Published online Feb 21, 2024. doi: 10.3748/wjg.v30.i7.770
Peer-review started: October 6, 2023
First decision: January 5, 2024
Revised: January 9, 2024
Accepted: January 22, 2024
Article in press: January 22, 2024
Published online: February 21, 2024
Processing time: 138 Days and 1.3 Hours
Liver metastases can appear in different forms in magnetic resonance imaging. Contrary to popular belief, while radiologists report hypovascular or hyper
Core Tip: Maino et al summarized the most frequent appearances of liver metastasis in detail. This letter adds to the mentioned literature with atypical examples and a potential misleading infectious cause, alveolar echinococcosis.
- Citation: Memis KB, Aydin S. Complementary comments on metastatic liver lesions with exceptional and rare cases. World J Gastroenterol 2024; 30(7): 770-773
- URL: https://www.wjgnet.com/1007-9327/full/v30/i7/770.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i7.770
Maino et al[1] recently published research suggesting the role of magnetic resonance imaging (MRI) in liver metastases. They reviewed the importance of MRI in the diagnosis and evaluation of liver metastases, as well as a description of their primary imaging characteristics. Additionally, they described MRI protocols using contrast agents to better diagnose liver metastases. Furthermore, the study emphasises the added value of the most recent imaging tools as well as the usual and atypical appearance of liver metastases, which increases their effect[1]. This letter aims to contribute to this review by presenting rare and atypical examples of liver metastases.
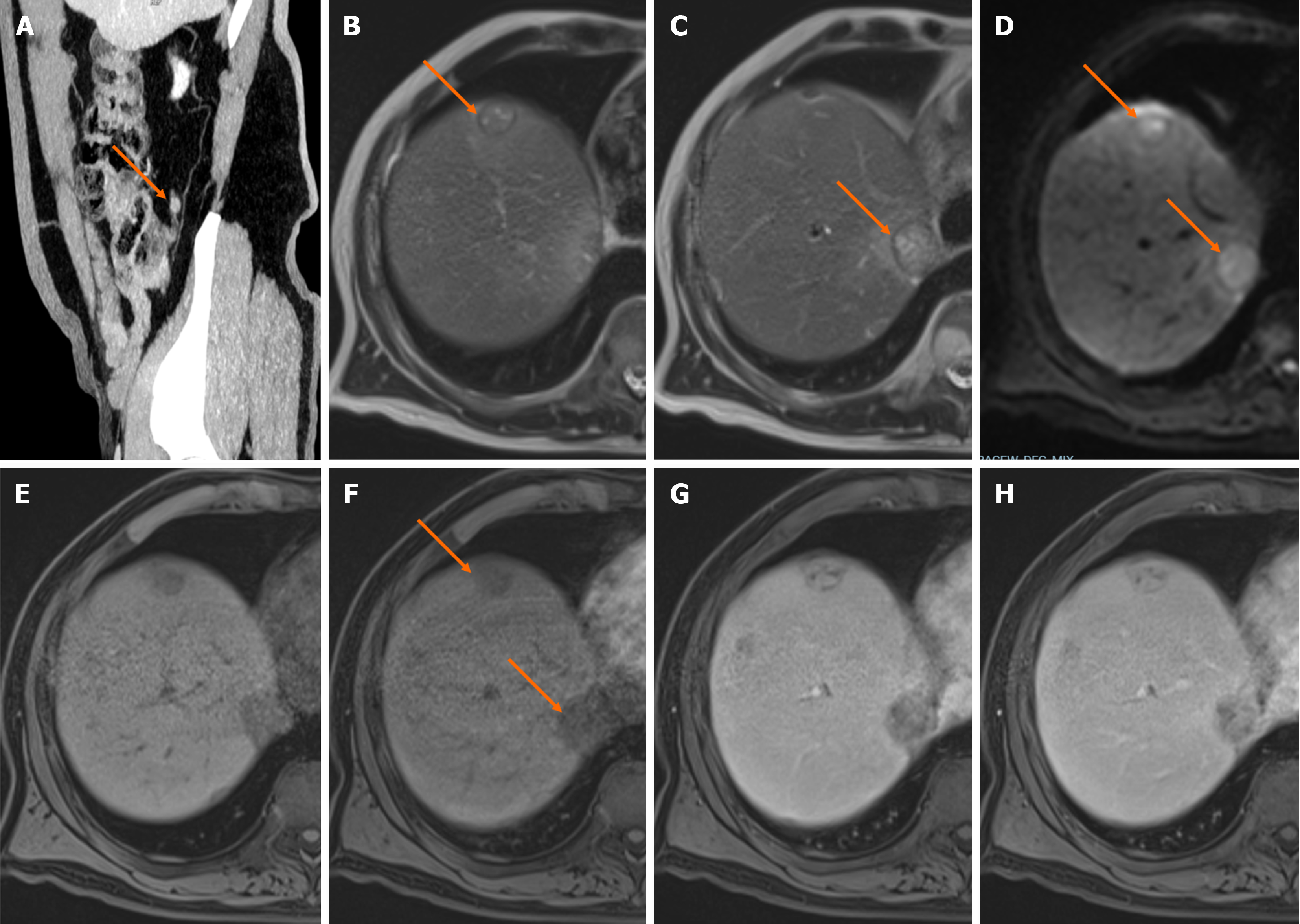
According to the authors of this study, hypovascular lesions are the most common typical appearances of liver metastases, but some tumors will present with atypical appearances, such as hypervascular metastases. As mentioned in the literature, hypervascular liver metastases typically arise from hypervascular primary cancers such as neuroendocrine cancers, kidney cancer, melanoma, and thyroid cancer[1,2]. In 73% of patients, hepatic metastases of neuroendocrine tumors displayed a characteristic hypervascular appearance. However, it should be kept in mind that hypervascular neuroendocrine tumors may cause hypovascular liver metastasis[3]. As seen in Figure 1, neuroendocrine tumors should also be included in the differential diagnosis of hypovascular liver metastases.
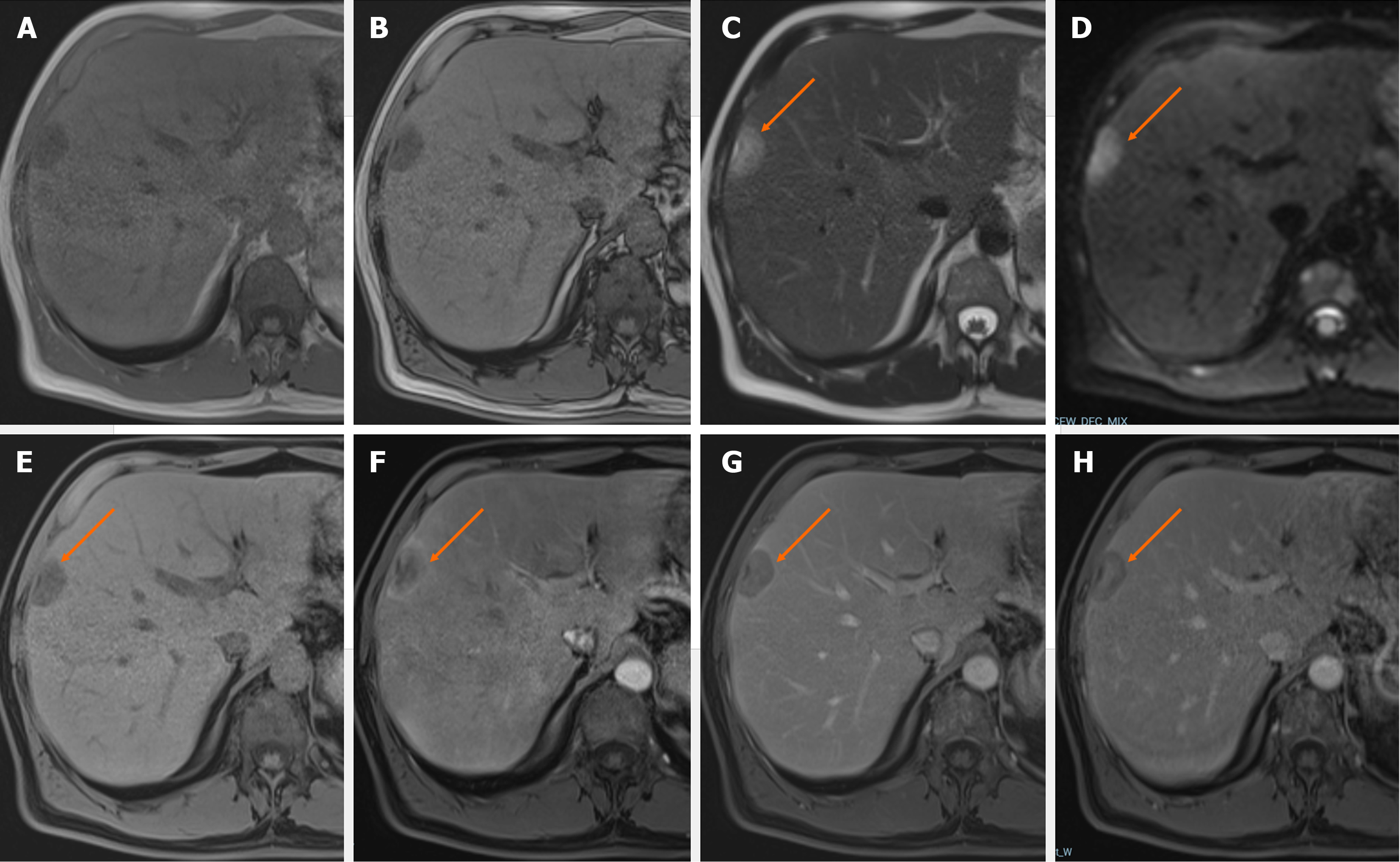
The article by Ozaki et al[2] demonstrated the prevalence of synchronous liver metastasis in primary tumors originating from various organs. They determined that the pancreas had the highest prevalence (77.6%), whereas the prostate had the lowest prevalence (4.8%). We intended to make this unusual entity memorable with our case in Figure 2, which shows the metastasis of prostate adenocarcinoma to the liver.
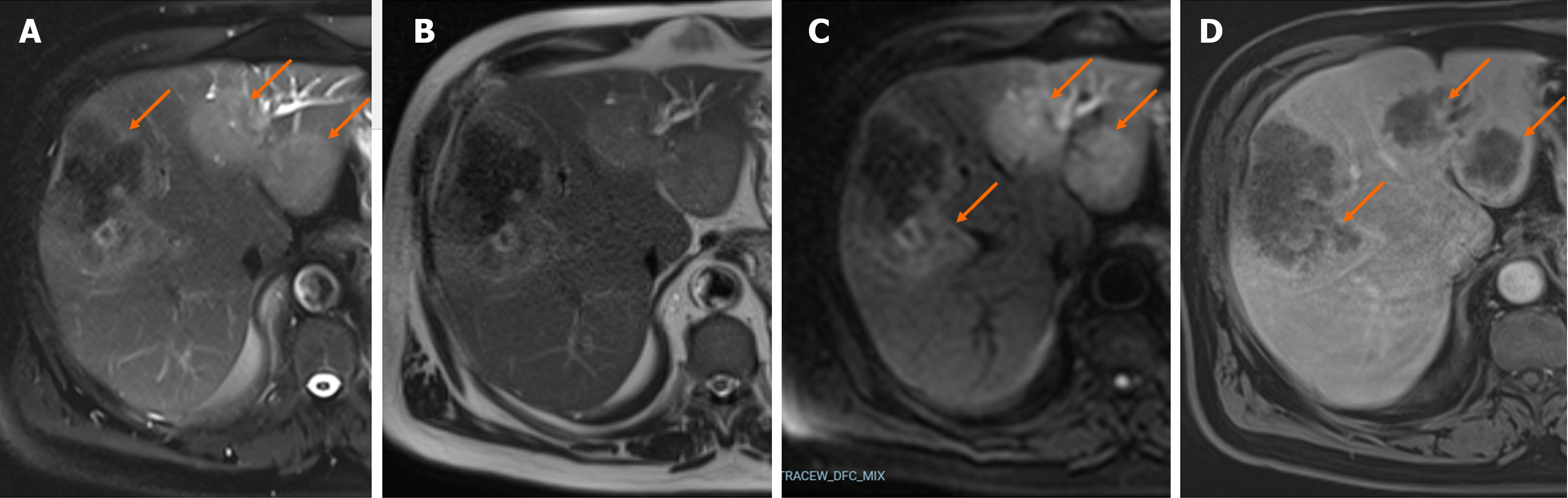
When describing the visible liver lesions as metastases, a differential diagnosis between primary benign or malignant liver masses and infectious diseases should be made initially. While multiple liver abscesses are the most common among these infectious lesions, alveolar echinococcosis (AE), a rare parasitic disease that we present in Figure 3, can also be misdiagnosed as metastases. The WHO classification system for PNM, based on imaging findings, also emphasises AE as a potential alternative differential diagnosis for malignant liver masses. To distinguish AE from other tumors, serology findings and multiple imaging modalities (ultrasonography and computed tomography), and most importantly, keeping the diagnosis in mind, are required[4-6].
Our objective in this letter was to make a contribution to the literature with images of exceptional and rarely occurring cases in daily practice. All authors are in complete agreement with the information stated. The content of this manuscript is our original work and has not been published, in whole or in part, before or simultaneously with this submission.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Isac S, Romania; Liu T, China S-Editor: Fan JR L-Editor: A P-Editor: Cai YX
| 1. | Maino C, Vernuccio F, Cannella R, Cortese F, Franco PN, Gaetani C, Giannini V, Inchingolo R, Ippolito D, Defeudis A, Pilato G, Tore D, Faletti R, Gatti M. Liver metastases: The role of magnetic resonance imaging. World J Gastroenterol. 2023;29:5180-5197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 16] [Article Influence: 8.0] [Reference Citation Analysis (3)] |
| 2. | Ozaki K, Higuchi S, Kimura H, Gabata T. Liver Metastases: Correlation between Imaging Features and Pathomolecular Environments. Radiographics. 2022;42:1994-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 38] [Reference Citation Analysis (0)] |
| 3. | Dromain C, de Baere T, Baudin E, Galline J, Ducreux M, Boige V, Duvillard P, Laplanche A, Caillet H, Lasser P, Schlumberger M, Sigal R. MR imaging of hepatic metastases caused by neuroendocrine tumors: comparing four techniques. AJR Am J Roentgenol. 2003;180:121-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 127] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | Amano T, Hayashi S, Nishida T, Matsubara T, Takahashi K, Nakamatsu D, Tomimaru Y, Yamamoto M, Nakajima S, Fukui K, Tamura H, Adachi S, Dono K, Inada M. Alveolar Echinococcosis Mimicking a Hepatic Neoplasm with Lymph Node Metastasis: A Case Report. Case Rep Gastroenterol. 2018;12:587-596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Kantarci M, Aydin S, Eren S, Ogul H, Akhan O. Imaging Aspects of Hepatic Alveolar Echinococcosis: Retrospective Findings of a Surgical Center in Turkey. Pathogens. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Eren S, Aydın S, Kantarci M, Kızılgöz V, Levent A, Şenbil DC, Akhan O. Percutaneous management in hepatic alveolar echinococcosis: A sum of single center experiences and a brief overview of the literature. World J Gastrointest Surg. 2023;15:398-407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |