Published online Feb 14, 2024. doi: 10.3748/wjg.v30.i6.599
Peer-review started: December 11, 2023
First decision: December 15, 2023
Revised: December 18, 2023
Accepted: January 16, 2024
Article in press: January 16, 2024
Published online: February 14, 2024
Processing time: 56 Days and 3.3 Hours
Treatment of postoperative anastomotic stenosis for colorectal cancer is often challenging, especially for patients who do not respond well to endoscopy. In cases where patients have undergone an enterostomy, the stenosis can be easily resolved through magnetic compression. However, common magnetic compre
We here report the case of a 57-year-old woman who had undergone a laparoscopic radical rectum resection (Dixon) for rectal cancer. However, she started facing difficulty in defecation 6 months after surgery. Her colonoscopy indicated stenosis of the rectal anastomosis. Endoscopic balloon dilation was performed six times on her. However, the stenosis still showed a trend of gradual aggravation. Because the patient did not undergo an enterostomy, the conventional endoscopic magnetic compression technique could not be performed. Hence, we imple
The Y–Z DMR deformable magnetic ring is an excellent treatment strategy for patients with rectal stenosis and without enterostomy.
Core Tip: The magnetic compression technique can be used to treat patients with rectal stenosis that have also undergone an enterostomy. However, the existing magnetic ring cannot be used in patients without enterostomy. We designed a Y–Z deformable magnetic ring (Y–Z DMR), which can realize the single channel of the magnet placed through the anus. This paper reports the first successful clinical case of using the Y–Z DMR for the treatment of rectal stenosis.
- Citation: Zhang MM, Sha HC, Qin YF, Lyu Y, Yan XP. Y–Z deformable magnetic ring for the treatment of rectal stricture: A case report and review of literature. World J Gastroenterol 2024; 30(6): 599-606
- URL: https://www.wjgnet.com/1007-9327/full/v30/i6/599.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i6.599
Rectal stenosis is a common postoperative complication of rectal cancer. Endoscopic treatment is generally preferred for such conditions. Balloon dilation[1,2], stent placement[3,4], and endoscopic radial incision[5] are some of the commonly used procedures that provide satisfactory treatment results in most patients. However, these procedures still lead to poor results in some patients, resulting in the need for surgical resection of anastomotic stenosis[6] or even permanent enterostomy. In addition, patients who have not undergone a prophylactic ileostomy or in whom stenosis occurs after ostomy reduction need urgent treatment.
Magnetic compression anastomosis (MCA) is a novel technique for the anastomosis of cavity organs through “non-contact” magnetic force. The current basic and clinical studies on MCA cover esophageal anastomosis[7-9], gastroin
Herein, we present a patient with the stenosis of rectal anastomosis and no enterostomy. For this case, we specially designed a Y–Z deformable magnetic ring (Y–Z DMR) and successfully achieved narrow recanalization in a single passage through the anus. The defecation status remained good even after 6 months of follow-up. This is the first study to report the clinical application of Y–Z DMR, which is of great clinical significance.
A 57-year-old woman presented to us in May 2023 for having difficulty in passing stools. She had undergone laparoscopic rectal cancer surgery 16 months ago (January 2022) and had started facing difficulty defecating 4 months after the surgery.
The patient had undergone laparoscopic radical rectum resection (Dixon) for rectal cancer at a local hospital 16 months ago and had recovered well after surgery. This patient did not undergo chemo-radio therapy before or after surgery. However, she started facing difficulties in defecation 1 year ago (May 2022). As a result, a colonoscopy was performed on her at a local hospital, which indicated stenosis of the rectal anastomosis. She underwent endoscopic balloon dilation treatment six times for the condition. However, the results were not satisfactory. For further treatment, the patient was admitted to the Magnetic Surgery Clinic of the First Affiliated Hospital of Xi’an Jiaotong University.
The patient had no history of acute or chronic infectious diseases, heart disease, hypertension or diabetes, or surgery other than laparoscopic radical rectum resection.
The patient did not have any relevant family medical history.
The patient’s vital signs were stable, with no obvious abnormalities in the physical examination of both her lungs and heart. Her abdomen was flat and soft, with no abdominal tenderness. Shifting dullness in the abdomen was negative, and bowel sounds were also normal.
The patient’s hematology results were normal.
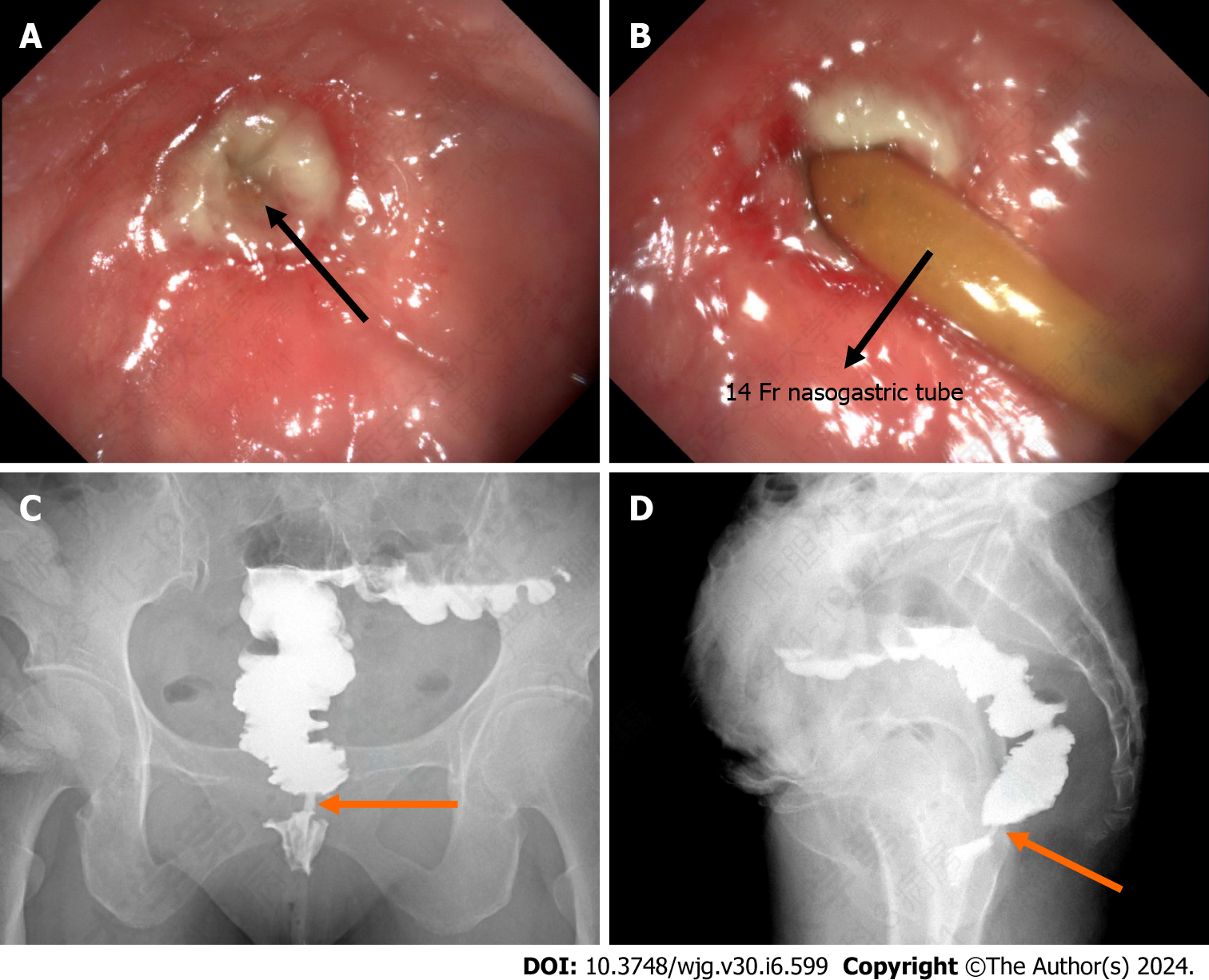
After admission to our hospital, the patient underwent further colonoscopy. The result indicated that the rectal anastomosis was severely narrowed (5 cm) from the anus. In addition, no obvious lumen was observed. Hence, an attempt was made to insert a 14 Fr nasogastric tube through the anus to pass through the stenosis. Colography was performed by injecting approximately 100 mL of iohexol through the nasogastric tube. The results showed that the stenosis of the rectum was 0.4 mm in diameter and 1 cm in length (Figure 1).
The patient was diagnosed with rectum stenosis based on her medical history and the imaging examination and colonoscopy results.
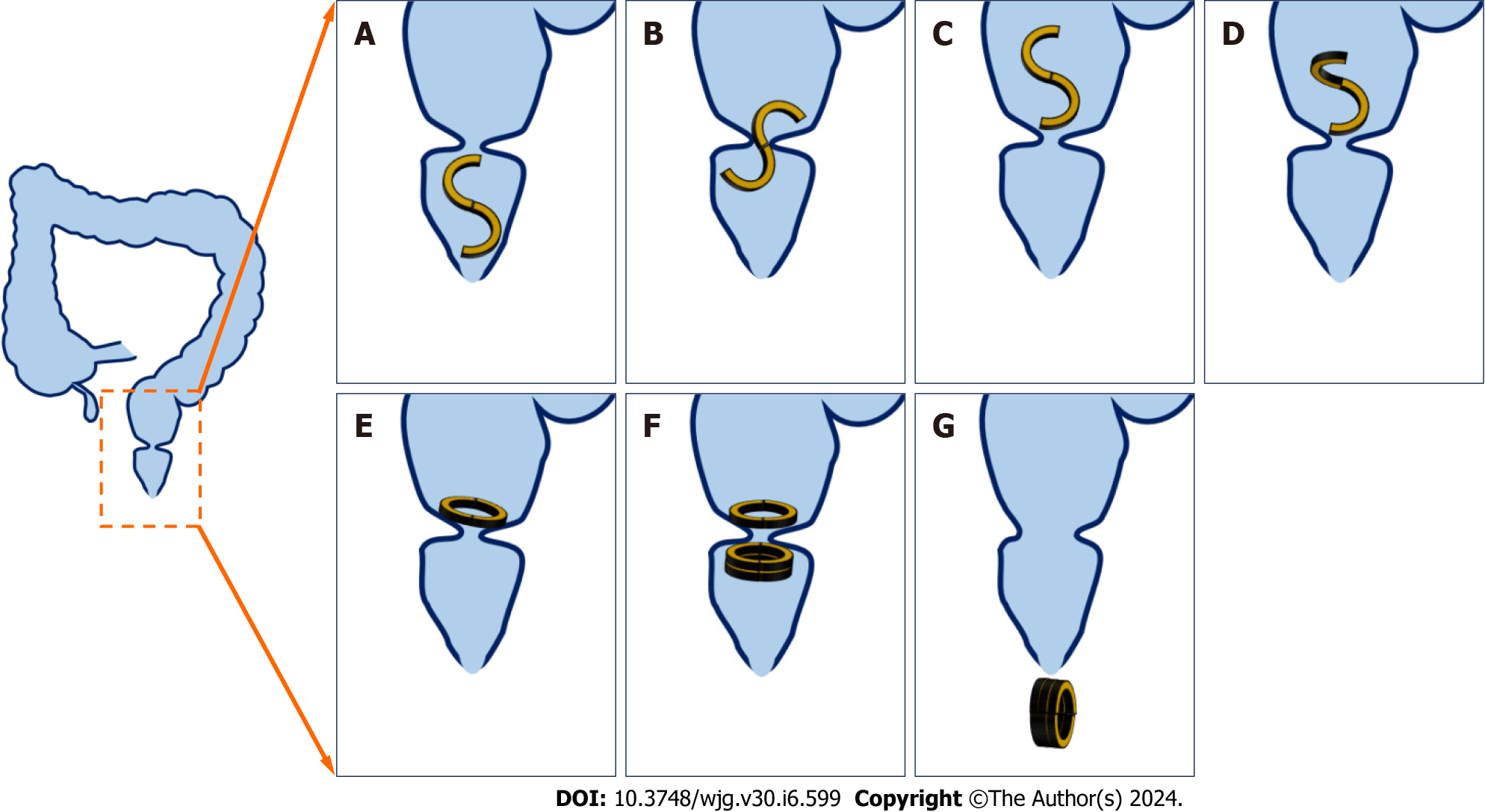
The patient refused further endoscopic treatment and surgery. Instead, she opted for minimally invasive magnetic surgery technique. The surgical plan was decided after a discussion with the Magnetic Surgery Multi-Disciplinary Treatment of the First Affiliated Hospital of Xi’an Jiaotong University (Figure 2). The patient agreed to the surgical protocol and signed the informed consent. The surgical plan was also approved by the Medical Department of the First Affiliated Hospital of Xi’an Jiaotong University. The S–O-shaped magnetic anastomosing ring designed by the author was used in the surgical plan. As the magnetic ring was designed, we named it the Y–Z DMR, also referred to as the Y–Z DMR. The Y–Z DMR was composed of two semicircular magnetic rings. The daughter magnetic ring was “S” shaped during the implantation process. It passed through the narrow section of the rectum in a serpentine motion. The daughter magnetic rings were manipulated by a control line to transform it from the “S” to the “O” shape. After adjusting the daughter magnetic ring to a suitable position, the two O-shaped parent magnetic rings were inserted through the anus. The daughter magnetic ring and the parent magnetic ring attracted each other and compressed the narrow section of the rectum. After a certain period, the scar of the narrow section and the magnetic rings fell off and were discharged through the anus.
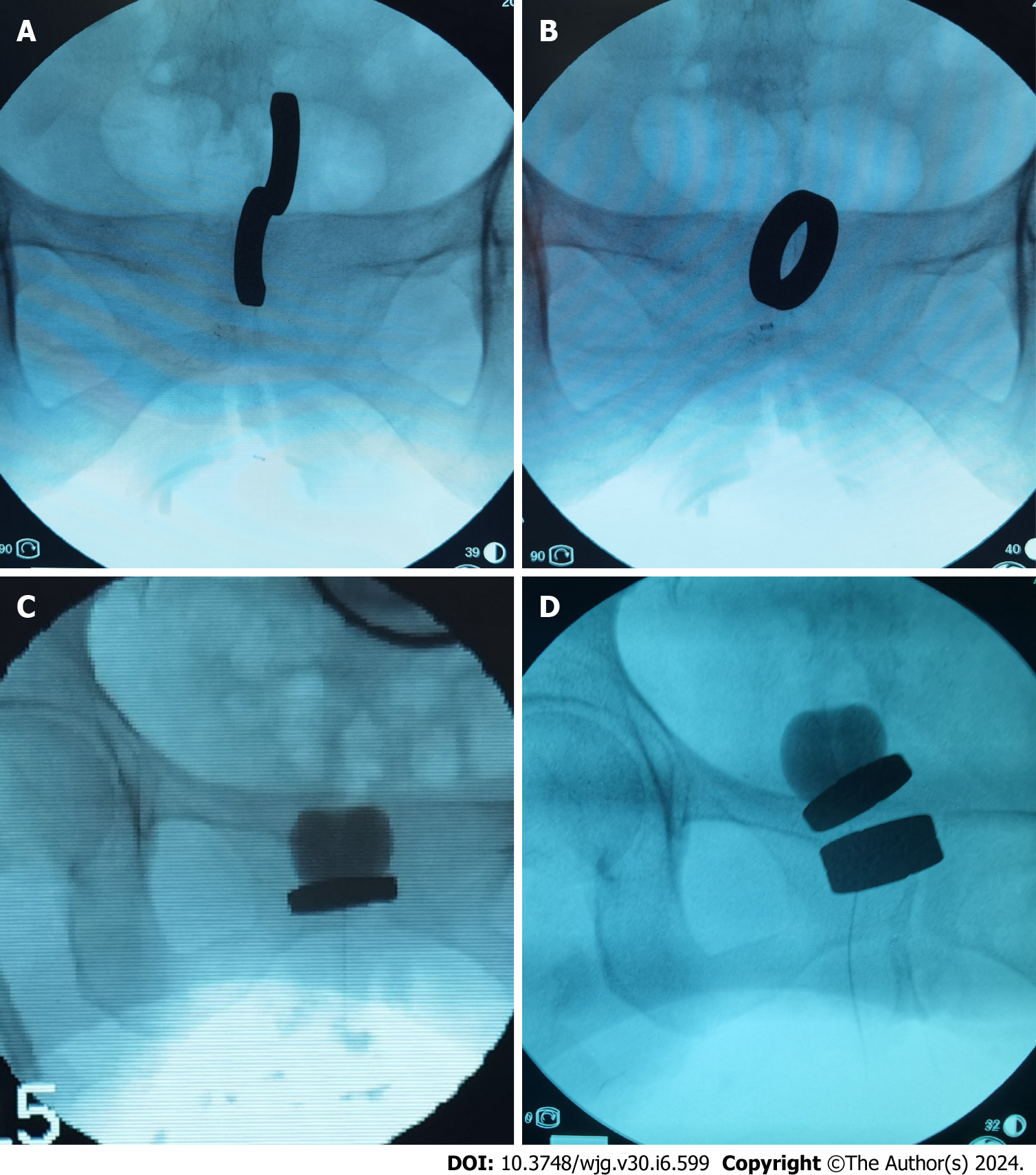
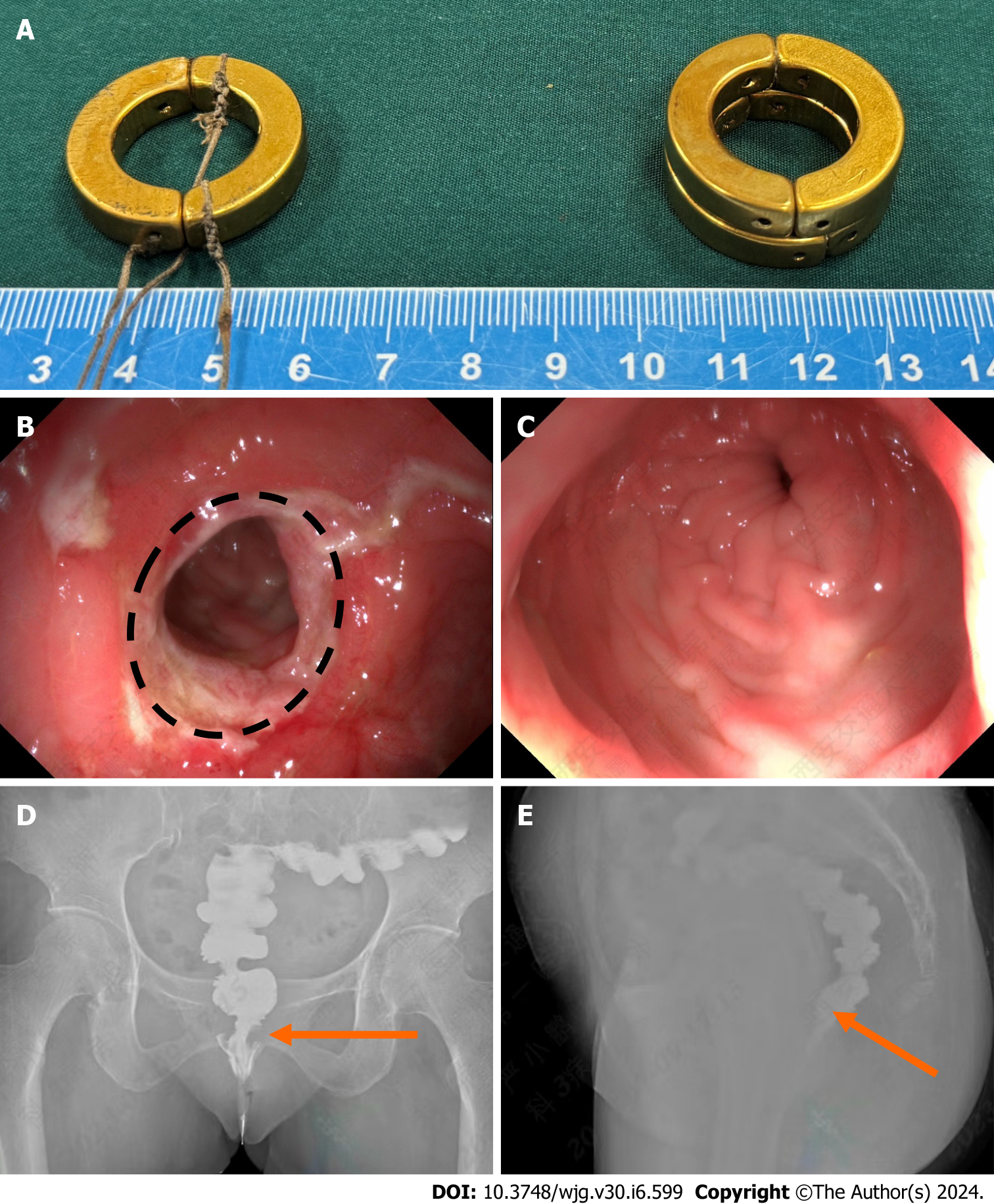
The patient was administered intravenous anesthesia and the lithotomy position was adopted. A disposable anoscope was inserted through the anus. Rectal stenosis could be seen directly with the naked eye. An S-shaped magnetic ring was inserted through the anus, which was passed through the narrow part of the rectum under X-ray surveillance (Figure 3A). After the control line was pulled, the magnetic ring changed its S shape to O shape (Figure 3B). The catheter was inserted through the anus so that the balloon passed through the narrow part of the rectum and the center of the O-ring. The catheter balloon was dilated by injecting 10 mL of diluted iohexol solution. The catheter was vertically pulled so that the O-shaped magnetic ring became perpendicular to the longitudinal axis of the rectum and close to the rectal stenosis (Figure 3C). Two O-shaped parent magnetic rings were inserted through the end of the catheter and pushed along the catheter to the narrow anal side of the rectum. The daughter and parent magnetic rings were attracted toward each other, compressing the narrow section of the rectum (Figure 3D). The catheter was placed in the rectum and the procedure was completed. On the 9th day after surgery, the magnet rings and catheter were pulled out through the anus (Figure 4A), establishing the MCA. Colonoscopy showed no bleeding, mucosal edema, or erosion at the anastomotic orifice (Figure 4B). The colonoscope successfully passed through the anastomotic orifice (Figure 4C). Further colonography showed that the stenosis of the rectum widened significantly (Figure 4D and E). The patient was discharged 10 d after surgery. The patient was strongly advised to use a 20-mm-diameter anal reaming stick 3 times a day for 5 min each time for 3 months after discharge to prevent restenosis.
The 6-month follow-up of the patient showed a generally good condition with normal bowel movements.
Before admission to our hospital, the patient had undergone balloon dilations six times. However, the stenosis kept gradually worsening, forcing the patient to rely only on a slag-free nutrient solution. As the patient refused other treatment options, she was offered the Y–Z DMR procedure. Thus, she became the first patient to benefit from the Y–Z DMR procedure.
In the previously reported cases of colorectal stenosis treated by the magnetic compression technique, all patients had undergone enterostomy. The resulting stoma provided an important access for placing magnets[30,31]. In the magnetic anastomosis of the digestive tract, the area of compression of the magnetic anastomosis ring is an important factor that determines the size of the final anastomosis. Therefore, to achieve the optimum magnet placement, clinicians tend to choose as large a magnetic ring as possible so as to obtain a larger anastomotic diameter. For those with a stoma, magnets can be easily inserted both through the anus and the stoma on either side of the rectum stenosis. In patients with rectal stenosis but without a stoma, conventional magnets cannot be inserted into the side of the rectal stenosis. Therefore, passing a large magnetic ring through the narrow section is a major research topic.
Inspired by the serpentine movement of snakes, we designed a Y–Z DMR with the following characteristics: First, it is composed of two semicircular magnetic rings. It forms an S-shaped structure when its one end is fixed and the other end is rotated by 180°. As a result, the cross-section of the magnet becomes significantly small, allowing the deformable magnetic ring to pass through the narrow section. Second, as the S-shaped magnetic ring adopts the serpentine move
Although we have treated only one patient at our clinic so far, our results show that it is possible to deform the Y-Z DMR from the S shape to the O shape. Satisfactory results were obtained at the 6-month follow-up. This is the first-generation Y–Z DMR. We believe that further optimization of the magnetic ring structure would increase the applications of the Y-Z DMR.
This study described the procedure and outcome of the first successful treatment of rectal stenosis using a Y–Z DMR through a unique anal access. The controllable deformation ability of the Y–Z DMR made this treatment strategy successful. We believe that our case report will provide more options to colorectal surgeons to treat rectal stenosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nakaji K, Japan S-Editor: Qu XL L-Editor: A P-Editor: Yuan YY
| 1. | Wang S, Wan J, Li Z, Long C, Zhang R, Luo Y, Han Z, Yan J. Comparison of the Efficacy of Endoscopic Radial Incision and Cutting Procedure and Endoscopic Balloon Dilation for Benign Anastomotic Stricture After Low Anterior Resection Combined With Preventive Loop Ileostomy in Rectal Cancer. Dis Colon Rectum. 2023;66:1392-1401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Clifford RE, Fowler H, Manu N, Vimalachandran D. Management of benign anastomotic strictures following rectal resection: a systematic review. Colorectal Dis. 2021;23:3090-3100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Lamazza A, Fiori E, Sterpetti AV, Schillaci A, Scoglio D, Lezoche E. Self-expandable metal stents in the treatment of benign anastomotic stricture after rectal resection for cancer. Colorectal Dis. 2014;16:O150-O153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Lamazza A, Fiori E, Schillaci A, Sterpetti AV, Lezoche E. Treatment of anastomotic stenosis and leakage after colorectal resection for cancer with self-expandable metal stents. Am J Surg. 2014;208:465-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Lee TG, Yoon SM, Lee SJ. Endoscopic radial incision and cutting technique for treatment-naive stricture of colorectal anastomosis: Two case reports. World J Gastrointest Surg. 2020;12:460-467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Imagami T, Takayama S, Maeda Y, Hattori T, Matsui R, Sakamoto M, Kani H. Surgical Resection of Anastomotic Stenosis after Rectal Cancer Surgery Using a Circular Stapler and Colostomy with Double Orifice. Case Rep Surg. 2019;2019:2898691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Sterlin A, Evans L, Mahler S, Lindner A, Dickmann J, Heimann A, Sahlabadi M, Aribindi V, Harrison MR, Muensterer OJ. An experimental study on long term outcomes after magnetic esophageal compression anastomosis in piglets. J Pediatr Surg. 2022;57:34-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Muensterer OJ, Sterlin A, Oetzmann von Sochaczewski C, Lindner A, Heimann A, Balus A, Dickmann J, Nuber M, Patel VH, Manfredi MA, Jennings RW, Smithers CJ, Fauza DO, Harrison MR. An experimental study on magnetic esophageal compression anastomosis in piglets. J Pediatr Surg. 2020;55:425-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Bruns NE, Glenn IC, Craner DR, Schomisch SJ, Harrison MR, Ponsky TA. Magnetic compression anastomosis (magnamosis) in a porcine esophagus: Proof of concept for potential application in esophageal atresia. J Pediatr Surg. 2019;54:429-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Gagner M, Abuladze D, Koiava L, Buchwald JN, Van Sante N, Krinke T. First-in-Human Side-to-Side Magnetic Compression Duodeno-ileostomy with the Magnet Anastomosis System. Obes Surg. 2023;33:2282-2292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Gagner M, Cadiere GB, Sanchez-Pernaute A, Abuladze D, Krinke T, Buchwald JN, Van Sante N, Van Gossum M, Dziakova J, Koiava L, Odovic M, Poras M, Almutlaq L, Torres AJ. Side-to-side magnet anastomosis system duodeno-ileostomy with sleeve gastrectomy: early multi-center results. Surg Endosc. 2023;37:6452-6463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Marchegiani F, Noll E, Riva P, Kong SH, Saccomandi P, Vita G, Lindner V, Namer IJ, Marescaux J, Diemunsch P, Diana M. Effects of Warmed and Humidified CO(2) Surgical Site Insufflation in a Novel Experimental Model of Magnetic Compression Colonic Anastomosis. Surg Innov. 2021;28:7-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Wall J, Diana M, Leroy J, Deruijter V, Gonzales KD, Lindner V, Harrison M, Marescaux J. MAGNAMOSIS IV: magnetic compression anastomosis for minimally invasive colorectal surgery. Endoscopy. 2013;45:643-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Klima U, MacVaugh H 3rd, Bagaev E, Maringka M, Kirschner S, Beilner J, Haverich A. Magnetic Vascular Port in minimally invasive direct coronary artery bypass grafting. Circulation. 2004;110:II55-II60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Zhang M, Ma J, An Y, Lyu Y, Yan X. Construction of an intrahepatic portosystemic shunt using the magnetic compression technique: preliminary experiments in a canine model. Hepatobiliary Surg Nutr. 2022;11:611-615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Heitmann C, Khan FN, Erdmann D, Olbrich KC, Adam Sharkawy A, Klitzman B. Vein graft anastomoses with magnets. J Plast Reconstr Aesthet Surg. 2007;60:1296-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Uygun I, Okur MH, Cimen H, Keles A, Yalcin O, Ozturk H, Otcu S. Magnetic compression gastrostomy in the rat. Pediatr Surg Int. 2012;28:529-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Uygun I, Okur MH, Arayici Y, Keles A, Ozturk H, Otcu S. Magnetic compression ostomy for simple tube colostomy in rats--magnacolostomy. Adv Clin Exp Med. 2012;21:301-305. [PubMed] |
| 19. | Uygun I, Okur MH, Cimen H, Keles A, Yalcin O, Ozturk H, Otcu S. Magnetic compression ostomy as new cystostomy technique in the rat: magnacystostomy. Urology. 2012;79:738-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Jang SI, Cho JH, Lee DK. Magnetic Compression Anastomosis for the Treatment of Post-Transplant Biliary Stricture. Clin Endosc. 2020;53:266-275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Jang SI, Lee KH, Joo SM, Park H, Choi JH, Lee DK. Maintenance of the fistulous tract after recanalization via magnetic compression anastomosis in completely obstructed benign biliary stricture. Scand J Gastroenterol. 2018;53:1393-1398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Kubo M, Wada H, Eguchi H, Gotoh K, Iwagami Y, Yamada D, Akita H, Asaoka T, Noda T, Kobayashi S, Nakamura M, Ono Y, Osuga K, Yamanouchi E, Doki Y, Mori M. Magnetic compression anastomosis for the complete dehiscence of hepaticojejunostomy in a patient after living-donor liver transplantation. Surg Case Rep. 2018;4:95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Shlomovitz E, Copping R, Swanstrom LL. Magnetic Compression Anastomosis for Recanalization of Complete Ureteric Occlusion after Radical Cystoprostatectomy. J Vasc Interv Radiol. 2023;34:1640-1641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Holler AS, König TT, Chen C, Harrison MR, Muensterer OJ. Esophageal Magnetic Compression Anastomosis in Esophageal Atresia Repair: A PRISMA-Compliant Systematic Review and Comparison with a Novel Approach. Children (Basel). 2022;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | Evans LL, Chen CS, Muensterer OJ, Sahlabadi M, Lovvorn HN, Novotny NM, Upperman JS, Martinez JA, Bruzoni M, Dunn JCY, Harrison MR, Fuchs JR, Zamora IJ. The novel application of an emerging device for salvage of primary repair in high-risk complex esophageal atresia. J Pediatr Surg. 2022;57:810-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Ödemiş B, Başpınar B, Durak MB, Coşkun O, Torun S. Lumen reconstruction with magnetic compression anastomosis technique in a patient with complete esophageal stricture. Acta Gastroenterol Belg. 2022;85:393-395. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Zhang M, He S, Sha H, Xue H, Lv Y, Yan X. A novel self-shaping magnetic compression anastomosis ring for treatment of colonic stenosis. Endoscopy. 2023;55:E1132-E1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 28. | Mascagni P, Tringali A, Boškoski I, Bove V, Schepis T, Perri V, Costamagna G. Magnetic kissing for the endoscopic treatment of a complete iatrogenic stenosis of the hypopharynx. Endoscopy. 2023;55:E499-E500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 29. | Zhang M, Lyu X, Zhao G, An Y, Lyu Y, Yan X. Establishment of Yan-Zhang's staging of digestive tract magnetic compression anastomosis in a rat model. Sci Rep. 2022;12:12445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 30. | Russell KW, Rollins MD, Feola GP, Scaife ER. Magnamosis: a novel technique for the management of rectal atresia. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Kamada T, Ohdaira H, Hoshimoto S, Narihiro S, Suzuki N, Marukuchi R, Takeuchi H, Yoshida M, Yamanouchi E, Suzuki Y. Magnetic compression anastomosis with atypical anastomosis for anastomotic stenosis of the sigmoid colon: a case report. Surg Case Rep. 2020;6:59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |