Published online Dec 7, 2024. doi: 10.3748/wjg.v30.i45.4844
Revised: September 23, 2024
Accepted: October 25, 2024
Published online: December 7, 2024
Processing time: 91 Days and 22.3 Hours
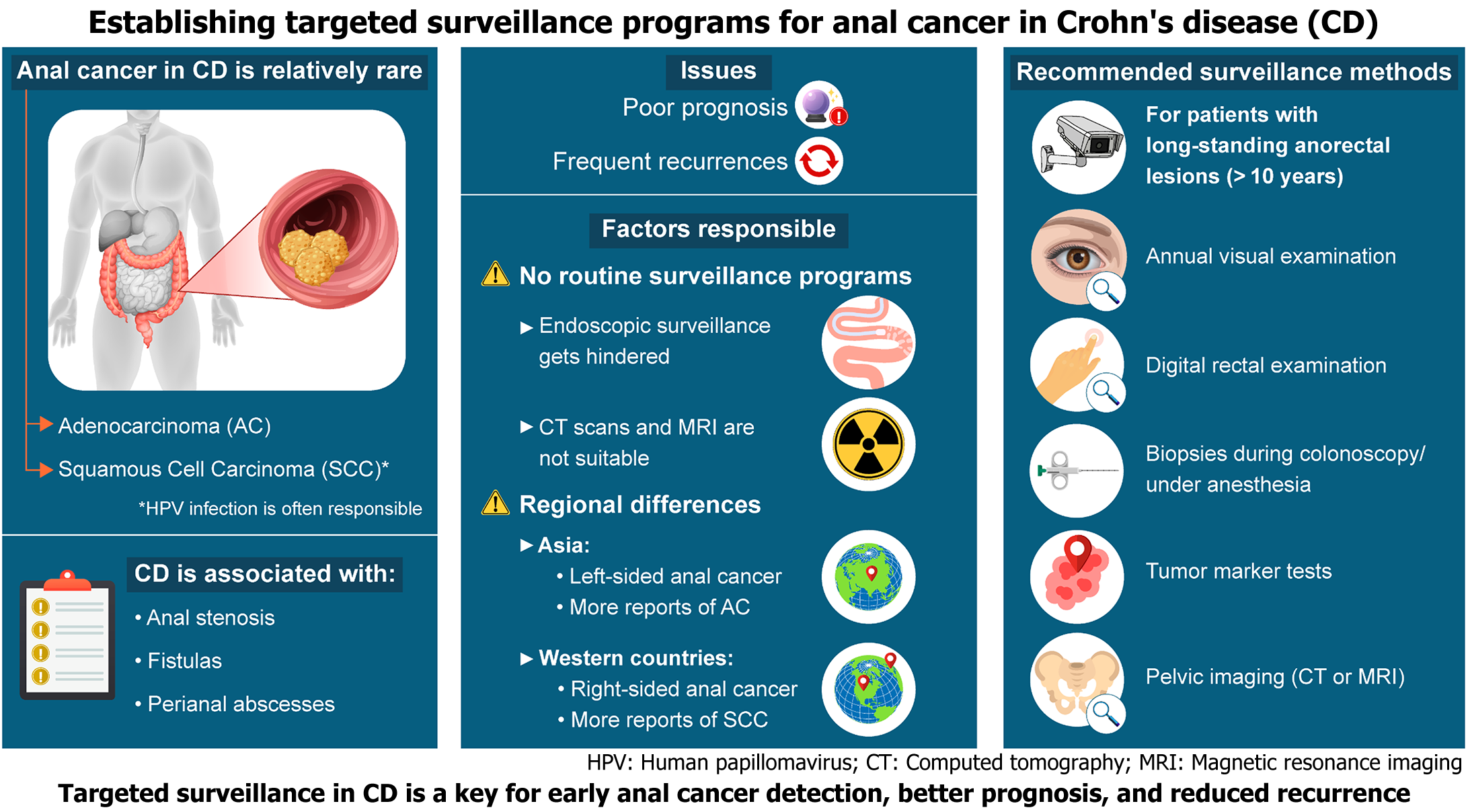
This letter discusses the incidence of anal cancer among Crohn's disease (CD)-related malignancies. Patients with CD have been demonstrated to be at a higher risk of developing small bowel and colorectal cancers than healthy individuals. Although CD-associated anal cancer is relatively rare, patients with CD accom
Core Tip: Patients with Crohn's disease (CD) are at a high risk of developing small and large bowel cancer. Regional differences exist in the prevalence of colorectal cancer, with more reports of right- and left-sided colorectal cancer in Western and Asian countries, respectively. The disease is detected at an advanced stage, and local recurrence is common, resulting in poor prognosis. Although surveillance programs have been established for ulcerative colitis, programs for colorectal cancer, especially anal cancer in CD, are lacking. Therefore, there is an imperative to focus on CD-related anal cancer and establish appropriate surveillance programs.
- Citation: Kayano H, Okada KI, Yamamoto S, Koyanagi K. Establishment of a surveillance program for anal cancer in Crohn's disease. World J Gastroenterol 2024; 30(45): 4844-4849
- URL: https://www.wjgnet.com/1007-9327/full/v30/i45/4844.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i45.4844
Inflammatory bowel disease (IBD) is a chronic and progressive inflammatory condition that affects the digestive tract and encompasses Crohn's disease (CD) and ulcerative colitis (UC). The exact cause of CD is unknown; however, it can lead to the formation of granulomatous inflammatory lesions with ulceration and fibrosis, which can occur anywhere in the gastrointestinal tract. Lesions may also occur outside the gastrointestinal tract, particularly in the skin. The anorectal region is frequently affected by conditions such as anal stenosis, skin tags, anal fissures, fistulas, and perianal abscesses, affecting 13%-30% of patients with CD over time[1]. With the advent of anti-tumor necrosis factor antibody biologics, such as infliximab and adalimumab, and human cell-processed therapeutic products, such as darvadstrocel, which have marked a significant advancement in IBD treatment, medical and surgical treatments have achieved a certain level of success[2-4]. However, patients with CD have a higher risk of developing small bowel and colorectal cancers than healthy individuals[5]. Furthermore, the prevalence of colorectal cancer varies by region; right-sided colorectal cancer is more common in Western countries, whereas left-sided colorectal cancer, especially rectal/anal canal and anal cancers, is predominant in Asian countries[6,7]. Although cases of CD-associated anal cancer are relatively rare, patients with CD accompanied by anal or perianal lesions have been suggested to be at an increased risk of anal cancer[8]. CD-related anal cancer is associated with a high incidence of local recurrence and poor prognosis[9]. However, the surveillance methods for CD-related malignancies recommended in the United States and Europe[10] are similar to those for UC. They are thus unsuitable for detecting CD-related malignancies in the recto-anal region, which has a different pathogenesis from that of UC. Therefore, there is an urgent need for surveillance programs aimed at the early detection of malignant anorectal lesions in patients with CD[11] (Figure 1). This editorial focuses on CD-associated anal cancer and summarizes the diagnostic methods, existing surveillance programs, treatments, and epidemiology to facilitate the establishment of a suitable surveillance program for CD-related malignancies.
Risk factors for colorectal cancer complications in CD include early disease onset, prolonged CD duration, extensive colon involvement, and an empty bowel tube due to a stoma. A long-term history of perianal fistula (> 10 years) has been exclusively associated with anal cancer[8,12]. The carcinogenic rate in patients with perianal CD is less than 1%[13], with cancer primarily arising from perianal fistulas. In patients with long-term stenosis, fistula, or other rectoanal lesions, warning signs of carcinogenesis include "clinical changes" such as hemorrhage, appearance or worsening of symptoms of rectoanal stenosis, pain, induration, the appearance of a mass, and mucus discharge from the fistula tube that was not present previously. The histological types of anal cancer are broadly classified into adenocarcinoma (AC) and squamous cell carcinoma (SCC), with AC being the most common type of anal cancer in CD, followed by SCC[14]. However, there are regional differences, with more reports of SCC and AC in Western and Asian countries, respectively[7,14,15]. AC may arise from the columnar epithelial lining of the fistula or via epithelial-mesenchymal transition within a longstanding Crohn's fistula[16]. Furthermore, in patients with SCC, an association with human papillomavirus (HPV) has been confirmed in CD[12], similar to the strong association between anal cancer and infection with HPV types 16 and 18[17].
The importance of surveillance endoscopy has been advocated in patients with IBD. For patients with UC, most cancers are diagnosed by surveillance; however, only 25% of CD-related cancers are diagnosed by surveillance, with more than half being diagnosed by symptom-driven testing[18]. In UC, cancer surveillance by endoscopy is well-established, cost-effective, and improves prognosis by increasing the number of early-stage diagnoses; however, endoscopy presents challenges in patients with CD owing to the presence of fistulas and stenotic lesions. Pelvic computed tomography (CT) and magnetic resonance imaging (MRI) are useful for assessing the extent of the disease, invasion into the surrounding organs, and lymph node metastasis; however, they are not effective for surveillance. Although CT is easy to perform, it carries risks associated with radiation exposure and incurs a financial burden, which affects the cost-benefit ratio. Furthermore, 18F-fluorodeoxyglucose positron emission tomography-CT scans are not very effective for surveillance because of their low accuracy in detecting mucinous carcinoma (41% to 58%)[19], which is common in anal cancer[20], and inflammation can also lead to false-positive results. Conversely, perianal observation under anesthesia has been useful for patients with perianal pain and stenotic perianal lesions[15,21]. In Japan, rectal canal and anal cancer are common in CD cases; thus, patients with long-lasting anorectal lesions, such as anal fistula, including fecal diversion, and those with clinical changes, such as bleeding, stricture, pain, and increased mucus secretion, should undergo rectal and anal examinations, cytological tests of the secretions, biopsy during colonoscopy or under anesthesia, tumor marker tests, and pelvic CT and MRI. The cancer surveillance program is specifically designed for patients who have had CD for > 10 years and have ulcers, stenosis, anal fistulas, or other lesions in the rectum, anal canal, or anus, or those who have undergone fecal diversion. As a rule, the following tests should be performed annually for cancer surveillance regardless of the presence or absence of clinical symptoms. If malignancy is suspected, the examination should be repeated as appropriate: (1) Visual examination, palpation, or digital rectal examination; (2) Biopsy by colonoscopy: Biopsies are performed under general or lumbar anesthesia in cases of severe stenosis. Cytological diagnosis should be performed in patients with mucus secretion; (3) For anal fistulas, biopsy, and cytology should be performed during outpatient consultation whenever possible, using curettage, biopsy, or brushing under local anesthesia. If this is difficult, a biopsy should be performed under general or lumbar anesthesia. Similarly, cytological tests should be performed in cases of mucus secretion. Curettage and biopsy of anal fistulas should be performed under local anesthesia (or general or lumbar anesthesia if necessary); (4) Tumor markers, including carcinoembryonic antigen, carbohydrate antigen 19-9, and SCC antigen, should be measured during biopsy and cytology; and (5) A pelvic CT scan or MRI should be performed if available[22].
Surgery is the standard of care for AC, and abdominoperineal rectal resection (APR) is the mainstay of treatment. In CD, several cases of invasion into the peri-rectal tissue have been reported, which lead to difficulty in securing negative surgical dissection margins, resulting in cancerous remnants. In such cases, total pelvic exenteration may be performed to secure dissection margins. Extensive perineal resection is often required simultaneously. Additionally, many cancers are diagnosed at an advanced stage, necessitating multidisciplinary treatment, including preoperative or postoperative chemotherapy. However, radiation therapy may be poorly tolerated in patients with CD accompanied by active perianal disease, rendering surgery the preferred treatment option[13,23]. For patients with SCC, radical surgery with abdominoperineal rectal amputation was the standard treatment previously. However, in 1974, chemoradiotherapy was demonstrated to have overall and disease-free survival rates comparable to surgery[24], and the combination of radiation therapy and chemotherapy has been associated with a higher disease-free survival rate and lower local recurrence rate than radiation therapy alone[25]. Therefore, combination chemoradiation is currently the standard of care for patients with SCC. Additionally, for patients with anal stenosis or perianal inflammation who undergo colostomy and for whom screening and surveillance are difficult, early APR is conducted based on symptoms alone before advanced cancer is diagnosed[26].
Anal cancer in CD has a poorer prognosis than anal cancer in healthy individuals, regardless of AC or SCC histology[27-29]. Patients with symptoms tend to have a poorer prognosis than those without symptoms[9,15]. CD is also associated with a poorer prognosis than UC, which has an established surveillance program[18,30]. This poor prognosis may be attributed to the delayed diagnosis of CD owing to the complexity of its pathogenesis.
To have a significant impact on cancer treatment, it is important to establish surveillance programs that can detect cancer in its early stages. It is equally important to research prevention strategies to avoid cancer incidence. HPV is associated with the development of SCC and is often detected in cervical, oropharyngeal, oral, and anal SCC[31]. Growing evidence suggests that oncogenic HPV types (especially subtypes 16 and 18) are etiologically associated with the development of anal canal SCC. Conversely, HPV positivity and/or p16 positivity has been shown to improve overall survival rates in patients with anal canal SCC[32]. Patients with CD with a history of long-term perianal fistula (> 10 years) are at an increased risk of anal cancer[8,12]. This patient population has also been reported to have a high rate of HPV positivity[33]. Anal cancer develops from HPV infection through persistent infection and precursor lesions. Therefore, prevention of anal cancer using HPV vaccines has gained significant attention. Thus, the latest guidelines from the European Crohn's and Colitis Organization on opportunistic infections recommend HPV vaccination for young adults with IBD regardless of sex[34].
Among the inflammatory diseases, UC has a well-established surveillance system for related malignancies. However, CD is more complex, and surveillance for related malignancies has not yet been established. Therefore, it is imperative to establish a system for CD-related malignancies. Currently, patients with long-standing (> 10 years) anorectal lesions should undergo periodic biopsy and imaging studies, and if clinical symptoms change, repeated examinations should be performed to rule out the possibility of cancer.
| 1. | Zhao M, Lo BZS, Vester-Andersen MK, Vind I, Bendtsen F, Burisch J. A 10-Year Follow-up Study of the Natural History of Perianal Crohn's Disease in a Danish Population-Based Inception Cohort. Inflamm Bowel Dis. 2019;25:1227-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 2. | Gu B, Venkatesh K, Williams AJ, Ng W, Corte C, Gholamrezaei A, Ghaly S, Xuan W, Paramsothy S, Connor S. Higher infliximab and adalimumab trough levels are associated with fistula healing in patients with fistulising perianal Crohn's disease. World J Gastroenterol. 2022;28:2597-2608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 3. | Vasudevan A, Bruining DH, Loftus EV Jr, Faubion W, Ehman EC, Raffals L. Approach to medical therapy in perianal Crohn's disease. World J Gastroenterol. 2021;27:3693-3704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (3)] |
| 4. | Zabot GP, Cassol O, Saad-Hossne R, Bemelman W. Modern surgical strategies for perianal Crohn's disease. World J Gastroenterol. 2020;26:6572-6581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Olén O, Erichsen R, Sachs MC, Pedersen L, Halfvarson J, Askling J, Ekbom A, Sørensen HT, Ludvigsson JF. Colorectal cancer in Crohn's disease: a Scandinavian population-based cohort study. Lancet Gastroenterol Hepatol. 2020;5:475-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 139] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 6. | von Roon AC, Reese G, Teare J, Constantinides V, Darzi AW, Tekkis PP. The risk of cancer in patients with Crohn's disease. Dis Colon Rectum. 2007;50:839-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 211] [Article Influence: 11.7] [Reference Citation Analysis (1)] |
| 7. | Higashi D, Katsuno H, Kimura H, Takahashi K, Ikeuchi H, Kono T, Nezu R, Hatakeyama K, Kameyama H, Sasaki I, Fukushima K, Watanabe K, Kusunoki M, Araki T, Maeda K, Kameoka S, Itabashi M, Nakao S, Maeda K, Ohge H, Watadani Y, Watanabe T, Sunami E, Hotokezaka M, Sugita A, Funayama Y, Futami K. Current State of and Problems Related to Cancer of the Intestinal Tract Associated with Crohn's Disease in Japan. Anticancer Res. 2016;36:3761-3766. [PubMed] |
| 8. | Beaugerie L, Carrat F, Nahon S, Zeitoun JD, Sabaté JM, Peyrin-Biroulet L, Colombel JF, Allez M, Fléjou JF, Kirchgesner J, Svrcek M; Cancers et Surrisque Associé aux Maladies Inflammatoires Intestinales En France Study Group. High Risk of Anal and Rectal Cancer in Patients With Anal and/or Perianal Crohn's Disease. Clin Gastroenterol Hepatol. 2018;16:892-899.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 82] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 9. | Ogino T, Mizushima T, Fujii M, Sekido Y, Eguchi H, Nezu R, Ikeuchi H, Motoi U, Futami K, Okamoto K, Nagahara H, Watanabe K, Okabayashi K, Yamada K, Ohge H, Tanaka S, Mizuuchi Y, Ohkita Y, Sato Y, Ueno H, Kono T, Itabashi M, Kimura H, Hida K, Kinugasa Y, Takahashi K, Koyama F, Hanai T, Maeda K, Noake T, Shimada Y, Yamamoto T, Arakaki J, Mastuda K, Okuda J, Sunami E, Akagi Y, Kastumata K, Uehara K, Yamada T, Sasaki S, Ishihara S, Ajioka Y, Sugihara K; Study Group for Inflammatory Bowel Disease Associated Intestinal Cancers by the Japanese Society for Cancer of the Colon and Rectum. Crohn's Disease-Associated Anorectal Cancer Has a Poor Prognosis With High Local Recurrence: A Subanalysis of the Nationwide Japanese Study. Am J Gastroenterol. 2023;118:1626-1637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 10. | Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE. ACG Clinical Guideline: Management of Crohn's Disease in Adults. Am J Gastroenterol. 2018;113:481-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 924] [Article Influence: 132.0] [Reference Citation Analysis (0)] |
| 11. | Pacheco T, Monteiro S, Barros L, Silva J. Perianal disease in inflammatory bowel disease: Broadening treatment and surveillance strategies for anal cancer. World J Gastroenterol. 2024;30:3373-3385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (2)] |
| 12. | Ruel J, Ko HM, Roda G, Patil N, Zhang D, Jharap B, Harpaz N, Colombel JF. Anal Neoplasia in Inflammatory Bowel Disease Is Associated With HPV and Perianal Disease. Clin Transl Gastroenterol. 2016;7:e148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Shwaartz C, Munger JA, Deliz JR, Bornstein JE, Gorfine SR, Chessin DB, Popowich DA, Bauer JJ. Fistula-Associated Anorectal Cancer in the Setting of Crohn's Disease. Dis Colon Rectum. 2016;59:1168-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Thomas M, Bienkowski R, Vandermeer TJ, Trostle D, Cagir B. Malignant transformation in perianal fistulas of Crohn's disease: a systematic review of literature. J Gastrointest Surg. 2010;14:66-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Hirano Y, Futami K, Higashi D, Mikami K, Maekawa T. Anorectal cancer surveillance in Crohn's disease. J Anus Rectum Colon. 2018;2:145-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Scharl M, Frei P, Frei SM, Biedermann L, Weber A, Rogler G. Epithelial-to-mesenchymal transition in a fistula-associated anal adenocarcinoma in a patient with long-standing Crohn's disease. Eur J Gastroenterol Hepatol. 2014;26:114-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 17. | Machalek DA, Poynten M, Jin F, Fairley CK, Farnsworth A, Garland SM, Hillman RJ, Petoumenos K, Roberts J, Tabrizi SN, Templeton DJ, Grulich AE. Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men: a systematic review and meta-analysis. Lancet Oncol. 2012;13:487-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 796] [Cited by in RCA: 717] [Article Influence: 55.2] [Reference Citation Analysis (0)] |
| 18. | Noguchi T, Ishihara S, Uchino M, Ikeuchi H, Okabayashi K, Futami K, Tanaka S, Ohge H, Nagahara H, Watanabe K, Itabashi M, Okamoto K, Okita Y, Mizushima T, Mizuuchi Y, Yamada K, Shimada Y, Sato Y, Kimura H, Takahashi K, Hida K, Kinugasa Y, Okuda J, Daito K, Koyama F, Ueno H, Yamamoto T, Hanai T, Maemoto A, Oba K, Ajioka Y, Sugihara K; Study Group for Inflammatory Bowel Disease Associated Intestinal Cancers by the Japanese Society for Cancer of the Colon, Rectum. Clinical features and oncological outcomes of intestinal cancers associated with ulcerative colitis and Crohn's disease. J Gastroenterol. 2023;58:14-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 19. | Whiteford MH, Whiteford HM, Yee LF, Ogunbiyi OA, Dehdashti F, Siegel BA, Birnbaum EH, Fleshman JW, Kodner IJ, Read TE. Usefulness of FDG-PET scan in the assessment of suspected metastatic or recurrent adenocarcinoma of the colon and rectum. Dis Colon Rectum. 2000;43:759-767; discussion 767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 174] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 20. | Uchino M, Ikeuchi H, Noguchi T, Okabayashi K, Futami K, Tanaka S, Ohge H, Watanabe K, Itabashi M, Okamoto K, Okita Y, Mizushima T, Mizuuchi Y, Yamada K, Shimada Y, Sato Y, Kimura H, Takahashi K, Hida K, Kinugasa Y, Okuda J, Daito K, Koyama F, Ueno H, Yamamoto T, Hanai T, Kono T, Kobayashi H, Ajioka Y, Sugihara K, Ishihara S; Study Group for Inflammatory Bowel Disease Associated Intestinal Cancers of the Japanese Society for Cancer of the Colon and Rectum. Histological differentiation between sporadic and colitis-associated intestinal cancer in a nationwide study: A propensity-score-matched analysis. J Gastroenterol Hepatol. 2024;39:893-901. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Matsuno H, Mizushima T, Nezu R, Nakajima K, Takahashi H, Haraguchi N, Nishimura J, Hata T, Yamamoto H, Doki Y, Mori M. Detection of Anorectal Cancer among Patients with Crohn's Disease Undergoing Surveillance with Various Biopsy Methods. Digestion. 2016;94:24-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Sugita A, Koganei K, Tatsumi K, Yamada K, Futatsuki R, Kuroki H, Kimura H, Kito F, Fukushima T. [Gastrointestinal malignancies with Crohn’s disease]. Stomach Intest. 2012;47:1537-1544. |
| 23. | Lightner AL, Moncrief SB, Smyrk TC, Pemberton JH, Haddock MG, Larson DW, Dozois EJ, Mathis KL. Long-standing Crohn's disease and its implication on anal squamous cell cancer management. Int J Colorectal Dis. 2017;32:661-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Nigro ND, Vaitkevicius VK, Buroker T, Bradley GT, Considine B. Combined therapy for cancer of the anal canal. Dis Colon Rectum. 1981;24:73-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 115] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Epidermoid anal cancer: results from the UKCCCR randomised trial of radiotherapy alone versus radiotherapy, 5-fluorouracil, and mitomycin. UKCCCR Anal Cancer Trial Working Party. UK Co-ordinating Committee on Cancer Research. Lancet. 1996;348:1049-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 824] [Cited by in RCA: 715] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 26. | Kuroki H, Sugita A, Koganei K, Tatsumi K, Futatsuki R, Nakao E, Obara N, Arai K. Clinicopathological and prognostic evaluations of anorectal cancer after fecal diversion for patients with Crohn's disease. BMC Gastroenterol. 2021;21:168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 27. | Slesser AA, Bhangu A, Bower M, Goldin R, Tekkis PP. A systematic review of anal squamous cell carcinoma in inflammatory bowel disease. Surg Oncol. 2013;22:230-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 28. | Iesalnieks I, Gaertner WB, Glass H, Strauch U, Hipp M, Agha A, Schlitt HJ. Fistula-associated anal adenocarcinoma in Crohn's disease. Inflamm Bowel Dis. 2010;16:1643-1648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 29. | Benjelloun el B, Abkari M, Ousadden A, Ait Taleb K. Squamous cell carcinoma associated anal fistulas in Crohn's disease unique case report with literature review. J Crohns Colitis. 2013;7:e232-e235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Higashi D, Irie H, Maki T, Kusaba H, Koreeda N, Hirano Y, Kaida H, Kawamoto M, Komono A, Takahashi H, Sakamoto R, Shibata R, Miyasaka Y, Hisabe T, Nimura S, Watanabe M. Small and large intestinal cancer in patients with Crohn's disease studied by surgeons. Surg Today. 2023;53:675-680. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 31. | Vonsky M, Shabaeva M, Runov A, Lebedeva N, Chowdhury S, Palefsky JM, Isaguliants M. Carcinogenesis Associated with Human Papillomavirus Infection. Mechanisms and Potential for Immunotherapy. Biochemistry (Mosc). 2019;84:782-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 32. | Benson AB, Venook AP, Al-Hawary MM, Azad N, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D, Garrido-Laguna I, Grem JL, Hecht JR, Hoffe S, Hubbard J, Hunt S, Hussan H, Jeck W, Johung KL, Joseph N, Kirilcuk N, Krishnamurthi S, Maratt J, Messersmith WA, Meyerhardt J, Miller ED, Mulcahy MF, Nurkin S, Overman MJ, Parikh A, Patel H, Pedersen K, Saltz L, Schneider C, Shibata D, Skibber JM, Sofocleous CT, Stotsky-Himelfarb E, Tavakkoli A, Willett CG, Williams G, Algieri F, Gurski L, Stehman K. Anal Carcinoma, Version 2.2023, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2023;21:653-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 33. | Boarini LR, Sobrado CW, Mota GR, Villa LL, de Albuquerque IC, Queiroz NSF, Facanali CBG, Nadal SR, Cecconello I. Perianal fistulizing Crohn's disease is associated with a higher prevalence of HPV in the anorectal fistula tract. A comparative study. Clinics (Sao Paulo). 2023;78:100219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 34. | Kucharzik T, Ellul P, Greuter T, Rahier JF, Verstockt B, Abreu C, Albuquerque A, Allocca M, Esteve M, Farraye FA, Gordon H, Karmiris K, Kopylov U, Kirchgesner J, MacMahon E, Magro F, Maaser C, de Ridder L, Taxonera C, Toruner M, Tremblay L, Scharl M, Viget N, Zabana Y, Vavricka S. ECCO Guidelines on the Prevention, Diagnosis, and Management of Infections in Inflammatory Bowel Disease. J Crohns Colitis. 2021;15:879-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 260] [Article Influence: 65.0] [Reference Citation Analysis (32)] |