sandulescu BA, Ciobica ML. Turning Points in Cross-Disciplinary Perspective of Primary Hyperparathyroidism and Pancreas Involvements: Hypercalcemia-Induced Pancreatitis, MEN1 Gene-Related Tumors, and Insulin Resistance. Int J Mol Sci. 2024;25:6349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 7. | Yuan JH, Luo S, Zhang DG, Wang LS. Early detection of multiple endocrine neoplasia type 1: A case report. World J Gastroenterol. 2024;30:3247-3252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Mederos MA, Reber HA, Girgis MD. Acute Pancreatitis: A Review. JAMA. 2021;325:382-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 487] [Article Influence: 121.8] [Reference Citation Analysis (1)] |
| 9. | Boxhoorn L, Voermans RP, Bouwense SA, Bruno MJ, Verdonk RC, Boermeester MA, van Santvoort HC, Besselink MG. Acute pancreatitis. Lancet. 2020;396:726-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 579] [Article Influence: 115.8] [Reference Citation Analysis (0)] |
| 10. | Misgar RA, Bhat MH, Rather TA, Masoodi SR, Wani AI, Bashir MI, Wani MA, Malik AA. Primary hyperparathyroidism and pancreatitis. J Endocrinol Invest. 2020;43:1493-1498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Ward JB, Petersen OH, Jenkins SA, Sutton R. Is an elevated concentration of acinar cytosolic free ionised calcium the trigger for acute pancreatitis? Lancet. 1995;346:1016-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 115] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Mithöfer K, Fernández-del Castillo C, Frick TW, Lewandrowski KB, Rattner DW, Warshaw AL. Acute hypercalcemia causes acute pancreatitis and ectopic trypsinogen activation in the rat. Gastroenterology. 1995;109:239-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 77] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | McCarthy A, Howarth S, Khoo S, Hale J, Oddy S, Halsall D, Fish B, Mariathasan S, Andrews K, Oyibo SO, Samyraju M, Gajewska-Knapik K, Park SM, Wood D, Moran C, Casey RT. Management of primary hyperparathyroidism in pregnancy: a case series. Endocrinol Diabetes Metab Case Rep. 2019;2019:19-0039. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Arshad MF, Arambewela MH, Bennet WM, Sterrenburg M, Balasubramanian SP. Primary hyperparathyroidism in pregnancy: experience of a tertiary centre. Surg Today. 2023;53:470-475. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Eremkina A, Bibik E, Mirnaya S, Krupinova J, Gorbacheva A, Dobreva E, Mokrysheva N. Different treatment strategies in primary hyperparathyroidism during pregnancy. Endocrine. 2022;77:556-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 16. | Musleh A, Shrateh ON, Abbadi K, Asbah M, Khader A. Successful surgical management of primary hyperparathyroidism during pregnancy: a rare case report. Ann Med Surg (Lond). 2023;85:1150-1153. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Motlaghzadeh Y, Bilezikian JP, Sellmeyer DE. Hypercalcemia Associated with Pregnancy and Lactation. Endocrinol Metab Clin North Am. 2024;53:437-452. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Mądro A. Pancreatitis in Pregnancy-Comprehensive Review. Int J Environ Res Public Health. 2022;19:16179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 19. | Maringhini A, Rossi M, Patti R, Maringhini M, Vassallo V. Acute Pancreatitis during and after Pregnancy: A Review. J Clin Med. 2024;13:2028. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Niu C, Zhang J, Liu H, Zhu K, Okolo PI 3rd. Maternal and fetal outcomes of acute pancreatitis in pregnancy: a population-based study. Eur J Gastroenterol Hepatol. 2023;35:1354-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Tsourdi E, Anastasilakis AD. Parathyroid Disease in Pregnancy and Lactation: A Narrative Review of the Literature. Biomedicines. 2021;9:475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Scholl TO, Chen X, Stein TP. Maternal calcium metabolic stress and fetal growth. Am J Clin Nutr. 2014;99:918-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 23. | Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, Doherty GM, Herrera MF, Pasieka JL, Perrier ND, Silverberg SJ, Solórzano CC, Sturgeon C, Tublin ME, Udelsman R, Carty SE. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg. 2016;151:959-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 612] [Article Influence: 68.0] [Reference Citation Analysis (0)] |
| 24. | Rigg J, Gilbertson E, Barrett HL, Britten FL, Lust K. Primary Hyperparathyroidism in Pregnancy: Maternofetal Outcomes at a Quaternary Referral Obstetric Hospital, 2000 Through 2015. J Clin Endocrinol Metab. 2019;104:721-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 25. | Diaz-Soto G, Linglart A, Sénat MV, Kamenicky P, Chanson P. Primary hyperparathyroidism in pregnancy. Endocrine. 2013;44:591-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 26. | Ali DS, Dandurand K, Khan AA. Primary Hyperparathyroidism in Pregnancy: Literature Review of the Diagnosis and Management. J Clin Med. 2021;10:2956. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 27. | Brandi ML, Agarwal SK, Perrier ND, Lines KE, Valk GD, Thakker RV. Multiple Endocrine Neoplasia Type 1: Latest Insights. Endocr Rev. 2021;42:133-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 126] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 28. | Takahashi S, Kamimura K, Abe H, Watanabe Y, Hayashi K, Mizuno K, Yamamoto T, Takeuchi M, Natsui M, Terai S. Multiple Endocrine Neoplasia Type 1-Related Acute Pancreatitis. Pancreas. 2019;48:e35-e38. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 29. | Pitkin RM, Gebhardt MP. Serum calcium concentrations in human pregnancy. Am J Obstet Gynecol. 1977;127:775-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 1.1] [Reference Citation Analysis (0)] |