Published online Jun 14, 2024. doi: 10.3748/wjg.v30.i22.2834
Revised: April 30, 2024
Accepted: May 20, 2024
Published online: June 14, 2024
Processing time: 87 Days and 21.7 Hours
This editorial is an analysis the review article by Nabi et al recently published in this journal. Achalasia Cardia is a disease whose pathophysiology is still unclear. It is known that there is inflammation of unknown aetiology leading to loss of ganglion cells in the muscularis propria. The end result is lower oesophageal sphincter spasm, loss of receptive relaxation, decreased oesophageal peristalsis, all leading on to varying degrees of dysphagia. The treatment of this condition is palliative in nature, performed by myotomy of the lower oesophagus either surgically or endoscopically. Gastroesophageal reflux disease (GERD) has been associated with the myotomy performed, particularly with the Peroral Endoscopic Myotomy (POEM) procedure. Nabi et al have provided an excellent overview of the latest developments in predicting, preventing, evaluating, and managing GERD subsequent to POEM. Based on this theme, this review article explores the concept of using histology of the oesophageal muscle layer, to grade the disease and thereby help tailoring the length/type of myotomy performed during the POEM procedure. In the future, will a histology based algorithm available preoperatively, help modify the POEM procedure, thereby decreasing the inci
Core Tip: Gastro Esophageal Reflux disease (GERD) is a side effect of the Peroral Endoscopic Myotomy (POEM) procedure done for Achalasia Cardia (AC). There is still lack of clear understanding of the histologic changes associated AC and its correlation with the natural history of the disease. The question put forward in this editorial is whether a histology based algorithm to modify the POEM procedure, will help decrease the incidence of GERD associated with POEM. This article is written to provide a deeper insight into the problem and provide thought for further research on this important, yet unexplored area in the management of AC.
- Citation: Samarasam I, Joel RK, Pulimood AB. Gastroesophageal reflux following per-oral endoscopic myotomy: Can we improve outcomes? World J Gastroenterol 2024; 30(22): 2834-2838
- URL: https://www.wjgnet.com/1007-9327/full/v30/i22/2834.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i22.2834
First described by Inoue et al[1] in 2008, Per-Oral Endoscopic Myotomy (POEM) has been proven to be an effective treatment for Achalasia Cardia. However, the ‘Achilles heel’ of the procedure is the occurrence of Gastro Esophageal Reflux disease (GERD) postoperatively and the solution for this problem has still been elusive. In this current issue of the journal, Nabi et al[2] have presented an excellent overview of the latest developments in predicting, preventing, evaluating, and managing GERD subsequent to POEM. Their review article looks into the various modifications of the POEM procedure and into the future perspectives for improving outcomes in relation to GERD.
Anatomically, there are two factors which are crucial in maintenance of the anti-reflux barrier of the Lower esophageal Sphincter (LES) – firstly, the intrinsic factor consisting of the oblique sling muscle fibres and secondly the extrinsic factor consisting of the phreno-esophageal ligament, which is a membranous ligament between the abdominal esophagus and the diaphragm[3]. A lower oesophageal myotomy done surgically or endoscopically has the potential to adversely affect one or both of these barrier mechanisms.
The original surgical Heller’s myotomy was a double-sided myotomy, by a transthoracic approach. This was later modified by Zaaijer[4], into a single-sided thoracic myotomy[4]. An anti-reflux procedure (fundoplication) was not part of these original procedures. The inherent problem with the thoracic approach was the inability to perform an adequate myotomy on the stomach side. This therefore resulted in suboptimal dysphagia relief. Therefore, the abdominal approach was improvised, to address this issue and subsequently Laparoscopic Heller’s myotomy (LHM) became the gold standard in the surgical management. When the myotomy was performed transabdominally, the dysphagia relief was much better, but GERD was inevitable as both the intrinsic and extrinsic anti-reflux barriers were at risk. However, the solution to this problem was relatively easy, by the way of addition of an anti-reflux procedure in the form of a fundoplication[5]. An anterior (Dor) fundoplication or a posterior partial (Toupet) fundoplication were added as an additional procedure to LHM. Thus, the current surgical guidelines clearly mention that LHM with fundoplication is superior to LHM without fundoplication in controlling distal oesophageal acid exposure[6].
What has changed with the advent of POEM? Although the approach of the POEM is different (being an endoscopic procedure), the principles of surgical myotomy remains the same. Since POEM is an endoscopic procedure, the extrinsic anti-reflux barrier is less affected, but the intrinsic anti-reflux barriers are compromised, resulting in the GERD. The addition of an anti-reflux procedure endoscopically as in the NOTES-F procedure is much more technically demanding when compared to the LHM. Although shown to be feasible, this modification of the NOTES procedure requires quite advanced endoscopic skills and its safety, efficacy and durability of the wrap are yet to be proven[7,8].
The EndoFLIP seems to be an attractive option to assess intraoperative LES distensibility during POEM, thereby enabling the tailoring of myotomies, with a view to possibly decrease the risk of postoperative reflux. The short term outcomes of this procedure have been looked at and have been favourable[9]. However, the available literature on the intraoperative use of EndoFLIP during POEM is still scanty and the procedure still under evolution.
The review article in this journal by Nabi et al[2], details the pros and cons of the various techniques of modification of the standard POEM procedure. The modifications focus on the location and length of the oesophageal and gastric myotomies and the techniques which allow preservation of the sling fibres of the Esophago-gastric junction (EGJ). However as mentioned in the article, the results of these techniques have not been consistent, with studies showing contrasting outcomes. Perhaps of the reasons for this paradox might lie in the fact patients with AC present at different stages of the evolution of the disease. Therefore a ‘one size fits all’ option may not be suitable for all patients with AC and a more personalised approach may be the way forward. Are there unexplored options available, to modify the POEM procedure and tailor it to every patient?
There have been significant advances in the techniques of management of AC, but there is still lack of clear understanding of the histologic changes that are associated with the condition and the correlation with the natural history of the disease. Histologic examination of the oesophageal mucosal specimens obtained at esophagectomy have shown lymphocytic infiltration, muscle hypertrophy, interstitial fibrosis, ganglion cell loss, ganglionitis[10,11]. The study by Sodikoff et al[12] looked at surgically obtained muscularis propria biopsy specimens from patients with achalasia cardia. The spectrum of histopathologic findings included complete aganglionosis, lymphocytic inflammation, to almost normal histopathology[12]. This again underlines the fact that patients with AC represent a pathogenically heterogeneous group, with symptoms of EGJ outflow obstruction.
We have conducted a prospective observational study in our centre, involving 21 patients who underwent LHM for AC (unpublished data). The study included taking two small bits (0.5 cm × 0.5 cm each) of oesophageal muscle from the cut ends of the myotomy at the lower esophageal muscle layer and the GEJ. Histopathological, immunohistochemical and ultrastructural analysis was performed. These pathology results were correlated with the clinical features, manometric features and post-operative outcomes. Post-operatively, these patients were monitored till discharge and followed up at 1 month, 3 months and 6 months in the surgery OPD. The short term surgical outcomes including complications and relief of dysphagia were recorded.
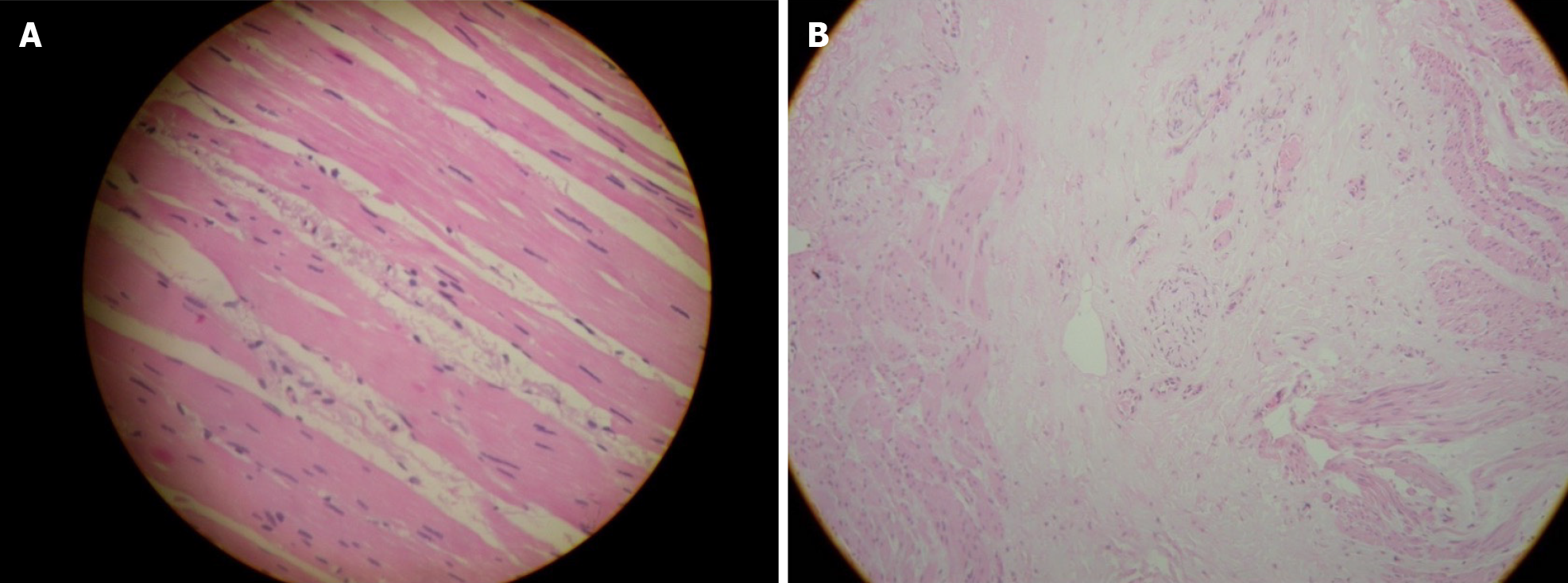
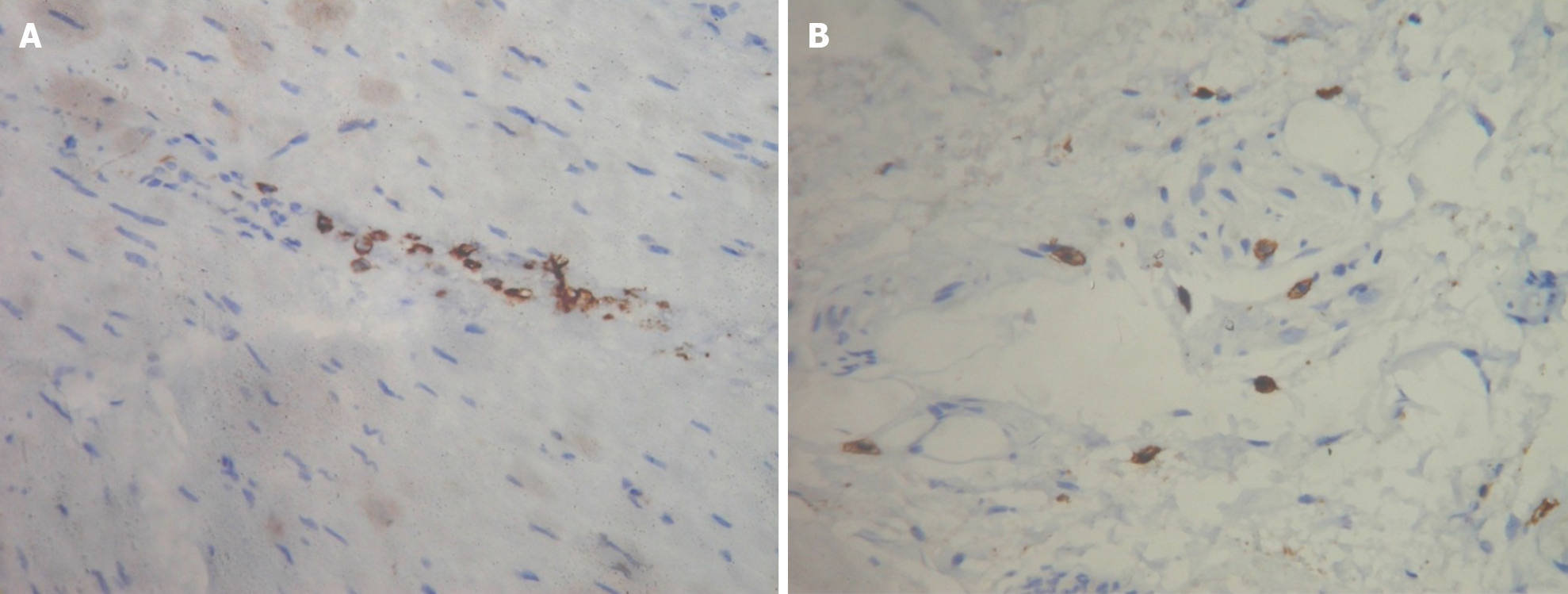
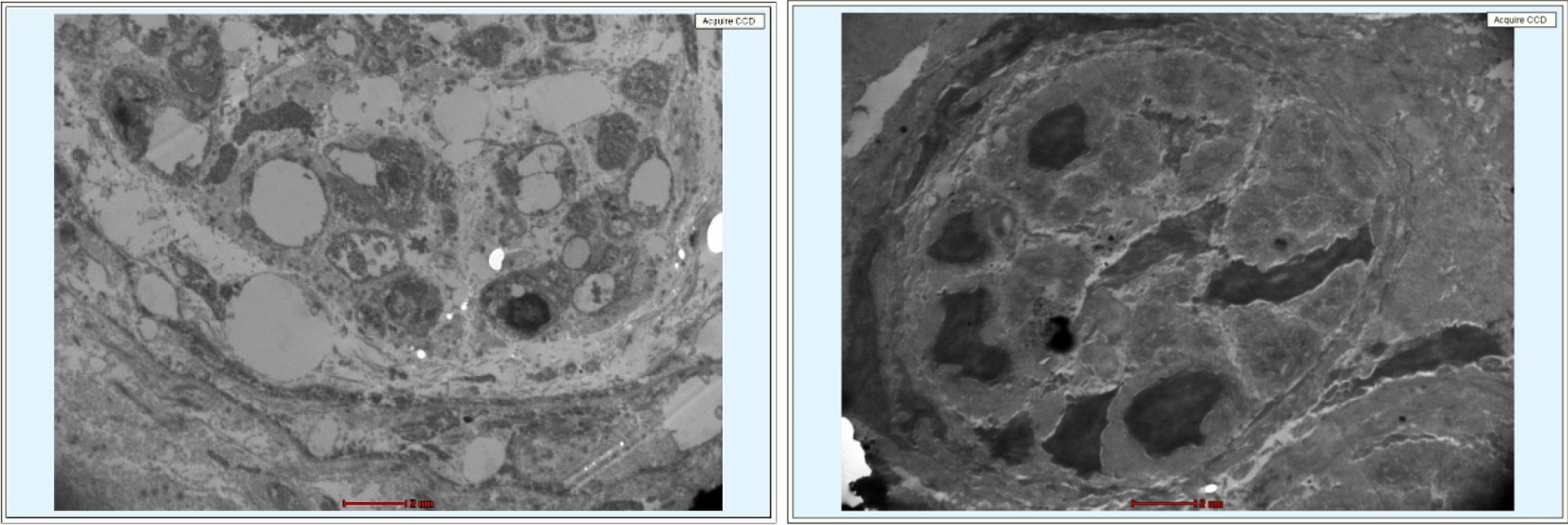
Specimens were graded on degree of neuronal loss, muscular damage, inflammation, and fibrosis. The spectrum of fibrosis and smooth muscle atrophy ranged mild to severe (Figure 1). The histology also demonstrated eosinophil and mast cell infiltration, indicating inflammation of the myentric plexus (Figure 2). Damage and demyelination of ganglion cells was a consistent finding (Figure 3). These histological changes were dependent on the disease duration, lower oesophageal sphincter dysfunction, degree of esophageal dilatation and the manometric subtype. The study also showed histologic changes starting with myenteric inflammation, and damage to the ganglion cells and neuronal fibrosis (early disease). This then progresses to total absence of ganglion cells (aganglionosis), severe fibrosis and varying degrees of smooth muscle atrophy/hypertrophy (late disease).
Liu et al[13] have described the Histologic Findings in Mucosa and Muscularis Propria Biopsied during POEM, in patients with AC. The study has described the feasibility and safety of muscle biopsy during POEM. Again, there was again varying degrees of inflammation, neuronal loss, muscle fibrosis and atrophy the specimens examined[13].
Now that the safety of muscle biopsies during LHM/POEM procedures have been demonstrated, what we need are larger multicentre studies which can help grade the histological changes - namely ganglion loss, inflammation, muscle loss/hypertrophy and fibrosis. When the histologic pattern is available preoperatively, the POEM or the LHM procedure can be modified based on the severity of the disease and the symptom palliation required. For example, in a patient with early disease and lesser fibrosis, dysphagia relief may be obtained by even shorter myotomies, thereby offering protection against future GERD. Whereas in a patient with end stage disease with severe aganglionosis and muscle atrophy/fibrosis, the focus of treatment must be to provide the maximum possible dysphagia relief and the side effect of GERD may be of secondary importance.
Will a pre operative, histology based algorithm help tailor the length/type of myotomy performed during POEM/LHM procedures, thereby minimising post procedural GERD? We leave this question in the minds of the readers of this article and hope this will provide fuel for further research on this important, yet unexplored area in the management of AC. This, along with the intraoperative use of EndoFLIP may offer a reasonable solution to the long debated issue of reflux following POEM.
| 1. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1234] [Article Influence: 82.3] [Reference Citation Analysis (1)] |
| 2. | Nabi Z, Inavolu P, Duvvuru NR. Prediction, prevention and management of gastroesophageal reflux after per-oral endoscopic myotomy: An update. World J Gastroenterol. 2024;30:1096-1107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Reference Citation Analysis (3)] |
| 3. | Andreollo NA, Earlam RJ. Heller's myotomy for achalasia: is an added anti-reflux procedure necessary? Br J Surg. 1987;74:765-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 89] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Zaaijer JH. Cardiospasm in the aged. Ann Surg. 1923;77:615-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 125] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 5. | Ellis F, Cole FL. Reflux after cardiomyotomy. Gut. 1965;6:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol. 2020;115:1393-1411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 238] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 7. | Bapaye A, Dashatwar P, Dharamsi S, Pujari R, Gadhikar H. Single-session endoscopic fundoplication after peroral endoscopic myotomy (POEM+F) for prevention of post gastroesophageal reflux - 1-year follow-up study. Endoscopy. 2021;53:1114-1121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 8. | Mandavdhare HS, Samanta J, Varma P, Praveen Kumar-M, Gupta P, Singh H, Dutta U, Kochhar R. Per oral endoscopic myotomy with fundoplication is a technically feasible NOTES for achalasia cardia. Minim Invasive Ther Allied Technol. 2022;31:319-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Knight W, Kandiah K, Vrakopoulou Z, White A, Barbieri L, Tewari N, Couch J, DiMaggio F, Barley M, Ragunath K, Catton J, Botha A. Early outcomes following EndoFLIP-tailored peroral endoscopic myotomy (POEM): the establishment of POEM services in two UK centers. Dis Esophagus. 2023;36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Goldblum JR, Whyte RI, Orringer MB, Appelman HD. Achalasia. A morphologic study of 42 resected specimens. Am J Surg Pathol. 1994;18:327-337. [PubMed] |
| 11. | Gockel I, Bohl JR, Doostkam S, Eckardt VF, Junginger T. Spectrum of histopathologic findings in patients with achalasia reflects different etiologies. J Gastroenterol Hepatol. 2006;21:727-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Sodikoff JB, Lo AA, Shetuni BB, Kahrilas PJ, Yang GY, Pandolfino JE. Histopathologic patterns among achalasia subtypes. Neurogastroenterol Motil. 2016;28:139-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 90] [Article Influence: 10.0] [Reference Citation Analysis (1)] |
| 13. | Liu X, Kuo E, Wang K, Perbtani YB, Yang D, Draganov P. Histologic Findings in Mucosa and Muscularis Propria Biopsied During Peroral Endoscopic Myotomy in Patients With Achalasia. Gastroenterology Res. 2021;14:281-289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |