Published online Aug 7, 2024. doi: 10.3748/wjg.v30.i29.3534
Revised: May 12, 2024
Accepted: July 18, 2024
Published online: August 7, 2024
Processing time: 111 Days and 21.9 Hours
The role of endoscopy in pathologies of the bile duct and gallbladder has seen notable advancements over the past two decades. With advancements in stent technology, such as the development of lumen-apposing metal stents, and ado
Core Tip: For malignant distal biliary obstruction, endoscopic ultrasound (EUS)-guided choledochoduodenostomy is noninferior to endoscopic retrograde cholangiopancreatography (ERCP) with biliary stent placement, and can be considered as a primary drainage modality instead of a salvage method. In cases with malignant hilar biliary obstruction, combined ERCP with EUS-biliary drainage (CERES), when performed in the appropriate patient, can not only provide bilateral drai
- Citation: Ali FS, Guha S. Defining failure of endoluminal biliary drainage in the era of endoscopic ultrasound and lumen apposing metal stents. World J Gastroenterol 2024; 30(29): 3534-3537
- URL: https://www.wjgnet.com/1007-9327/full/v30/i29/3534.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i29.3534
Biliary interventional endoscopy refers to the ability to treat pathologies of the biliary tract through a non-surgical, endoluminal approach. The availability of fluoroscopy, coupled with endoscopic ability to access the biliary system through the ampulla of Vater, gave rise to the now well-established modality, endoscopic retrograde cholangiopancreatography (ERCP)[1]. As expertise with ERCP grew, our ability to treat and palliate expanded to encompass pathologies of the biliary system which were historically managed with surgery. While this opened new avenues, it also unveiled new challenges that highlighted the need to evolve beyond ERCP through technological innovation and novel thought to address unmet needs of patients with limited options for management of their malady. This milieu led to innovations such as endoscopic ultrasound (EUS) and development of the lumen-apposing metal stent (LAMS), both major milestones which continue to improve our ability to manage biliary pathologies.
Traditionally, failure of endoscopic biliary drainage meant failure of ERCP, subjecting patients to percutaneous biliary drainage (PTBD). Although PTBD is a valuable treatment option, one could argue that it adversely impacts patients’ quality of life due to its external attachments. In the current era, the availability of EUS and LAMS have served to redefine failure of endoscopic biliary drainage, as has been highlighted by Fugazza et al[2], who shed light on the role of EUS-guided biliary drainage (EUS-BD) in the management of gallbladder and biliary tree pathologies.
In malignant distal biliary obstruction (MDBO), EUS-choledocoduodenostomy (EUS-CDS) historically served as a salvage modality in the setting of ERCP failure. This stepwise approach allowed expansion of endoscopic techniques available for biliary decompression in patients with MDBO. As experience with EUS-CDS grew, its technical equivalency to ERCP in the setting of MDBO became evident; EUS-CDS has now been shown to be noninferior to ERCP in the ELEMENT and DRA-MBO clinical trials[3,4], and as such one may perform EUS-CDS as a primary drainage modality in appropriately selected patients. The question of cost-effectiveness of EUS-CDS as a primary drainage modality compared to ERCP in MDBO remains to be answered. In countries where LAMS are unavailable, EUS-BD still serves a useful purpose in the setting of MDBO by providing rendezvous access to allow transpapillary biliary drainage, particularly when MDBO leads to ampullary distortion.
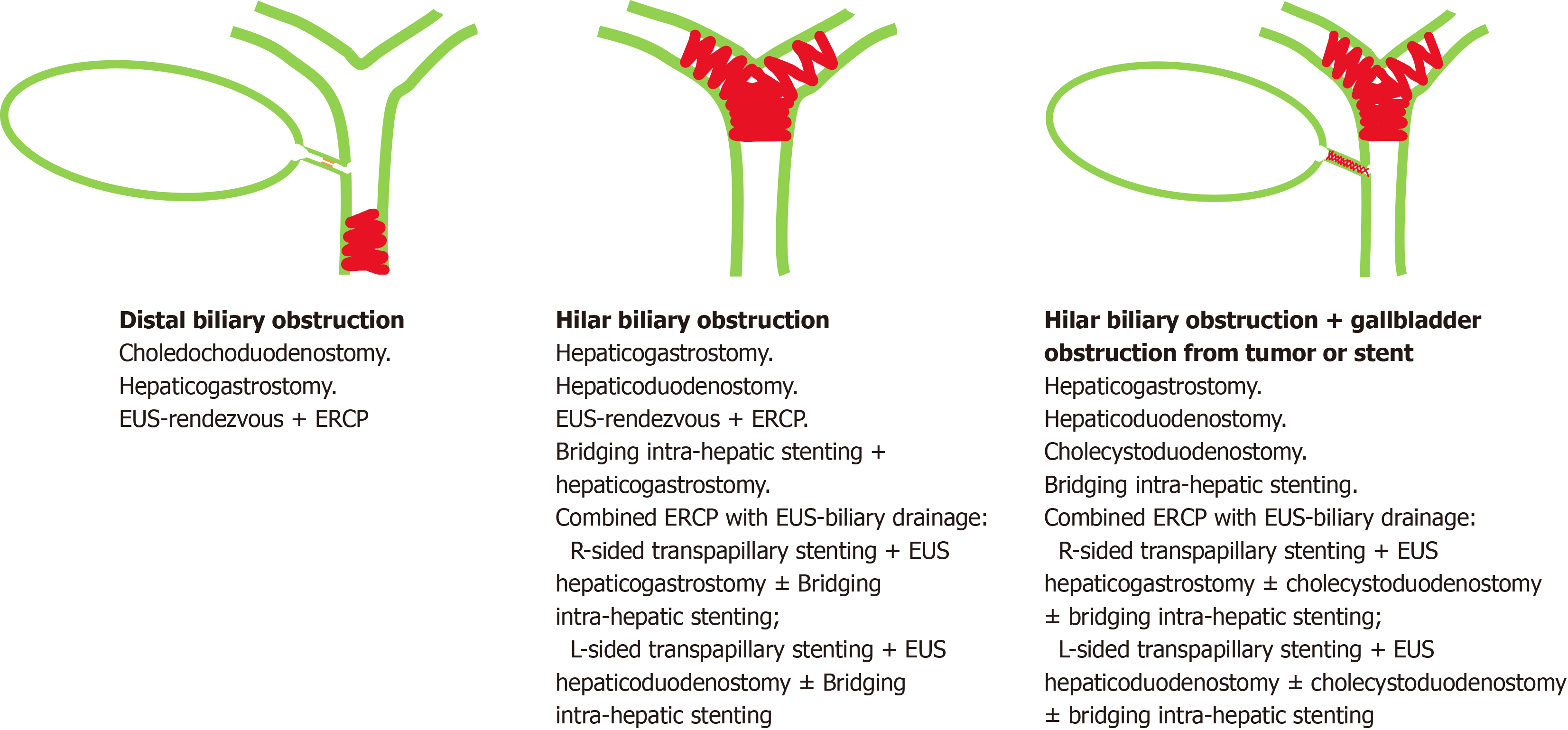
In cases with malignant hilar biliary obstruction (MHBO), EUS-BD can serve as an adjuvant drainage modality that is to be used alongside ERCP; the utility of combined ERCP with EUS-BD (CERES) allows applicability of EUS-BD in multiple configurations (Figure 1)[5,6]. The techniques of EUS-BD studied in the setting of MHBO can serve to prolong the efficacy of endoscopic biliary drainage, potentially delaying PTBD in appropriately selected patients, thereby preserving their quality of life. EUS-BD can also establish bilateral drainage of the liver in cases with high grade MHBO with non-communicating left and right biliary systems by performing bridging intra-hepatic stenting along with a hepa
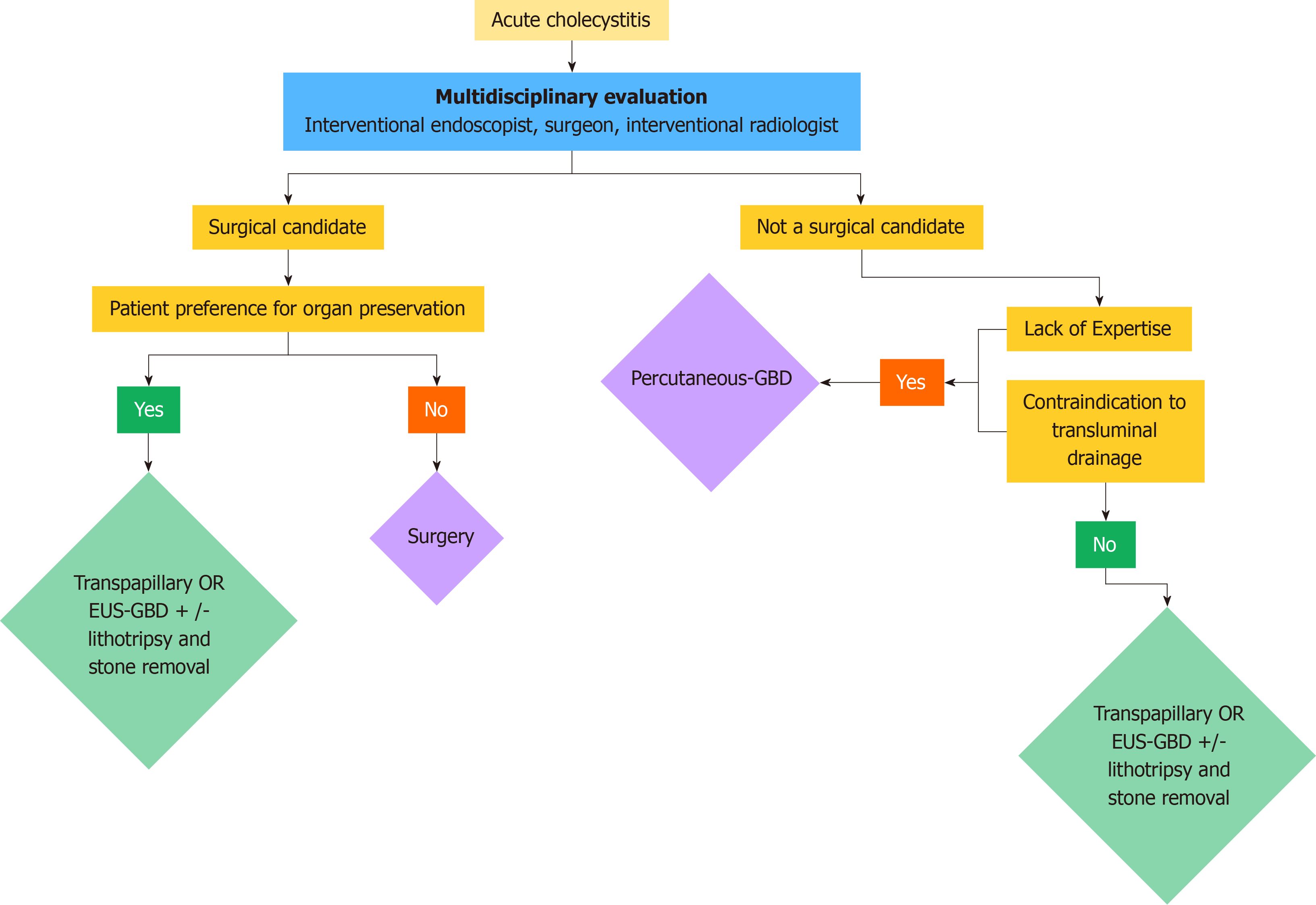
The presence or absence of gallbladder can materially alter the course of management in the setting of biliary obs
As the armamentarium of interventional endoscopy continues to grow, the definition of “failure” as it pertains to the ability to achieve endobiliary drainage will continue to evolve to the point where a majority of patients can be offered one of the many potential therapeutic modalities to achieve adequate biliary drainage, be it through the biliary tree or the gallbladder.
| 1. | Fujita R. The History of ERCP and EUS. In: Mine T, Fujita R. Advanced Therapeutic Endoscopy for Pancreatico-Biliary Diseases. Tokyo: Springer, 2019. |
| 2. | Fugazza A, Khalaf K, Pawlak KM, Spadaccini M, Colombo M, Andreozzi M, Giacchetto M, Carrara S, Ferrari C, Binda C, Mangiavillano B, Anderloni A, Repici A. Use of endoscopic ultrasound-guided gallbladder drainage as a rescue approach in cases of unsuccessful biliary drainage. World J Gastroenterol. 2024;30:70-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (2)] |
| 3. | Chen YI, Sahai A, Donatelli G, Lam E, Forbes N, Mosko J, Paquin SC, Donnellan F, Chatterjee A, Telford J, Miller C, Desilets E, Sandha G, Kenshil S, Mohamed R, May G, Gan I, Barkun J, Calo N, Nawawi A, Friedman G, Cohen A, Maniere T, Chaudhury P, Metrakos P, Zogopoulos G, Bessissow A, Khalil JA, Baffis V, Waschke K, Parent J, Soulellis C, Khashab M, Kunda R, Geraci O, Martel M, Schwartzman K, Fiore JF Jr, Rahme E, Barkun A. Endoscopic Ultrasound-Guided Biliary Drainage of First Intent With a Lumen-Apposing Metal Stent vs Endoscopic Retrograde Cholangiopancreatography in Malignant Distal Biliary Obstruction: A Multicenter Randomized Controlled Study (ELEMENT Trial). Gastroenterology. 2023;165:1249-1261.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 60] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 4. | Teoh AYB, Napoleon B, Kunda R, Arcidiacono PG, Kongkam P, Larghi A, Van der Merwe S, Jacques J, Legros R, Thawee RE, Saxena P, Aerts M, Archibugi L, Chan SM, Fumex F, Kaffes AJ, Ma MTW, Messaoudi N, Rizzatti G, Ng KKC, Ng EKW, Chiu PWY. EUS-Guided Choledocho-duodenostomy Using Lumen Apposing Stent Versus ERCP With Covered Metallic Stents in Patients With Unresectable Malignant Distal Biliary Obstruction: A Multicenter Randomized Controlled Trial (DRA-MBO Trial). Gastroenterology. 2023;165:473-482.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 76] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 5. | Sundaram S, Dhir V. EUS-guided biliary drainage for malignant hilar biliary obstruction: A concise review. Endosc Ultrasound. 2021;10:154-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (2)] |
| 6. | Kongkam P, Tasneem AA, Rerknimitr R. Combination of endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography-guided biliary drainage in malignant hilar biliary obstruction. Dig Endosc. 2019;31 Suppl 1:50-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Nakai Y, Kogure H, Isayama H, Koike K. Endoscopic Ultrasound-Guided Biliary Drainage for Unresectable Hilar Malignant Biliary Obstruction. Clin Endosc. 2019;52:220-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Irani SS, Sharzehi K, Siddiqui UD. AGA Clinical Practice Update on Role of EUS-Guided Gallbladder Drainage in Acute Cholecystitis: Commentary. Clin Gastroenterol Hepatol. 2023;21:1141-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 34] [Reference Citation Analysis (0)] |
| 9. | Quoraishi S, Ahmed J, Ponsford A, Rasheed A. Lessons learnt from a case of extracorporeal shockwave lithotripsy for a residual gallbladder stone. Int J Surg Case Rep. 2017;32:43-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |