Published online Nov 21, 2024. doi: 10.3748/wjg.v30.i43.4677
Revised: September 29, 2024
Accepted: October 11, 2024
Published online: November 21, 2024
Processing time: 74 Days and 17.1 Hours
Despite advancements in the field, early diagnosis of multiple endocrine neo
Core Tip: Early diagnosis of multiple endocrine neoplasia type 1 (MEN1) is critical for effective management and improved outcomes. This letter underscored the importance of considering MEN1 in patients presenting with recurrent gastrointestinal symptoms, hypercalcemia, and elevated serum gastrin levels. The discussed case demonstrated how a comprehensive diagnostic approach, including imaging studies and blood tests, can lead to timely surgical intervention and accurate diagnosis. Clinicians should remain vigilant for MEN1 in patients with persistent or recurrent symptoms, facilitating early detection and treatment.
- Citation: Velikova T, Lazarov V. Improving early diagnosis of multiple endocrine neoplasia type 1 by assessing the gastrointestinal symptoms, hypercalcemia, and elevated serum gastrin. World J Gastroenterol 2024; 30(43): 4677-4681
- URL: https://www.wjgnet.com/1007-9327/full/v30/i43/4677.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i43.4677
We were delighted to read the high-quality case-based article by Yuan et al[1] published in the World Journal of Gastroenterology. The main focus of this article was the early detection of multiple endocrine neoplasia (MEN) type 1. The authors presented a case report of a patient in whom MEN1 was detected early. At the same time, the presenting symptoms were recurrent abdominal pain and diarrhea. After performing computed tomography of the parathyroid glands (demon
The latest research by Yuan et al[1] raised important questions regarding the challenges in MEN1 diagnostics and why it usually takes several years. MEN1 is a rare genetic disorder that affects approximately 1 in 30000 individuals. This condition is inherited in an autosomal dominant manner, meaning that a single copy of the altered gene in each cell is sufficient to cause the disorder. MEN1 affects males and females equally and shows no significant geographical, racial, or ethnic preferences[2].
MEN1 is characterized by the development of tumors in multiple endocrine glands. The most common types of tumors associated with MEN1 include: Parathyroid tumors, which lead to primary hyperparathyroidism and elevated calcium levels in the blood; pituitary tumors, which can produce excess hormones resulting in conditions such as prolactinoma, acromegaly, or Cushing’s disease; and pancreatic NETs, which can produce hormones like insulin, gastrin, and glucagon, leading to clinical syndromes such as Zollinger-Ellison syndrome or insulinoma. Additionally, MEN1 can also involve less common tumors in the adrenal glands, thymus, and bronchial tubes[3]. Diagnosing MEN1 involves a combination of clinical evaluation, biochemical tests, imaging studies, and genetic testing[4]. Since MEN1 is an autosomal dominant inherited syndrome caused by germline mutations in the MEN1 gene that predisposes carriers to variable risk of development of tumors in diverse non-endocrine and endocrine organs, most MEN1 carriers develop main tumors between 5 years and 80 years with at least one initiating around 20-30 years (50%-60%), and invariably 94% of MEN1 carriers have developed one or more disease manifestations at the age of 50 years[5].
The process typically begins with a thorough clinical evaluation where a healthcare provider assesses symptoms and conducts physical examinations to identify signs of endocrine tumors. Biochemical tests are then performed to measure hormone levels in the blood, such as calcium, prolactin, and gastrin, which can indicate the presence of endocrine tumors. Imaging studies, including magnetic resonance imaging, computed tomography scans, and ultrasound, visualize tumors in the endocrine glands. Finally, genetic testing is conducted to identify mutations in the MEN1 gene, which can confirm the diagnosis, especially in individuals with a family history of the disorder. This comprehensive approach ensures accurate diagnosis and helps plan appropriate management and treatment strategies for patients with MEN1[6].
Clinical practice guidelines for MEN1 diagnosis from 2021 by Thakker et al[7] on behalf of the Endocrine Society was further discussed for updates by Newey and Newell-Price in 2022[2]. Current recommendations advise a rigorous clinical, biochemical, and radiological monitoring program starting in early childhood for individuals with a clinical or genetic diagnosis of MEN1, aiming for early detection and treatment of tumors. While it may be assumed that such screening improves patient outcomes, there is limited strong evidence supporting several aspects of MEN1 management. Additionally, there are potential risks from unnecessary interventions or tests that lack proven benefits. The psychological and financial impacts of intensive screening remain largely unexplored. Although screening is crucial in MEN1 care, this perspective emphasizes the uncertainties and challenges surrounding current guidelines, particularly regarding the detection of presymptomatic tumors. A future approach that considers these limitations and actively involves patients in decision-making is recommended. In line with this, differential diagnoses of MEN1 include Von Hippel-Lindau syndr
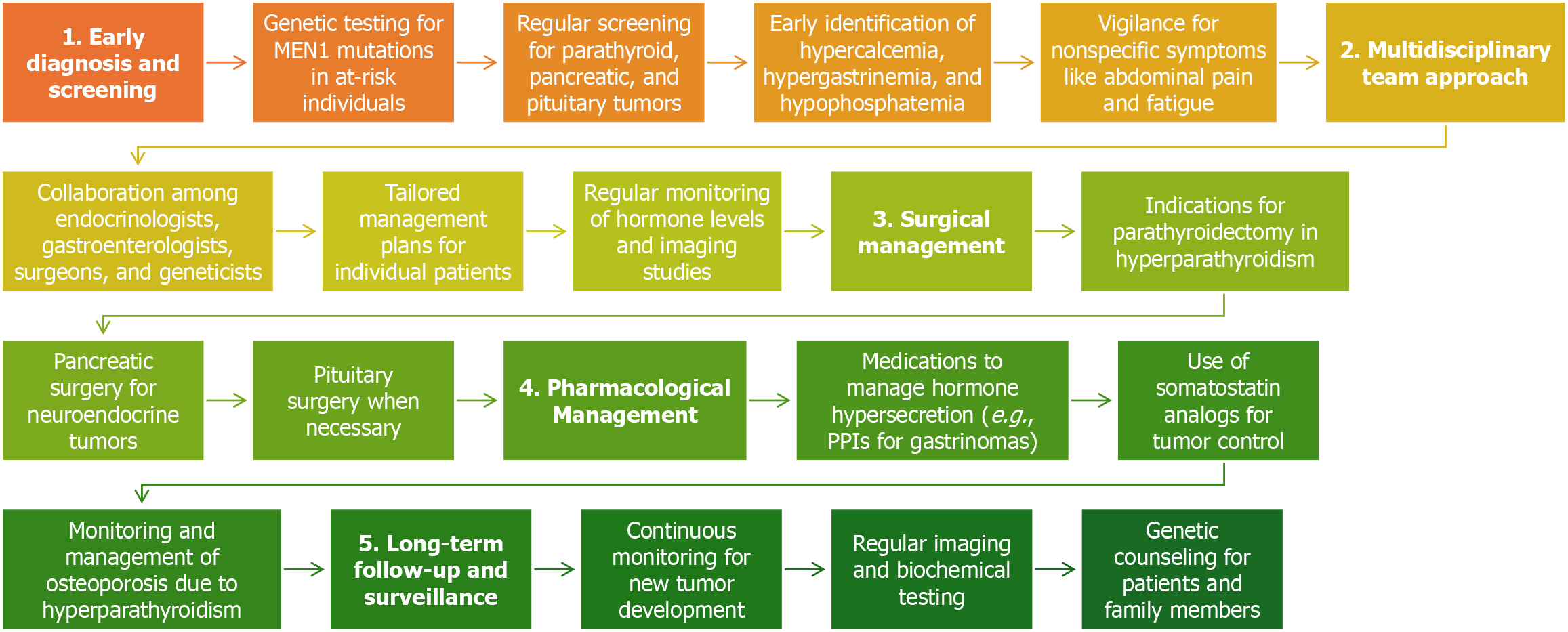
Therapy for MEN1 focuses on managing the symptoms and complications caused by the various tumors associated with the disorder. This often requires a multidisciplinary approach involving different medical specialties to address the diverse manifestations of MEN1[6].
Surgery is a primary treatment option for many MEN1-related tumors. For instance, parathyroidectomy is commonly performed to treat hyperparathyroidism caused by parathyroid tumors. Similarly, surgical removal of pancreatic NETs and pituitary tumors may be necessary to control hormone overproduction and alleviate symptoms[9].
Medications play a crucial role in managing hormone levels and symptoms. For example, proton pump inhibitors can reduce stomach acid production in gastrinoma patients, while medications like dopamine agonists can help control prolactin levels in patients with prolactinomas. Hormone replacement therapy may also be required if endocrine glands are removed or damaged during surgery[10].
Radiation therapy may be employed for certain types of tumors, such as pituitary adenomas, particularly when surgery is not feasible or if the tumor recurs after surgery. This approach helps to shrink the tumors and control hormone production[11].
Regular monitoring is essential for patients with MEN1 due to the risk of developing new tumors over time. Lifelong surveillance, including periodic biochemical tests and imaging studies, is necessary to detect any new or recurrent tumors early and effectively manage existing ones. Managing MEN1 presents several difficulties and challenges (Figure 1). One of the primary challenges is early detection. Since MEN1 can cause a variety of tumors in different endocrine glands, regular and comprehensive screening is essential but can be burdensome for patients. Early detection is critical to prevent complications, but the need for frequent monitoring can be stressful and time-consuming[12].
Genetic counseling is another significant challenge. Given the hereditary nature of MEN1, genetic counseling is essential for affected families to understand the risks and implications of the disorder. However, the psychological impact of genetic testing and the potential for discovering that other family members are at risk can be profound and complex to manage[13].
Treatment complications also pose a challenge. Surgical and medical treatments for MEN1-related tumors can have significant side effects and complications. For example, parathyroid surgery can lead to hypocalcemia (low calcium levels), and managing hormone levels with medications can be complex and require careful monitoring to avoid adverse effects[8].
Quality of life is a significant concern for patients with MEN1. The chronic nature of the disorder, the need for ongoing treatment, and the constant monitoring can significantly impact the quality of life for patients and their families. The psychological burden of living with a genetic disorder that predisposes individuals to multiple tumors can be substantial[14].
In summary, while advances in genetic testing and treatment options have improved outcomes for patients with MEN1, the disorder still presents significant challenges (Table 1) in terms of early detection, genetic counseling, treatment complications, and maintaining quality of life.
| Challenge | Description | Suggestions for improvement |
| Nonspecific symptoms | MEN1 often presents with vague symptoms like abdominal pain, diarrhea, and fatigue | Increase clinical awareness and consider MEN1 in differential diagnosis for patients with these symptoms |
| Overlap with common conditions | Symptoms such as hypercalcemia and gastrointestinal issues can be mistaken for more common diseases | Encourage routine screening for MEN1 markers in patients with persistent symptoms |
| Genetic testing accessibility | Limited access to genetic testing in some regions hinders early diagnosis | Expand genetic testing programs and offer counseling to at-risk individuals and their families |
| Delayed diagnosis | MEN1 diagnosis is often delayed due to its rarity and complex presentation | Implement standardized protocols for early screening and referral to specialized centers |
| Multisystem involvement | MEN1 affects multiple endocrine glands, complicating diagnosis, and management | Foster a multidisciplinary approach to care, involving endocrinologists, surgeons, and geneticists |
| Inconsistent surveillance practices | Variation in follow-up and surveillance across institutions | Establish uniform guidelines for ongoing monitoring and management of patients with MEN1 |
| Psychosocial impact | The diagnosis of MEN1 can lead to significant psychological stress for patients | Provide mental health support and counseling services as part of comprehensive care |
In line with this, Yuan et al[1], by providing a case report of a patient exhibiting nonspecific gastrointestinal symptoms, hypercalcemia, and elevated serum gastrin levels, raised awareness for diagnosing MEN1 within just 1 year from the onset of such symptoms. Given that MEN1 can present with a variety of clinical symptoms and is often misdiagnosed, it is crucial to consider MEN1 as a possibility in patients with gastrointestinal symptoms, particularly if symptoms reoccur after discontinuing proton pump inhibitors. Early suspicion, diagnosis, and treatment are essential in improving patient outcomes.
This case underscored the importance of considering MEN1 in patients presenting with recurrent gastrointestinal symptoms, hypercalcemia, and elevated serum gastrin levels, even when these symptoms overlap with more common conditions. By raising clinical suspicion for MEN1 in such cases, earlier diagnosis and intervention can be achieved, potentially preventing disease progression. Incorporating this diagnostic approach into routine clinical practice may lead to earlier detection of MEN1-associated tumors, altering the current reliance on later-stage diagnosis and improving long-term outcomes through timely treatment.
Early diagnosis of MEN1 remains a significant challenge due to its diverse and often nonspecific clinical presentation. The discussed case highlighted how gastrointestinal symptoms, when combined with hypercalcemia and elevated serum gastrin levels, should prompt consideration of MEN1. However, the overlap of these symptoms with more common conditions often leads to delays in diagnosis. This underscores the need for heightened clinical awareness and a thorough, multidisciplinary approach to evaluation. By recognizing the potential for MEN1 early in the diagnostic process, clinicians can improve outcomes through timely intervention. Yet, the rarity and variability of the condition demand ongoing vigilance and education in the medical community.
Moreover, this case emphasized the importance of integrating MEN1 into the differential diagnosis of gastrointestinal symptoms, especially in the presence of biochemical abnormalities like hypercalcemia and elevated gastrin. This approach may refine clinical guidelines by encouraging earlier genetic screening and imaging in patients with similar symptom clusters. Additionally, by adopting a proactive stance in identifying MEN1, this case supported the call for further research on cost-effective diagnostic strategies that can mitigate the economic burden of intensive surveillance without compromising early detection. Ongoing education and updated clinical guidelines that stress the importance of early recognition may lead to improved management and patient outcomes.
| 1. | Yuan JH, Luo S, Zhang DG, Wang LS. Early detection of multiple endocrine neoplasia type 1: A case report. World J Gastroenterol. 2024;30:3247-3252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 2. | Newey PJ, Newell-Price J. MEN1 Surveillance Guidelines: Time to (Re)Think? J Endocr Soc. 2022;6:bvac001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | de Laat JM, van Leeuwaarde RS, Valk GD. The Importance of an Early and Accurate MEN1 Diagnosis. Front Endocrinol (Lausanne). 2018;9:533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Kamilaris CDC, Stratakis CA. Multiple Endocrine Neoplasia Type 1 (MEN1): An Update and the Significance of Early Genetic and Clinical Diagnosis. Front Endocrinol (Lausanne). 2019;10:339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 119] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 5. | Lourenço DM Jr, de Herder WW. Editorial: Early Genetic and Clinical Diagnosis in MEN1. Front Endocrinol (Lausanne). 2020;11:218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Pieterman CRC, Valk GD. Update on the clinical management of multiple endocrine neoplasia type 1. Clin Endocrinol (Oxf). 2022;97:409-423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Thakker RV, Newey PJ, Walls GV, Bilezikian J, Dralle H, Ebeling PR, Melmed S, Sakurai A, Tonelli F, Brandi ML; Endocrine Society. Clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1). J Clin Endocrinol Metab. 2012;97:2990-3011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 879] [Cited by in RCA: 882] [Article Influence: 67.8] [Reference Citation Analysis (0)] |
| 8. | Singh G, Mulji NJ, Jialal I. Multiple Endocrine Neoplasia Type 1. 2023 Jul 10. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 9. | van Beek DJ, Nell S, Verkooijen HM, Borel Rinkes IHM, Valk GD; (on behalf of the DutchMEN study group), Vriens MR; International MEN1 Insulinoma Study Group. Surgery for multiple endocrine neoplasia type 1-related insulinoma: long-term outcomes in a large international cohort. Br J Surg. 2020;107:1489-1499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. | Hu X, Guan J, Wang Y, Shi S, Song C, Li ZP, Feng ST, Chen J, Luo Y. A narrative review of multiple endocrine neoplasia syndromes: genetics, clinical features, imaging findings, and diagnosis. Ann Transl Med. 2021;9:944. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | van Vliembergen ENM, Eijkelenkamp H, Valk GD, Vriens MR, Meijer GJ, Intven MPW, de Laat JM. Precision radiotherapy using MR-linac for pancreatic neuroendocrine tumors in MEN1 patients (PRIME): a protocol for a phase I-II trial, and systematic review on available evidence for radiotherapy of pNETs. Front Endocrinol (Lausanne). 2023;14:994370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | Marini F, Giusti F, Tonelli F, Brandi ML. Management impact: effects on quality of life and prognosis in MEN1. Endocr Relat Cancer. 2017;24:T227-T242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Giusti F, Marini F, Brandi ML. Multiple Endocrine Neoplasia Type 1. 2005 Aug 31. In: GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–. [PubMed] |
| 14. | van Leeuwaarde RS, Pieterman CRC, May AM, Dekkers OM, van der Horst-Schrivers AN, Hermus AR, de Herder WW, Drent ML, Bisschop PH, Havekes B, Vriens MR, Valk GD. Health-Related Quality of Life in Patients with Multiple Endocrine Neoplasia Type 1. Neuroendocrinology. 2021;111:288-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |