Published online Nov 14, 2024. doi: 10.3748/wjg.v30.i42.4569
Revised: September 29, 2024
Accepted: October 12, 2024
Published online: November 14, 2024
Processing time: 149 Days and 6.4 Hours
This letter offers commentary on an article published in a recent issue of the World Journal of Gastroenterology. Hemorrhoidal artery embolization is a promising approach to severe hemorrhoidal bleeding treatment, but inappropriate patient selection and the use of different embolization procedures may affect the clinical efficacy and cause serious complications. In this article, the most appropriate candidate patients, embolization materials, embolization methods, and clinical evaluation methods are discussed to improve the safety and effectiveness of the procedure.
Core Tip: Hemorrhoidal artery embolization (Emborrhoid) is a promising nonsurgical technique for treating severe hemorrhoidal bleeding. The indications, contraindications, effectiveness, and safety of hemorrhoidal artery embolization should be considered to achieve better health outcomes.
- Citation: Lei ML, Dong LL, Zhang HP, Yu YB. Does hemorrhoidal artery embolization really benefit patients with hemorrhoids? World J Gastroenterol 2024; 30(42): 4569-4575
- URL: https://www.wjgnet.com/1007-9327/full/v30/i42/4569.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i42.4569
Hemorrhoidal artery embolization (Emborrhoid) is an effective method of treating bleeding hemorrhoids, preserving anal function, and relieving pain. As reported in their article “Transanal eco-Doppler evaluation after hemorrhoidal artery embolization", Tutino et al[1] conducted an observational study on 11 patients who underwent Emborrhoid. The data from that study suggest that Emborrhoid is a minimally invasive, effective, and relatively safe treatment approach. However, embolization is not effective in all patients, and some undesirable complications and failures are not uncommon. Thus, increasing the benefits conferred by Emborrhoid remains challenging.
For patients with symptomatic hemorrhoidal disease (HD), the current guidelines recommend dietary adjustments and behavioral therapy as the main first-line therapies[2]. Drug treatment can alleviate the clinical symptoms of HD to varying degrees[3]. The conventional excisional methods (Milligan–Morgan, Ferguson procedures) are still an effective treatment for symptomatic 2nd- and 3rd-degree hemorrhoids[4]. However, traditional excisional methods are limited by complications such as pain, bleeding, and fecal incontinence. Emborrhoid is currently available in clinical practice[5]. In a randomized clinical trial, the patients in the superior rectal artery (SRA) embolization group had clinical outcomes similar to those in the Ferguson closed hemorrhoidectomy surgical group, and the patients in the embolization group had relatively lower pain levels[6]. Regarding the short-term outcomes, Emborrhoid is a realistic, safe, and minimally invasive treatment for refractory symptomatic internal hemorrhoids[7].
There are currently no standard indications for Emborrhoid in patients experiencing chronic hemorrhoidal bleeding. It is a safe and effective technique for treating 2nd and 3rd-degree hemorrhoids, particularly in individuals who are not suitable candidates for surgery according to the guidelines provided by the Italian Society of Colorectal Surgery (level 2 evidence, grade C recommendation)[4]. These guidelines provide evidence-based recommendations; however, more studies are needed to determine the ideal candidates for this procedure. Emborrhoid may also be considered in patients with bleeding or surgical contraindications from 1st- or 4th-degree internal hemorrhoids[8,9]. Threatening rectal bleeding is a potential indication for the embolization of hemorrhoidal arteries[10]. Moreover, embolization is prioritized for patients with hemorrhoids who cannot tolerate surgery, have no prior history of surgery, do not have severe prolapse, want treatment, have been diagnosed with vascular abnormalities, or have other correlated factors. For people with severe heart disease and bleeding hemorrhoids, Emborrhoid may be an alternative option to consider[11]. Prior surgery can significantly alter the vascular anatomy, making it not conducive to treatment with embolization. Nonetheless, hemorrhoidal artery embolization remains an acceptable alternative for patients in whom prior surgeries failed[8,10]. Notably, Komekami et al[12] reported that rectal arteriovenous malformation (AVM) might be a cause of severe hemorrhage from internal hemorrhoids. Under these conditions, arterial embolization can safely be used to treat both bleeding hemorrhoids and AVMs at the same time. Notably, alternative causes of rectal bleeding, such as radiation proctitis, can be successfully treated with embolization[13]. We summarized the characteristics of the participants in the included studies (Table 1).
| Indications | Specific situations |
| Disabling rectal bleeding[10] | |
| Surgical contraindications[16] | Abnormal coagulation function anticoagulants, various acquired or genetic coagulation disorders (cirrhosis, protein S deficiency, haemophilia, etc.)[8,11,23] |
| Previous unsuccessful surgery[8,16] | |
| Poor cardiopulmonary function[34] | |
| No history of surgery[8,10] | |
| Vascular abnormalities | Rectal arteriovenous malformation[12] |
| Both hemorrhoidal disease and portal hypertension with rectal varices[35] | |
| No severe prolapse[8] | |
| Wishes of younger active patients[8], immunosuppressed patients[36] | |
| Pathological condition[15] | Morbid obesity, paraplegia |
Contraindications for endovascular treatment include severe renal impairment, contrast medium allergy, and the lack of vascular access. Other contraindications include acute hemorrhoid complications, chronic anal or perianal fissures, and colorectal cancer[5,14,15]. Emborrhoid in patients with inflammatory bowel disease remains controversial[15,16].
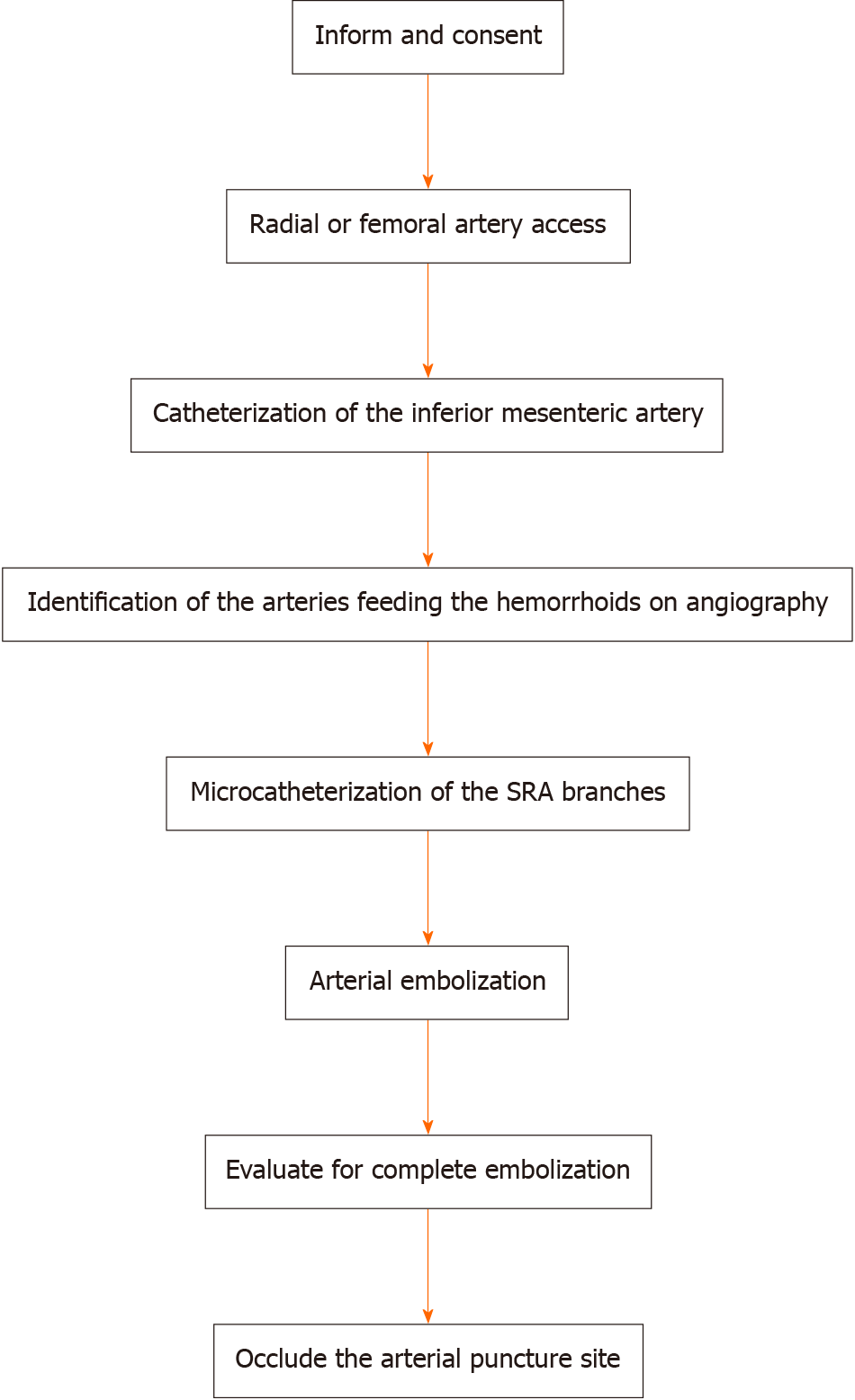
The hemorrhoid embolization technique has been previously described (Figure 1). Patients signed a consent form after they were informed of the benefits and risks of the embolization procedure. The embolization procedure was performed under local anesthesia through the right femoral or radial artery using a 5F introducer sheath. Selective angiography of the inferior mesenteric artery was subsequently performed with a Simmons catheter inserted through the vascular sheath. In most cases, the SRA branches were subsequently catheterized and superselected with a 2.4F or smaller microcatheter. Arterial embolization needs to consider choosing appropriate sites and materials. Complete embolization is defined as the absence of distal SRA branch flow and the absence of opacification of the terminal branches in the projection of the hemorrhoids. The extensive use of vascular closure devices helps achieve faster hemostasis and provides early ambulation to patients. Embolization via the transradial access is advantageous for outpatients because of its association with a low incidence of vascular complications, early ambulation, and short hospital stay[17].
Regarding the site of embolization, no generally accepted standards currently exist. Complete or incomplete embolization depends heavily on a comprehensive risk assessment of rebleeding or lack of bleeding[8]. Most studies did not report on the occurrence of ischemic complications[8,18]. Tradi et al[5] confirmed that the preservation of the upper branches feeding the anorectal wall and anastomoses can effectively prevent potential ischemic complications from occurring. However, additional studies with larger sample sizes and longer follow-up periods are needed to verify the long-term efficacy of these treatments. Vascular abnormalities increase the difficulty and risk of Emborrhoid. In a single-center retrospective study, Sun et al[19] concluded that embolization based on the connection between the SRA and the inferior rectal artery was an effective and safe method. Moussa et al[20] recommend embolization of the middle rectal artery as the first choice when the main blood supply appears to be from the middle rectal artery with a thin SRA. The need for internal iliac arteriography and embolization in patients whose branches of the internal iliac artery involve the blood supply to the hemorrhoidal area requires further exploration[21].
Currently, there are several types of embolic agents, each with its own advantages and disadvantages (Table 2). Zakharchenko et al[22] reported that embolization with particles is more effective at controlling hemorrhoid symptoms than embolization with coils. Theoretically, embolization with particles has a greater likelihood of clinical success and clinical benefit but is linked to a higher risk of ischemic complications than coil embolization[23]. However, there was no discernible difference in the clinical success rate between coil embolization and coil embolization combined with particle embolization in some studies[20]. Moreover, the radiation dose significantly increased as the procedure time for combined embolization with particles and coils increased[15]. Recent clinical studies have shown that gelfoam particles have similar short-term efficacy compared to polyvinyl alcohol (PVA) microparticles[24]. Importantly, PVA particles are permanent embolic materials that can occlude the distal branch of the SRA. Although PVA embolization can prevent the collateral circulation from causing secondary bleeding, it theoretically increases the risk of intestinal ischemic necrosis[21]. The clinical outcomes are better when larger particles (900–1200 μm) are used than when smaller particles are used[25]. In addition, the safety of using liquid embolic materials requires further study[26].
| Embolic materials | Advantages | Disadvantages |
| Microcoils | Easy to identify under fluoroscopy[37] | Dependent on a normal coagulation status[38] |
| Mild adverse reactions[29] | A non-distal embolization[8] | |
| Slow symptom relief[22] | ||
| Particles | Occluding the distal branches[22] | Particulate reflux[38] |
| Higher clinical success rates[23] | An increased risk of local ischemic complications[23] | |
| Liquid embolic materials | A high hemostasis effect with a low recurrent bleeding rate[38] | Vascular glue penetration can be difficult to control[38] |
| Unwanted retrograde flow or reflux[39] | ||
| Possibility of ischemic complications[26] |
Through advances in technology and materials, embolization devices and new embolic materials have been developed and improved to overcome these limitations. At the 3-month follow-up, most patients with cirrhotic portal hypertension (4 out of 5) showed clinically relevant improvement due to the release of oversized coils in a stretched fashion (“spaghetti technique”)[23]. A new electric detachable microcoil has been shown to be effective[27].
The incidence of complications is low, and these complications have no significant effect on prognosis. In one case report, only 1 of 3 patients experienced self-limiting perianal pain and edema after a third embolization (all the branches of the SRAs had been embolized)[10]. This may be a benign manifestation of temporary blood flow redistribution that can be alleviated by the administration of nonsteroidal anti-inflammatory drugs[8,15,21,28]. After confirming the number and shape of the SRA, patients were intervened with different embolization materials and experienced transient complications, including tenesmus (14/15), pain (5/15) and low-grade fever (11/15)[29]. After embolization, 34.4% of patients developed low-grade fever, which is related to the absorption of a gelatin sponge[21]. The incidence of ischemic complications is low. In one case report, ischemic damage and subsequent rectal stenosis occurred in patients who underwent particle embolization[30]. Finally, the patient was successfully treated with 3 endoscopic balloon dilations[30]. Lupattelli et al[31] suggested that particle migration toward a nontarget area may be caused by a large SRA-sigmoid artery anastomosis. Embolization with ethylene vinyl alcohol, a liquid agent, caused focal rectal necrosis, and microparticle embolism resulted in cellulitis in porcine animal models[26].
The reported technical success rates ranged from 90% to 100%, and the clinical success rates ranged from 64% to 93%. However, the definition of clinical success is often vague and thus requires further exploration[32]. Clinical success was defined by Moussa et al[16] as an increase of at least 2 points in the French bleeding score after embolization, with no complications. Afterwards, measures of clinical success included the time limit and visual analogue scale score[5]. Vidal et al[8] defined clinical success as an improvement in symptoms that could not be quantified intuitively. Clinical evaluations included a quality of life assessment, endoscopic findings, histopathological analysis, ultrasound findings, sphincterometry, and anal electromyography[10,16,17,22,29]. However, these self-evaluations are mainly based on hemorrhoidal symptom evaluation, which is not closely related to any clinical findings and presents challenges. Embolization can moderately improve the prolapse score, which can be explained by the decrease in arterial flow after embolization. In addition, surgery is still needed for Grade IV hemorrhoid prolapse[5].
Rectal bleeding can occur immediately after embolization (after a few weeks) or after a certain period of time (after months)[10]. Recurrent rectal bleeding may be associated with incomplete embolization of the superior rectal network[10] caused by unrecognized anatomical variations[8], vascular spasm[16], vascular distortion[33], prior surgery[33], coil recanalization[8], and coagulation disorders[8]. A combination of nitroglycerine, verapamil, and unfractionated heparin was prophylactically administered intraluminal to prevent vasospasm[28]. Tradi et al[5] performed univariate analysis of the influence of various factors on the incidence of recurrence. They reported an association between the appearance of collateral branches of the SRA and recurrence by reperfusion of the corpus cavernosum recti downstream of the coil packing. Re-embolization or even surgery should be considered to achieve hemostasis.
In summary, Emborrhoid is a promising technique for the treatment of bleeding hemorrhoids. Physicians need to carefully evaluate the patient’s condition to choose the appropriate embolization materials and suitable embolization methods. Future randomized controlled trials with greater sample sizes and longer follow-up periods are needed to determine the most appropriate candidate patients, embolization sites, and embolic materials to avoid adverse effects, and a standardized scoring system for hemorrhoidal artery embolization treatment is needed.
| 1. | Tutino R, Stecca T, Farneti F, Massani M, Santoro GA. Transanal eco-Doppler evaluation after hemorrhoidal artery embolization. World J Gastroenterol. 2024;30:2332-2342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (3)] |
| 2. | Hawkins AT, Davis BR, Bhama AR, Fang SH, Dawes AJ, Feingold DL, Lightner AL, Paquette IM; Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Hemorrhoids. Dis Colon Rectum. 2024;67:614-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 3. | Perera N, Liolitsa D, Iype S, Croxford A, Yassin M, Lang P, Ukaegbu O, van Issum C. Phlebotonics for haemorrhoids. Cochrane Database Syst Rev. 2012;CD004322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Gallo G, Martellucci J, Sturiale A, Clerico G, Milito G, Marino F, Cocorullo G, Giordano P, Mistrangelo M, Trompetto M. Consensus statement of the Italian society of colorectal surgery (SICCR): management and treatment of hemorrhoidal disease. Tech Coloproctol. 2020;24:145-164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 168] [Cited by in RCA: 146] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 5. | Tradi F, Louis G, Giorgi R, Mege D, Bartoli JM, Sielezneff I, Vidal V. Embolization of the Superior Rectal Arteries for Hemorrhoidal Disease: Prospective Results in 25 Patients. J Vasc Interv Radiol. 2018;29:884-892.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Falsarella PM, Nasser F, Affonso BB, Galastri FL, Motta-Leal-Filho JMD, Valle LGM, Cunha MJS, Araújo SEA, Garcia RG, Katz M. Embolization of the Superior Rectal Arteries versus Closed Hemorrhoidectomy (Ferguson Technique) in the Treatment of Hemorrhoidal Disease: A Randomized Clinical Trial. J Vasc Interv Radiol. 2023;34:736-744.e1. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Bagla S, Pavidapha A, Lerner J, Kasimcan MO, Piechowiak R, Josovitz K, Marathe A, Isaacson A, Sajan A. Outcomes of Hemorrhoidal Artery Embolization from a Multidisciplinary Outpatient Interventional Center. J Vasc Interv Radiol. 2023;34:745-749. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Vidal V, Sapoval M, Sielezneff Y, De Parades V, Tradi F, Louis G, Bartoli JM, Pellerin O. Emborrhoid: a new concept for the treatment of hemorrhoids with arterial embolization: the first 14 cases. Cardiovasc Intervent Radiol. 2015;38:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Zhou H, Li L, Wang WJ, Li YL. [Clinical analysis of percutaneous superselective superior rectal artery embolization for grades Ⅱ-Ⅲ internal hemorrhoids]. Zhonghua Nei Ke Za Zhi. 2024;63:861-865. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Vidal V, Louis G, Bartoli JM, Sielezneff I. Embolization of the hemorrhoidal arteries (the emborrhoid technique): a new concept and challenge for interventional radiology. Diagn Interv Imaging. 2014;95:307-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Venturini M, De Nardi P, Marra P, Panzeri M, Brembilla G, Morelli F, Melchiorre F, De Cobelli F, Del Maschio A. Embolization of superior rectal arteries for transfusion dependent haemorrhoidal bleeding in severely cardiopathic patients: a new field of application of the "emborrhoid" technique. Tech Coloproctol. 2018;22:453-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Komekami Y, Konishi F, Makita K, Mijin T, Onogawa A, Chochi T, Lee C, Yoshida T, Maeda T, Mitsusada M, Hasegawa S. Rectal arterio-venous malformation (AVM) with bleeding of an internal hemorrhoid. Clin J Gastroenterol. 2016;9:22-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Ma X, Niu T, Peng Y, Xu S. The first case report of rectal artery embolization in the treatment of radiation proctitis. Asian J Surg. 2024;47:1003-1004. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Campennì P, Iezzi R, Marra AA, Posa A, Parello A, Litta F, De Simone V, Ratto C. The Emborrhoid Technique for Treatment of Bleeding Hemorrhoids in Patients with High Surgical Risk. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Ferrer Puchol MD, Esteban Hernández E, Blanco González FJ, Ramiro Gandia R, Solaz Solaz J, Pacheco Usmayo A. Selective intra-arterial embolization to treat hemorrhoids. Radiologia (Engl Ed). 2020;62:313-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Moussa N, Sielezneff I, Sapoval M, Tradi F, Del Giudice C, Fathallah N, Pellerin O, Amouyal G, Pereira H, de Parades V, Vidal V. Embolization of the superior rectal arteries for chronic bleeding due to haemorrhoidal disease. Colorectal Dis. 2017;19:194-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 17. | Iezzi R, Campenni P, Posa A, Parello A, Rodolfino E, Marra AA, Ratto C, Manfredi R. Outpatient Transradial Emborrhoid Technique: A Pilot Study. Cardiovasc Intervent Radiol. 2021;44:1300-1306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Sun X, Bai X, Cheng L, Gu X, Yuan Q, Jing J, Zhang J, Jin Y, Zhou Y, Chen Q. Embolization of the Superior and Inferior Rectal Artery for Chronic Bleeding Caused by Hemorrhoidal Disease: A Case Report. J Vasc Interv Radiol. 2017;28:1753-1756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Sun X, Xu J, Zhang J, Jin Y, Chen Q. Management of rectal bleeding due to internal haemorrhoids with arterial embolisation: a single-centre experience and protocol. Clin Radiol. 2018;73:985.e1-985.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 20. | Moussa N, Bonnet B, Pereira H, Pechmajou L, Pellerin O, Abed A, Del Giudice C, Dean C, Bouda D, de Parades V, Fathallah N, Sapoval M. Mid-Term Results of Superior Rectal Artery and Coils for Hemorrhoidal Embolization with Particles Bleeding. Cardiovasc Intervent Radiol. 2020;43:1062-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 21. | Han X, Xia F, Chen G, Sheng Y, Wang W, Wang Z, Zhao M, Wang X. Superior rectal artery embolization for bleeding internal hemorrhoids. Tech Coloproctol. 2021;25:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Zakharchenko A, Kaitoukov Y, Vinnik Y, Tradi F, Sapoval M, Sielezneff I, Galkin E, Vidal V. Safety and efficacy of superior rectal artery embolization with particles and metallic coils for the treatment of hemorrhoids (Emborrhoid technique). Diagn Interv Imaging. 2016;97:1079-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 23. | Giurazza F, Corvino F, Cavaglià E, Silvestre M, Cangiano G, Amodio F, De Magistris G, Niola R. Emborrhoid in patients with portal hypertension and chronic hemorrhoidal bleeding: preliminary results in five cases with a new coiling release fashion "Spaghetti technique". Radiol Med. 2020;125:1008-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 24. | Wang X, Sheng Y, Wang Z, Wang W, Xia F, Zhao M, Han X. Comparison of different embolic particles for superior rectal arterial embolization of chronic hemorrhoidal bleeding: gelfoam versus microparticle. BMC Gastroenterol. 2021;21:465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Küçükay MB, Küçükay F. Superior Rectal Artery Embolization with Tris-Acryl Gelatin Microspheres: A Randomized Comparison of Particle Size. J Vasc Interv Radiol. 2021;32:819-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Tradi F, Panneau J, Brige P, Mege D, Habert P, Hak JF, Di Bisceglie M, Vidal V. Evaluation of Multiple Embolic Agents for Embolization of the Superior Rectal Artery in an Animal Model. Cardiovasc Intervent Radiol. 2022;45:510-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | De Gregorio MA, Bernal R, Ciampi-Dopazo JJ, Urbano J, Millera A, Guirola JA. Safety and Effectiveness of a New Electrical Detachable Microcoil for Embolization of Hemorrhoidal Disease, November 2020-December 2021: Results of a Prospective Study. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 28. | De Gregorio MA, Guirola JA, Serrano-Casorran C, Urbano J, Gutiérrez C, Gregorio A, Sierre S, Ciampi-Dopazo JJ, Bernal R, Gil I, De Blas I, Sánchez-Ballestín M, Millera A. Catheter-directed hemorrhoidal embolization for rectal bleeding due to hemorrhoids (Goligher grade I-III): prospective outcomes from a Spanish emborrhoid registry. Eur Radiol. 2023;33:8754-8763. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 29. | Luo CS, Jia YP, Mao AW, Yang W. [Preliminavy clinical study of the treatment of hemorrhoids by superselective embolization of superior rectal artery]. Zhonghua Yi Xue Za Zhi. 2017;97:1960-1963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 30. | Eberspacher C, Ficuccilli F, Tessieri L, D'Andrea V, Lauro A, Fralleone L, Mascagni D. Annoyed with Haemorrhoids? Risks of the Emborrhoid Technique. Dig Dis Sci. 2021;66:3725-3729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Lupattelli T. Regarding "Annoyed with Hemorrhoids? Risks of the Emborrhoid Technique". Dig Dis Sci. 2022;67:1423-1425. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 32. | Morsi S, Linares Bolsegui M, Kobeissi H, Ghozy S, Kallmes DF, Kelley SR, Mathis KL, Dozois EJ, Loftus CG, Bendel EC, Vidal V, Thompson SM. Common design and data elements on rectal artery embolization for treatment of symptomatic internal hemorrhoidal disease: an interactive systematic review of clinical trials. CVIR Endovasc. 2024;7:45. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 33. | Ahmed TM, Cowley JB, Robinson G, Hartley JE, Nicholson AA, Lim M, Ettles DF, Monson JR. Long term follow-up of transcatheter coil embolotherapy for major colonic haemorrhage. Colorectal Dis. 2010;12:1013-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | De Nardi P, Maggi G. Embolization of the superior rectal artery: another management option for hemorrhoids. Tech Coloproctol. 2021;25:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 35. | Alves E Sousa F, Lopes PM, Mónica IB, Carvalho AC, Sousa P. Emborrhoid technique performed on a patient with portal hypertension and chronic hemorrhoidal bleeding as a salvage therapy. CVIR Endovasc. 2022;5:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Thompson SM, Kelley SR. Invited Commentary: Rectal Artery Embolization for Treatment of Symptomatic Hemorrhoidal Disease-Opportunity for Multidisciplinary Collaboration. Radiographics. 2022;42:E176-E178. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 37. | Weldon DT, Burke SJ, Sun S, Mimura H, Golzarian J. Interventional management of lower gastrointestinal bleeding. Eur Radiol. 2008;18:857-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 38. | Urbano J, Manuel Cabrera J, Franco A, Alonso-Burgos A. Selective arterial embolization with ethylene-vinyl alcohol copolymer for control of massive lower gastrointestinal bleeding: feasibility and initial experience. J Vasc Interv Radiol. 2014;25:839-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 39. | Jagadeesan BD, Grigoryan M, Hassan AE, Grande AW, Tummala RP. Endovascular balloon-assisted embolization of intracranial and cervical arteriovenous malformations using dual-lumen coaxial balloon microcatheters and Onyx: initial experience. Neurosurgery. 2013;73:ons238-43; discussion ons243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |